
Protecting Non-communicable Diseases Patients during Pandemics:
Fundamental Rules for Engagement and the Case of Lebanon
Luna El Bizri
a
and Nabil Georges Badr
b
Higher Institute of Public Health, Saint Joseph University, Beirut, Lebanon
Keywords: Non-Communicable Diseases, Patient Journey, Digital Health, Universal Health Coverage, COVID-19,
Lebanon, Sendai Framework, Disasters.
Abstract: Non-communicable diseases (NCDs) are still the number one killer in the world. Their economic burden is
heavy, notably in low-and-middle-income countries. Lebanon is a middle-income country in the Eastern
Mediterranean region. The arising COVID-19 pandemic, political and economic instability, inadequate
funding, and deteriorated infrastructure have rendered the country a fragile setting, significantly affecting
persons with non-communicable diseases. Improving the patient journey during the COVID-19 pandemic and
a comprehensive approach to NCD management is important during emergencies.This paper used a quantitate
literature review to provide a theoretical framework touching NCDs patients in their journey during
emergencies and crisis. It further adopted the Sendai Framework to draw the road for these patients in
Lebanon. The ultimate goal is better preparedness and response in case of emergencies and disasters. It calls
for a clear and coordinated action plan addressing the challenges posed by NCDs to a resilient country's
response. This paper provides an overview of the situation of NCD patients in Lebanon during the COVID-
19 pandemic. It suggests strategies to address non- communicable diseases guided by the Sendai Framework's
four priorities, based on previous experiences.
1
INTRODUCTION
Non-communicable diseases (NCDs) kill 41 million
people each year, equivalent to 71% of all deaths
globally
1
. The World Health Organization (WHO)
reports that each year, more than 15 million people die
from a NCD between the ages of 30 and 69 years;
85% of these premature deaths occur in low- and
middle-income countries. Non- communicable
diseases such as cardiovascular diseases account for
most NCD deaths, or 17.9 million people annually,
followed by cancer (9.3 million), respiratory disease
(4.1 million), and diabetes (1.5 million).
The COVID -19 pandemic has accentuated the
vulnerability of NCD patients and weakened that
resilience of the public health system. Diabetes,
hypertension, and cholesterol levels are among the
comorbidity factors that increase the severity of
a
https://orcid.org/0000-0001-9317-2132
b
https://orcid.org/0000-0001-7110-3718
1
https://www.who.int/news-room/fact-
sheets/detail/noncommu nicable-diseases
COVID-19 infection (Zaki et al, 2020), placing a
higher risk (Chan et al, 2020) on NCD patients. This
risk increase with the lack of appropriate care due to
the sudden shift in priorities of the healthcare system
and providers, infrastructure disruption, degraded
living conditions, inability to operate safely and offer
quality care to all patients. Evidently, NCD diagnosis
and treatment services were partially or completely
disrupted worldwide - Hypertension (-50% decrease),
cancer treatment (-45%), and cardiovascular
emergencies (-30%)
2
.
The patient journey for NCDs is depicted in five
broad touchpoints: awareness, screening, diagnosis,
treatment, and adherence with integration of
palliative care along the care continuum pathway (Fig
1.). These phases require the development of
interventions and policies tailored to the patient’s
need at these different phases (Devi et al, 2020),
which, if disrupted may be fatal to the patients, or
2
NCD department (May 2020): final results: rapid
assessment for NCDs during the COVID-19 pandemic.
WHO (2020). The impact of the COVID-19 pandemic
on non-communicable disease resources and services:
results of a rapid assessment.
306
El Bizri, L. and Badr, N.
Protecting Non-communicable Diseases Patients during Pandemics: Fundamental Rules for Engagement and the Case of Lebanon.
DOI: 10.5220/0010742300003123
In Proceedings of the 15th International Joint Conference on Biomedical Engineering Systems and Technologies (BIOSTEC 2022) - Volume 5: HEALTHINF, pages 306-315
ISBN: 978-989-758-552-4; ISSN: 2184-4305
Copyright
c
2022 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved

introduce risks that yield to an unpredictable
outcome. Essentially, the COVID-19 and NCD
pandemics exert a combined effect, leaving NCD
patients at a higher risk of developing severe COVID-
19 complications, and more likely to develop long-
term chronic conditions (Nassereddine, 2021).
Figure 1: Key Stages - NCD patient journey (adapted from
Devi et al, 2020).
1.1 Motivation
The context of our paper is the country of Lebanon.
A middle-income country located in the Eastern
Mediterranean region, where NCDs account for
approximately 91% of all deaths
3
. The economic
growth was slowing since 2011, following the Arab
Springs, and the influx of 1.5 million Syrian refugees
to Lebanon, abruptly raising the population by 25%.
Syrian refugees live in close contact with the host
community, and their living conditions are favourable
for the epidemic spread to the Lebanese public at
large. Inadequate access to health care, and
inadequate community awareness levels are
vulnerability factors. The relatively high prevalence
of non-communicable diseases in this population
could also affect the severity of the disease among
those infected. Poverty, stigma, and fear of legal
consequences are contextual factors that further
exacerbate this vulnerability (Fouad, 2021).
Adding to the already failing health sector, the
disruptions of the COVID-19 pandemic, and the
stressful economic situation, was a massive explosion
in Beirut that rendered three major hospitals
3
www.who.int/nmh/countries/lbn_en.pdf.
4
https://www.who.int/publications-detail-
redirect/9789240029682
inoperable, and other hospitals severely damaged,
with more than 300,000 people left without shelter.
