
Factors Influencing Tele-dermatology Adoption among the Lebanese
Youth: A Pilot Study at Saint Joseph University
Nanor Aroutine
a
, Nabil Georges Badr
b
and Joumana Yeretzian
c
Higher Institute of Public Health, Saint Joseph University, Beirut, Lebanon
Keywords: Tele-dermatology, Technology Acceptance Model (TAM), Mobile Medical Application, Skin Cancer,
Consumer Acceptance.
Abstract: The demand and use for Tele-dermatology (TDM) to diagnose skin lesions is rising worldwide. Using the
technology acceptance model, we evaluate the factors influencing the acceptance of Tele-Dermatology to
diagnose skin lesions among the Lebanese students. We complete a pilot study with Lebanese students from
Saint Joseph University of Beirut (USJ). After examining the responses in a descriptive analysis, we develop
some initial hypotheses and proceed to build the statistical model to test them using Smart PLS3. Our findings
show that 64% of the students are ready to use Tele-Dermatology in their everyday life. Most of those students
are females between 18 and 24 years old. Wrapping up our results, information from this study indicates that
marital status is most likely a determinant of intention to use TDM among students – whereby, most single
students are ready now (65%) while most married students are inclined to use it in the future (67%). The study
also suggests that the Lebanese youth prioritize result demonstrability as a factor in their intention to use
TDM. Further, mobile TDM must save them time must be easy to use to be perceived useful.
1 INTRODUCTION
“The two areas that are changing... information
technology and medical technology. Those are the
things that the world will be different from in 20 years
from now than it is today”- Bill Gates
1
.
Decentralized, mobile and personalized care has
improved population access to care. Medical mobile
applications are redefining the future of medical
consultation; a trend that started at the turn of the
century caused the line between physical and virtual
care to blur. Before the 2019 COVID-19 pandemic,
physicians and patients started using telehealth to care
for different conditions including cancer, behavioural
health, surgical recovery, substance abuse, home
dialysis and more. These telehealth use cases cover
the full spectrum of care from acute to post-acute and
urgent to managing healthy lifestyles. The demand for
a
https://orcid.org/0000-0001-6509-1378
b
https://orcid.org/0000-0001-7110-3718
c
https://orcid.org/ 0000-0001-5805-4915
1
https://www.quotemaster.org/author/Bill+Gates
2
https://gco.iarc.fr/
telehealth, especially for diseases in which the
incidence rate is increasing yearly, such as in the case
with cancer, is on a rise
2
.
1.1 Mobile Tele-dermatology
Worldwide, 2020 has seen an estimated 19.3 million
new cancer cases of which more than 8% were skin
related, with loss of life in about 1 in 12 skin cancer
patients (Sung et al, 2021), and an increase of 15% in
skin cancer cases since 2018 (Ferlay, et al. 2018).
Advancements in technology sought to improve
early detection and reduce the mortality rate of the
disease through skin cancer screening for early
detection of suspicious skin lesions which can
potentially lead to skin cancer (Jolliffe et al., 2001).
Mobile Tele-dermatology (TDM) is a mobile medical
application by which patients can get a diagnosis for
their skin lesions, anywhere and anytime (Desai et al.,
2010; Massone et al., 2014). The technology is about
Aroutine, N., Badr, N. and Yeretzian, J.
Factors Influencing Tele-dermatology Adoption among the Lebanese Youth: A Pilot Study at Saint Joseph University.
DOI: 10.5220/0010746400003123
In Proceedings of the 15th International Joint Conference on Biomedical Engineering Systems and Technologies (BIOSTEC 2022) - Volume 5: HEALTHINF, pages 15-25
ISBN: 978-989-758-552-4; ISSN: 2184-4305
Copyright
c
2022 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
15
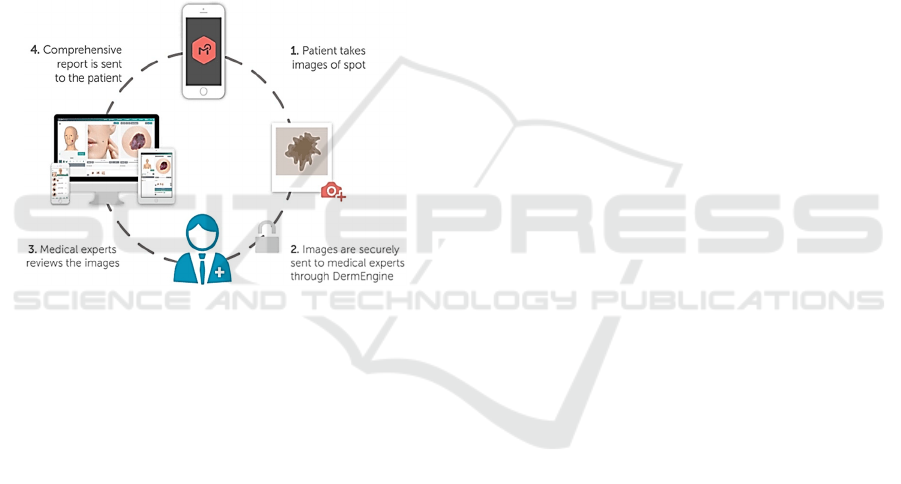
acquiring images