Consequently, there was a significant decrease in
scheduled mammograms, screening colonoscopies,
and elective surgeries and follow-up visits. This led
to delay in diagnoses or treatments in chronically ill
and cancer patients (El Karak, 2021). In fact, 29% of
NCD patients had interrupted or rationed their
medication before the explosion due to financial
problems and medicine shortage (Medecins sans
frontieres, 2021).
Components of health ecosystems, encompassing
collaborations between health and other sectors must
work in synergy to meet the demands imposed by
health emergencies
4
. Targeted investments and policy
reforms in building the capacity of health systems to
effectively manage routine demands can help
countries strengthen the effectiveness and coverage
of routine health care provision for NCD during
pandemics (Rentschler, 2021) and strengthen the
resilience of health systems to shocks and pressures.
The Ministry of Public Health (MoPH) have not been
able to meet the challenges, albeit having developed
the national NCD prevention and control plan (NCD-
PCP) back in 2016
5
.
With this work, we intend to summarize
Lebanon’s response to the pandemic and the
disruption of the NCD journey. Then, using guidance
from the extant literature, we outline a call to action
for the Lebanese communities that draw attention to
the case of NCD patients during a Pandemic.
Therefore, we try to answer the question What does
the literature recommend as principle strategies that
would help address the needs of NCD patients during
a pandemic emergency?
2
APPROACH
This effort was conducted between March 2021 and
August 2021, completing a literature search to
identify articles within the scope of the NCD journey
in Lebanon during the COVID Pandemic. The search
included databases such as PubMed, and Google
Scholar to look for papers that cover all three contexts
and published during and after the year of the
COVID-19 pandemic. Searches included keywords
such as "COVID-19" AND "Lebanon" AND "Non
communicable Diseases" to yield 101 papers;
5
https://www.moph.gov.lb/en/DynamicPages/index/2/
3687/non-%20communicable-diseases#/en/view/3691/
non-communicable-dis eases-prevention-and-control-plan-
ncd-pcp-lebanon-2016-2020.
Protecting Non-communicable Diseases Patients during Pandemics: Fundamental Rules for Engagement and the Case of Lebanon
307

"COVID-19" AND "Lebanon" AND "Non
communicable Disease", to produce 326 papers and,
"COVID-19" AND "Lebanon" AND "NCD", to
identify 118 sources. Papers eligible for review
included research studies, review articles, policy
papers, opinion articles, and legal briefs. There were
no limitations in term of times and languages. In
parallel we retrieve secondary sources of data: the
first author includes media stories and articles, blog
postings, and magazine articles from the grey
literature in the study (e.g., secondary sources from the
Ministry of Public Health - MoPH), only when
necessary to bridge the information gap in the
literature and triangulate authors concepts. Both
authors reduced the duplicate articles and review them
independently. After isolating 68 articles, they read
them in full, then checked for relevance, rejecting
patents and citations and restricting the review to
papers relevant to the study, which resulted in the
retention of 46 articles. That is, authors have found a
few entries in the literature discussing the Lebanon
context in general (23 papers). Citing Lebanon
example, sixteen articles were found to address NCD
in Emergencies (Covid-19 Pandemic specifically).
Others covered disaster risk reduction (DRR),
Universal Healthcare (UHC), and the NCD journey in
low and medium-income countries (LMIC) inferring
to the Lebanese context (seven publications). Next,
both authors proceeded with the paper to synthesize
the findings. Two steps were followed: First, a
summary of Lebanon’s reaction to the pandemic and
the NCD Population was produced (section 3.1). As a
second step, the authors identified components of
Health EDRM and SENDAI Priorities for Action to
provide a basis for a roadmap to strengthening the
resilience of health systems (Aitsi- Selmi et al, 2015)
and connect the recommendations from EDRM and
Sendai in the context of the NCD journey to
summarize a call to action in the Lebanese context
(section 3.2). Therefore, using these frameworks as a
backdrop to our paper, we pave the way to learn from
the extant literature and augment actionable examples
into these frameworks that would contextually apply
to the Lebanese case. We explicate the frameworks’
prescriptive nature to connect it to the NCD patient
journey. We identify gaps in the Lebanese handling
of the NCD journey and develop calls to action based
on the frameworks for (section 3.2.). Therefore, we
propose a vision under the guidelines of these
frameworks to shift focus from disaster response to
fundamentals of planning and preparedness. This new
lens may be helpful to focus the frameworks on
6
https://datareportal.com/reports/digital-2020-lebanon
addressing the risks of NCD in a pandemic (Hung et
al, 2021). In a contextual framework, we try to
compensate for the lack of evidence by suggesting
priorities for action that map to the NCD patient
journey. Then, we aim to use learnings from the
extant literature, raise public awareness, and provide
guidance from DRR frameworks (Health EDRM,
SENDAI).
3
PERSPECTIVES FROM THE
LITERATURE
COVID-19 response in Lebanon was meager,
burdened by compromised healthcare systems,
prolonged political unrest, conflict, and humanitarian
crisis, poor vital registration systems, suboptimal
reporting, and dearth of publicly available data
(Nassereddine, 2021). To set the stage for our work in
this paper and after consulting a few documents and
materials from the MoPH, we summarize the
response as follows:
At the onset of the COVID-19 pandemic (Jan
2020), Lebanon saw an increase of 6.8% of social
media compared to April 2019, and 68% of the total
population were using mobile Apps
6
. The MoPH set
up COVID-19 dashboards, for information diffusion
and provisioned resources for collecting information
required to guide all aspects of the operations
7
. That
included communications, risk and needs assessment,
priority setting, planning, information management,
health operations, and health logistics. Formalizing
their pandemic response, the MoPH put in place a
regional preparedness and response plan for COVID-
19, developed to establish a national plan of action to
scale up preparedness and response capacities in
Lebanon for prevention, early detection, and rapid
response to coronavirus disease 2019. The plan called
for screening at Points of Entry (POE) of coming from
outbreak countries, provision of PPEs at the health
facility level, the designation of additional referral
hospitals national coordination mechanisms, and
assessment of capacities and gaps for potential local
spread and outbreak.
Lebanon has managed to control the virus spread
through an initial strict lockdown and confinement
measures amid an already struggling economy (Fouad
et al, 2021). Nevertheless, the healthcare system has
been seriously affected and, the scarce resources have
been diverted from the primary healthcare centres
(PHCs) supported by the government to the COVID-
7
https://covid19.mohp.gov.np/
HEALTHINF 2022 - 15th International Conference on Health Informatics
308

19 emergency systems. The result was the interruption
of the provision of basic services such as procurement
of vaccines, chronic and essential medicines (Rosita di
Peri et al, 2020; Hamadeh et al, 2021).
3.1 Lebanon’s Reaction to the
Pandemic and the NCD Journey
Only a handful of publications studied and reported
the impact of the pandemic on the NCD patient
journey in Lebanon. Namely, Hamadeh et al (2020),
discuss the low level of readiness of the Lebanese
primary healthcare centres during the COVID-19
pandemic to address non-pandemic related diseases.
During COVID-19, visits to primary healthcare
centers (PHCs) waned to a minimum, and access to
essential chronic health services was interrupted.
Visits to PHCs for essential services declined by up
to 70%. As a result, the most vulnerable NCD
population was more likely to defer and postpone
care until their condition becomes critical, most
often requiring hospitalization (Hamadeh et al,
2021). Elsewhere, Zablith et al (2021) document the
complex dynamics of NCD management worsened
by lack of governance, the scarcity of financial and
human resources, perceptions of care quality, and
community trust in services. The COVID-19
pandemic dealt a heavy blow to the country’s health-
care system that has been buckling under
consecutive politico-economic and security events
(Zablith et al, 2021). Karak et al (2021) explain the
disruption in terms of lack of rapid access to
medications and the need for dedicated care centres
for cancer patients to ensure continued treatment and
care.
Whilst, touching on the digitalization of mental
health services, Fouad et al (2021a) described how
Tele-mental health was introduced as a viable
solution in times of pandemic especially in low-
income settings. The delay in diagnosis and early
treatment has a relevant impact and subsequently
increases the burden of NCDs. Teleconsultation had
become the norm for both Lebanese and Syrian
populations as less and less direct in-person services
and resources were available (Saleh et al, 2018). The
majority of Lebanese physicians increased their use
of WhatsApp (80%), phone calls (67%), and email
(63%) for their telehealth activities. These activities
include reading test results, discussing the patient's
case, prescribing medication, and providing public
awareness (Helou et al, 2020). The burden of the
pandemic had its toll on the NCD journey at all
stages (Table 1).
Table 1: NCD Journey in Lebanon – During COVID – 19.
Key Stages - NCD in Lebanon, during COVID – 19
Awareness
MOPH - WhatsApp and Facebook broadcast educational videos
(Sacca et al, 2020); Individual initiative – APP for weight control
and fitness (Bardus et al, 2019); breast cancer awareness (Sacca et
al, 2020);
Screening
Access to information for screening via mobile devices (Manca,
2015) and EMR systems (Saleh et al. 2018). Tele-mental health a
viable solution (Fouad et al, 2021a)
Diagnosis
Physicians relied on telehealth activities for diagnosis and
treatment (Helou et al, 2020); Teleconsultation had become norm
in both the Lebanese and Syrian populations as less and less direct
in person services and resources were available (Saleh et al, 2018).
Treatment
Physicians relied on telehealth activities for diagnosis and
treatment (Helou et al, 2020); lack of rapid access to medications
and care center resources (Karak et al, 2021); Low level of
readiness of the Lebanese primary healthcare centres (Hamadeh et
al, 2020)
Adherence
Lack of interoperability between healthcare stakeholders’ systems
(FIP, 2019). Lack of rapid access to medications and care center
resources (Karak et al, 2021); Learn new supply chain and/or
dispensing approaches for NCD medicines (Khoury, 2020); most
vulnerable NCD population likely to defer and postpone care
(Hamadeh et al, 2021)
Awareness - As the MoPH and the health
ecosystem in the country reacted to the pandemic, the
NCD population was left unattended, served only by
a few individual initiatives, trying to close the gap in
awareness and self-care interventions in NCD
patients through the promotion of training and
education. WhatsApp and Facebook broadcast
educational videos raising cancer awareness and the
importance of screening (Sacca et al, 2020). By
individual initiative, community members have
developed applications to help weight control
application - WaznApp (Bardus et al, 2019), help
individuals achieve their fitness goals
8
and raising
breast cancer awareness and the importance of
screening (Sacca et al, 2020).
Exceptionally, in this case, to curb the mental
health issues that resulted from the pandemic, the
MoPH developed an extension to the plan that aimed
at comprehensively addressing the mental health and
psychosocial support (MHPSS) aspects of the
COVID-19 outbreak in the country, including
Protecting Non-communicable Diseases Patients during Pandemics: Fundamental Rules for Engagement and the Case of Lebanon
309

Palestinian and Syrians refugees
8
. Components of this
action plan were to: (1) Promote mental health and
mitigate COVID-19 related stressors; (2) Support to
the quarantined; caregivers, first responders, and
mental health patients. However, the plan did not
include special provisions for resources to maintain
the services for the non- pandemic related chronic
diseases. The action plan mainly focused on multiple
scenarios for strengthening surveillance and response
to COVID-19 and missed the requirements of the
primary healthcare activities regarding the vulnerable
NCD populations' needs; dynamics of NCD
management were worsened by lack of governance,
scarcity of financial and human resources,
perceptions of care quality, and shaken community
trust (Zablith et al, 2021).
Screening and Diagnosis - Telehealth activities
took to the mainstream. These activities include
reading test results, discussing the patient's case,
prescribing medication, and providing public
awareness (Helou et al, 2020). Almost half of the
Syrian households have a member with an NCD
(Sethi et al, 2017). Over 90% of Syrian refugees’
households in Lebanon have access to a mobile phone
and use it widely (Manca, 2015). A cloud-based EHR
system (Sijilli) – meaning "my record" in Arabic,
launched in 2018 to gather and maintain medical data
for displaced Syrian refugees – which became an
essential source of information to care for the needs
of the refugees during the pandemic – some of which
were NCD patients. Another project (the e-Sahha
project) offered the Palestinian refugees the facility to
capture information on diabetic and hypertensive care
seekers. The project included a weekly diffusion of
personalized, educational text messages, providing
health information on lifestyle, dietary habits, body
weight, smoking, medications, and symptoms of
hypertension and diabetes (Saleh, S. et al. 2018).
Treatment - Lebanese primary healthcare centres
were taken by surprise, as the COVID-19 pandemic
came to exacerbate the already stressed systems
(Hamadeh et al, 2020). NCD patients tended to defer
and care, at the risk of complications (Hamadeh et al,
2021), before admission to care centres, that
dedicated their resources to address COVID-19
patients. Some instances spawned the need for
dedicated care centres to treat cancer patients and
ensure their continuum of care (Karak et al, 2021).
8
MoPH Action Plan MHPSS response to the COVID-19
outbreak in Lebanon-V1.0 (2020, March).
Adherence - In Lebanon, the lack of
interoperability between different healthcare
stakeholders’ systems is a major concern (FIP, 2019).
Barriers are multiple: finding "common languages"
between medical records in different hospitals, a
significant cost of implementation, ensuring patients’
confidentiality, and care coordination between
different healthcare providers. NCD patients had to
learn new ways to manage their care, and their
caregivers were pushed to adopt telemedicine, learn
new supply chain and/or dispensing approaches for
NCD medicines, adapt new triaging protocols to
identify priorities and to care for the most vulnerable,
and often redirect their NCDs to alternate health care
facilities (Khoury, 2020).
In sum, from the initial stages of awareness,
prevention, and screening to the subsequent stages of
diagnosis and treatment and ongoing management,
the NCD population fought hard to gain access to
proper care. NCD patients had to learn new ways to
manage their care, and their caregivers were pushed
to adopt telemedicine, learn new supply chain and/or
dispensing approaches for NCD medicines, adapt new
triaging protocols to identify priorities and to care
for the most vulnerable, and often redirect their NCDs
to alternate health care facilities (Khoury, 2020). It
was not until a year later, in February 2021, when the
vaccination campaign took hold that the NCD
population received some attention. NCD patients
took "high priority".
3.2 Preparing the NCD Patient
Journey for Disaster Resilience
We start the conversation about disaster risk
reduction by referencing the Health Emergency and
Disaster Risk Management (EDRM) Framework,
published in 2019 by the WHO. The EDRM
framework prescribes fundamental components and
an approach for all actors in health and other sectors
who are working to reduce health risks and
consequences of emergencies and disasters (Hung et
al, 2021). Extended from the UN Sendai Framework
for Disaster Risk Reduction 2015–2030, the EDRM
places human health at the centre of disaster risk
reduction. The Sendai Framework stipulates that the
disaster management cycle is a continuing process
with three ultimate goals: mitigating the present
disaster effects, achieving a rapid and effective
recovery, and acting during the post-disaster phase
(Bullock et al, 2013). Disaster planners draw the
HEALTHINF 2022 - 15th International Conference on Health Informatics
310
roadmap for strengthening the resilience of their
health systems, while relying on the effective
implementation of such framework, which require
local, national, regional, and global actions and
cooperation between all stakeholders (Aitsi-Selmi et
al, 2015). A clear and coordinated action plan
addressing the challenges faced by NCD patients
before, during, and after disasters will help to mitigate
the heightened burden of risks, especially in the
context of low and middle- income countries
(LMICs) and among their vulnerable populations
(Gnanapragasam et al, 2016). Moreover, in 2018, the
WHO issued guidance on integrating NCD
management in emergency response preparedness
(ERP) plans
9
. In the preparedness phase, the guidance
emphasized the identification of priority conditions
for inclusion in emergency response that outline the
pre-emergency profile of NCDs and assess the
readiness of the concerned Health Facilities.
Coordination plans would be put in place for
contingencies, with individualized emergency plans,
ensuring the availability of resources, essential
medicines, and technologies. At the onset of the
emergency, coined as the emergency response phase,
the WHO working groups propose integrating NCDs
in initial rapid assessments, mapping the service
provisioned, and organizing the service delivery that
focuses on their care. Finally, a post-emergency phase
is recommended to debrief on lessons learned from
the crises, strengthen health ecosystem response to
the needs of NCD patients with a continuous loop of
monitoring and evaluation. In Table 2, we adapt the
works of Bullock et al, (2013) et Hung et al (2021), to
frame the EDRM context and the priorities for action
of Sendai Framework and provide insight into the
activities required in the NCD patient journey, during
an active disaster.
As a first priority, it is vital to enhance risk
governance and better understand disaster risk to
reduce the frequency and effects of disasters (Aitsi-
Selmi et al, 2015). Ultimately current risks are
reduced and, the development of new ones is
minimized (Mizutori, March 2020). Developing risk
communication improvement strategies can help
planners and managers design and implement
effective risk management programs (Fathollahzadeh
et al, 2021). Effective Risk Communication is critical
for health and other sectors, government authorities,
the media, and the public. A consistent collection of
reliable, strong data from past and present inform
projections to build good strategies and interventions
9
https://apps.who.int/iris/handle/10665/272964
for the future; the ultimate result is to reduce disaster
risks and improve the safety and functionality of
critical infrastructure (Mizutori and March, 2020).
Operative information and knowledge management
include risk assessment, surveillance, early warning,
information management, technical guidance, and
research.
Table 2: Four Priorities for action for NCD – Adapted from
(Bullock et al, 2013 & Hung et al, 2021) and our literature
review.
Priority 1. Understanding disaster risk:
Effective Risk Communication (health and other sectors,
government, media, and the public)
Operative information and knowledge management (risk
assessment, surveillance, early warning, information
management, technical guidance and research)
Patient engagement (identify priority conditions for
inclusion in emergency response, outline pre- emergency
profile of NCDs and assess readiness of health facilities).
Leveraging technologies: Encourage community-based
screening for NCDs w/ digital tools to scale level of care.
Priority 2. Strengthening disaster risk governance:
Policies, strategies and legislation that define structures,
roles and responsibilities of governments and other actors that
strengthen capacities (incl. care costs for NCDs)
Patient engagement with care providers and other
stakeholders in planning and crisis management.
Priority 3. Investing in disaster reduction for resilience:
Human resource plans (staffing, education training).
Financial resources to supports implementation of Health
EDRM activities, capacity development and contingency
funding for emergency response and recovery.
Include contribution from the whole care team,
(pharmacists, etc.) to provide focused interventions,
specialised counselling and care coordination
Health infrastructure and Logistics that includes supply
chain of essential NCD medicines.
Patient engagement and coordination for contingencies,
with individualized emergency plans (NCD patient profiles),
Leveraging technologies: “care anywhere” concepts
Priority 4. Enhancing disaster preparedness:
Strengthen the capacity of local health workforce and
inclusive community-centered planning and action –
Establish monitoring and evaluation to constantly assess
progress and provide feedback for managing risks and
capacities and fine-tuning of strategies.
Patient engagement in Post Emergency Debrief to
strengthen response to needs of NCD patients
Integrate NCD patients in initial rapid assessments and
organizing the service delivery that focus on their care.
As an example, community-based screening for
Protecting Non-communicable Diseases Patients during Pandemics: Fundamental Rules for Engagement and the Case of Lebanon
311

diabetes and hypertension that leverage digital tools
may advance the level of care and avail these services
at scale, for NCD patients screening (Saleh et al,
2018) even during disasters. Here we echo the
recommendations of Devi et al (2020) that patients
and care providers ought to collaboratively design
their care pathways with the inclusion of “care
anywhere” concepts leveraging advancements in
technology; among those, the support of home
monitoring, optimized accurate diagnosis,
personalized care plans, and facilitated timely
intervention through mobile devices and integration
of digital portals. The resilience of services away
from the traditional setting would bring continuity of
care in the face of emergent disruption.
Priority two calls for strengthening disaster risk
governance. It is critical to invite all stakeholders to
partner together, with the ultimate goal of using and
implementing all instruments to mitigate disaster risk
(UN Office for DRR, 2015). NCD stakeholders are
part of this planning and crisis management group.
Aside from risk reduction, the target of this group is
to improve economic, social, health, and
environmental durability. Agencies must implement
policies, strategies, and legislation that define the
structures, roles, and responsibilities of governments
and other actors including strategies for strengthening
Health EDRM capacities and related services.
Priority 3 calls on investing in disaster reduction
for resilience. I Integration of primary, secondary,
and tertiary healthcare systems into disaster risk
management becomes vital for NCD patients to shift
towards alternate, well-prepared and well-resourced
healthcare services since the essential healthcare
systems and their workers are more engaged in the
containment of disaster, as happened during the
COVID-19 pandemic. This includes Data collection
and assessment for NCD patient profiles, as well as
reviewing the national essential medicines list to
maintain fluidity in the drug supply chain (Slama S et
al, 2017).
Supporting primary healthcare professionals and
training them is important to achieve this shift.
Planning of human resources is necessary, which
includes staffing, education, and training across the
spectrum of capacities at all levels, and the
occupational health and safety of personnel. Some
recommend increasing the involvement from the
whole care team, including pharmacists that build on
the key roles they already play as primary healthcare
professionals in the community to provide focused
interventions, specialized counselling, and care
coordination, improving patient engagement to
achieve better outcomes (Pinto et al, 2020). Financial
resources to supports implementation of NCD
support activities, capacity development, and
contingency funding for emergency response and
recovery. Investments are also required for health
infrastructure and logistics that focus on safe,
sustainable, secure, and prepared health facilities,
critical infrastructure (e.g. water, power), and supply
systems to sustain the care ecosystem for NCD
patients, in continuity without compromise.
Considerations for NCD patient-centered care
include the best practices to ensure management
sustainability in the most collaborative and
productive ways between healthcare stakeholders and
patients.
Priority 4 emphasizes on improving preparedness
for effective response and on "Building Back Better"
in recovery, rehabilitation, and reconstruction. The
post- disaster phase evaluation of emergency response
to NCDs is critical to "Building Back Better".. This
evaluation will "build" the road to strengthening the
NCD surveillance system, implementing strategies to
prepare better in case of new emergencies, and
incorporating NCDs into government budgeting and
plans (WHO, 2018). To alleviate the disaster’s effects
on NCD patients, it is essential to strengthening the
Lebanese national good governance to include NCDs
in national disaster plans. A robust public health
surveillance system will spot indicators that identify
vulnerable groups (NCD patients in the case of the
COVID-19 pandemic, among others), for further
Emergency and Disaster Risk Management (EDRM),
planning (Law, 2019). Further, a focus on a systemic
approach to strengthening the capacity of the local
health workforce and inclusive community-centred
planning and action for the wellbeing of the
vulnerable NCD population in a pandemic situation.
3.3 NCD Patient Engagements in
Disaster Planning
A comprehensive response to NCD management in
emergencies that may place a large demand on
resources is not trivial. Often, NCD patients find
themselves at the lower priority as aspects of non-
communicable disease control become inadequate to
reduce the potential risk of morbidity and mortality.
Findings from our review have stressed the
engagement of NCD patients in the planning and
preparedness for disasters. We, therefore, stress the
importance for policymakers, communities, and
individuals to give adequate attention to disaster risk
HEALTHINF 2022 - 15th International Conference on Health Informatics
312

reduction (DDR), specifically to include the needs of
NCD patients. During a pandemic, it is critical to
focus the resources available on the containment of
the pandemic while also continuing to support the
NCD patient journey. The strengthening of health
infrastructure and logistics are important to build that
focus on safe, sustainable, secure, and prepared health
facilities, critical infrastructure (e.g. water, power),
and supply systems to support the complete Health
ecosystem. However, this must include, for
instance,reviewing the national essential medicines
list to maintain fluidity in the drug supply chain for
NCD patient journey support.
NCD patients and care providers are stakeholders
in the planning and management of the crisis. Patient
engagement in the coordination for contingencies,
with individualized emergency plans (NCD patient
profiles) ensures that adequate resources, essential
medicines, and technologies are available upon need.
NCD patients must participate in the elaboration of a
clear and coordinated action plan addressing the
challenges faced by NCD patients before, during, and
after disasters. This planning effort identifies priority
conditions for inclusion in emergency response that
outline the pre-emergency profile of NCDs and assess
the readiness of the concerned health facilities.
Further, the finding of this study reinforces a
recommendation that NCD patients engage in post-
emergency debrief activities on lessons learned to
strengthen the response to the needs of NCD patients
in the next emergency events with a continuous loop
of monitoring and evaluation.
3.4 Leveraging Technology Tools
The development of an action plan for NCD patients
must leverage solid tools for collecting reliable data,
such as electronic medical records (EMR / EHR),
strengthening national healthcare and policies, in
addition to the capacity of the medical body and
institutions. Technologies that provide for the concept
of “care anywhere” leveraging advancements in
telemedicine, for instance, become necessary tools in
the success of the NCD journey continuum. Namely,
the support of home monitoring, optimized accurate
diagnosis, personalized care plans, and facilitated
timely intervention through mobile devices and
integration of digital portals. Additionally,
community-based screening for diabetes and
hypertension that leverage digital tools may advance
the level of care and avail these services at scale, for
NCD patients ‘screening and early detection. This
further contributes to reducing the demand for acute
care. Additionally, empowering individuals through
educating them about different self-care interventions
can mitigate the effect of the disaster on their health.
They must strive to learn how to use mHealth
applications and web-based technologies. Wearable
devices and teleconsultation are ways to maintain a
connection with their healthcare providers.
Resilience in disaster management helps the country
to respond to and to recover from it in a better way.
Investing in technology is an opportunity that can
optimize the country's response to future disasters.
Lebanon must learn from this pandemic to better
prepare for any future disaster and to establish strong
policies for the final target citizens and community.
4 RECOMMENDATIONS
The Lebanese government and community partners
should pay immediate attention to develop an action
plan and strategies where vulnerable populations
notably NCD patients are included in the response
and mitigation efforts. Planners and practitioners
must therefore:
1) Establish an overall coordinated approach to
develop effective risk assessment and
communication plans that include both public
and private sectors (MoPH, primary healthcare
providers, community and media) with the
consult and the participation of key stakeholders
in the NCD patient journey.
2) Provide means to collect and diffuse operative
information that aid in risk assessment,
surveillance, early warning, information
management, technical guidance, and research.
Emphasize transforming knowledge to policy to
strengthen the structures and response
mechanism to serve specific needs of NCD
patients throughout their journey.
3) Define clear roles and responsibilities with a
rapid response plan that includes contingencies
to care for NCD patients – for instance, plans that
encourage community-based screening for
NCDs w/ digital tools to scale the level of care
and set up the provisions necessary for continuity
of care in the time of stress on the health
ecosystem.
4) Strengthen capacities, in addition to funds and
resources set aside for the care of NCDs in their
journey. Education and training would be
included in the plan to make sure that the
readiness for response and care of the NCDs.
5) Augment diagnostics centres capabilities to take
on the added burden during emergencies,
Protecting Non-communicable Diseases Patients during Pandemics: Fundamental Rules for Engagement and the Case of Lebanon
313
through scalable resource planning – with the
ability for the government to unlock assistance in
funding and resources.
6) Equip treatment facilities with telehealth and
other scalable technologies, potentially, standing
up mobile clinics to increase access to care.
7) Develop the ability to muster other supportive
functions and volunteers in the health ecosystem,
such pharmacists and informal carers, to alleviate
the burden on the primary care function.
8) Optimize the logistics supply chain. The plans
must account for logistical support to provide an
adequate flow of medicines and required
treatment for the continuity of care for NCD
patients. Human, financial, and supply chain
resources must be ready to scale to the required
capacity.
9) Finally, establish monitoring and evaluation
cycles that integrate NCD patients in rapid
assessments and organizing the service delivery
that focuses on their care.
We, therefore, call on the responsibility of the
disaster planners to include NCD patients in response
and recovery planning. They are informed and pivotal
stakeholders. Leverage technology such as portals,
integration tools, mobile and telehealth, supply chain,
and tracing technology to facilitate the identification,
planning, communication, and delivery of care - as
“care anywhere”.
5 CONCLUSION
The Lebanese health system is fragile and lacks a
sustainable preparedness to build a strong future
considering the vulnerable populations. As we aim
for Universal Health Coverage while protecting the
vulnerable, it is crucial to accompany them during
their disease journey, in periods of peace and
disasters. NCD patients have been the most hit by the
COVID-19 pandemic then later on with the severe
shortage of medicines resulting from the economic
situation. Structured guidelines and considerations
under the Sendai framework priorities will build a
strong ground for preventing disruptions of the
different stages of the NCD patient journey. The
success of this action plan is the contribution of all
involved stakeholders under the umbrella of good
governance and the integration of the NCD care in
emergency preparedness and responses.
Our work reviews the extant literature and draws
the connection between theory and practice. We
summarize what is in the literature and identify a
serious gap in scientific studies that would improve
the NCD journey. Potentially, further research could
explore the level of resources required in order to
support the underserved NCD patients in an effective
response, given certain contexts, during abnormal
situations, as pandemics, etc.
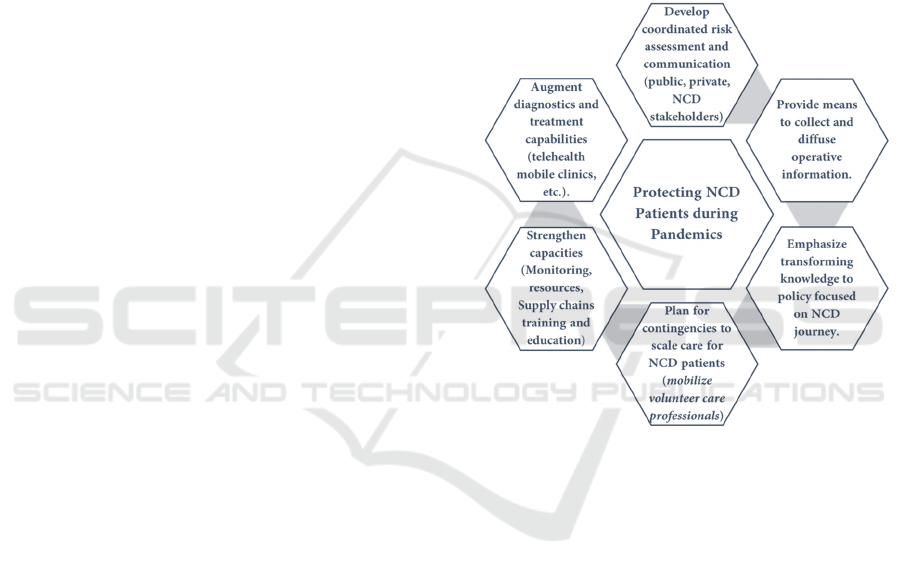
In conclusion, our contribution is timely and
primarily targeted towards the practices of health
disaster planning and response. Moreover, our paper
suggests the broad lines of such response strategy and
identifies key initiatives that must become priorities
in emergency response that includes provisions for
protecting NCD patients during pandemics (Fig.2).
Figure 2: Key priorities for protecting NCD patients during
a pandemic (by the authors).
REFERENCES
Aitsi-Selmi, A. et al. The Sendai Framework for Disaster
Risk Reduction: Renewing the Global Commitment to
People’s Resilience, Health, and Well-being. Int J
Disaster Risk Sci 6, 164–176. (2015).
Bardus M & al Assessing the Quality of Mobile Phone
Apps for Weight Management: User-Centered Study
With Employees From a Lebanese University; JMIR
Mhealth Uhealth; 7(1):e9836. doi: 10.2196/mhealth.
9836 (2019).
Bullock, J. A.et al. Mitigation, Prevention, and
Preparedness. Introduction to Homeland Security, 435–
494. (2013).
Chan E.Y.Y & al. What Happened to People with Non-
Communicable Diseases during COVID-19:
Implications of H-EDRM Policies; IJERPH; (2020).
Devi, R., Kanitkar, K., Narendhar, R. et al. A Narrative
Review of the Patient Journey through the Lens of Non-
HEALTHINF 2022 - 15th International Conference on Health Informatics
314

communicable Diseases in Low- and Middle-Income
Countries. Adv Ther 37, 4808–4830 (2020).
El Karak F. & al. The impact of disasters on cancer care in
Lebanon; Future Oncol. 17(6), 629–631; 10.2217/fon-
2020-0927 C 2021 Future Medicine Ltd; Published
Online:5 Jan (2021).
Fathollahzadeh, Abazar, et al. "Strategies of relief
organizations for improvement of disaster risk
communication process in Iran." (2021).
Fouad, F. M., Barkil-Oteo, A., & Diab, J. L. Mental Health
in Lebanon's Triple-Fold Crisis: The Case of Refugees
and Vulnerable Groups in Times of COVID-19.
Frontiers in Public Health, 8, 1049. (2021a).
Fouad, F. M., McCall, S. J., Ayoub, H., Abu-Raddad, L. J.,
& Mumtaz, G. R. Vulnerability of Syrian refugees in
Lebanon to COVID-19: quantitative insights. Conflict
and Health, 15(1), 1-6. (2021).
Gnanapragasam, S., Aitsi-Selmi, A., Rashbrook, E., &
Murray, V. Addressing non-communicable diseases in
disaster risk reduction–an issue of equity. Journal of
epidemiology and global health, 6(2), 119-121. (2016).
Hamadeh, R. S., Kdouh, O. A., Hammoud, R., Leresche, E.,
& Leaning, J. Can Primary Healthcare be Protected as
a Public Good in Lebanon Today? (2020).
Hamadeh, R.S. et al. Working short and working long: can
primary healthcare be protected as a public good in
Lebanon today? Confl Health 15, 23 (March 2021).
Helou et al. The Effect of the COVID-19 Pandemic on
Physicians’ Use and Perception of Telehealth: The Case
of Lebanon; IJERPH 2020, 17, 4866; (2020).
Hung, K. K., Mashino, S., Chan, E. Y., MacDermot, M. K.,
Balsari, S., Ciottone, G. R., ... & Graham, C. A. Health
Workforce Development in Health Emergency and
Disaster Risk Management: The Need for Evidence-
Based Recommendations. IJERPH, 18(7), 3382 (2021).
Karak, F. E., Rawadi, E., Sawan, J., & Haddad, F. G.
(2021). The impact of disasters on cancer care in
Lebanon. Future Oncol. 17(6), 629–631; 10.2217/fon-
2020-0927 C 2021 Future Medicine Ltd (2021).
Khoury P, Azar E, Hitti E. COVID-19 Response in
Lebanon: Current Experience and Challenges in a Low-
Resource Setting. JAMA.; 324(6):548–549 (2020).
Law, R. Guidance on Research Methods for Health
Emergency and Disaster Risk Management. WHO.
(2019).
Manca D. P. Do electronic medical records improve quality
of care? Yes. Canadian family physician Medecin de
famille canadien, 61(10), 846–851. (2015)
Medecins sans frontiers. Overlapping crises in Lebanon
increase needs and worsen access to care. (8 January
2021).
Mizutori, M. Reflections on the Sendai Framework for
Disaster Risk Reduction: Five Years Since Its
Adoption. Int J Disaster Risk Sci 11, 147–151 April
2020.
Nassereddine, G., Habli, S., Slama, S., Sen, K., Rizk, A., &
Sibai, A. M. COVID-19 and non-communicable
diseases in the Eastern Mediterranean Region: the need
for a syndemics approach to data reporting and
healthcare delivery. BMJ Global Health, 6(6), e006189.
(2021). Online September 13, 2016 (January 2017);
Pinto, G. S., Bader, L., Billberg, K., Criddle, D., Duggan,
C., El Bizri, L., ... & Laven, A. Beating non-
communicable diseases in primary health care: the
contribution of pharmacists and guidance from FIP to
support WHO goals. Research in Social and
Administrative Pharmacy, 16(7), 974-977 (2020).
Rentschler, J., Klaiber, C., Tariverdi, M., Desjonqueres, C.,
& Mercadante, J. Frontline: Preparing Healthcare
Systems for Shocks from Disasters to Pandemics.
World Bank. (2021).
Rosita di Peri.; A Sectarianised Pandemic: COVID-19 in
Lebanon; IAI commentaries 20; Published on IAI
Istituto Affari Internazionali (2020, October).
Sacca L.& al Using Intervention Mapping to Develop
Health Education and Health Policy Components to
Increase Breast Cancer Screening and Chemotherapy
Adherence Among Syrian and Iraqi Refugee Women in
Beirut, Lebanon; Front. Public Health, (15 April 2020).
Saleh S. & al Sijilli: A Scalable Model of Cloud-Based
Electronic Health Records for Migrating Populations in
Low-Resource Settings; J Med Internet Res;22(8):
e18183) (2020).
Saleh, S. et al. mHealth use for non-communicable diseases
care in primary health: patients' perspective from rural
settings and refugee camps. Journal of public health
(Oxford, England), 40(suppl_2), ii52–ii63. (2018).
Sethi et al. Community-Based Noncommunicable Disease
Care for Syrian Refugees in Lebanon; Global Health:
Science and Practice | Volume 5 | Number 3; (2017).
Slama S. et. al. Care of non-communicable diseases in
emergencies; Lancet 2017; 389: 326–30 Published.
United Nations Office for Disaster Risk Reduction.. 54.
United Nations Office for Disaster Risk Reduction:
What is the Sendai Framework for Disaster Risk
Reduction? (2015, March 18).
Zablith, N., Diaconu, K., Naja, F., El Koussa, M., Loffreda,
G., Bou-Orm, I., & Saleh, S. Dynamics of non-
communicable disease prevention, diagnosis and
control in Lebanon, a fragile setting. Conflict and
health, 15(1), 1-13. (2021).
Zaki, N., Alashwal, H., & Ibrahim, S. Association of
hypertension, diabetes, stroke, cancer, kidney disease,
and high-cholesterol with COVID-19 disease severity
and fatality: A systematic review. Diabetes &
metabolic syndrome, 14(5), 1133–1142. (2020).
Protecting Non-communicable Diseases Patients during Pandemics: Fundamental Rules for Engagement and the Case of Lebanon
315
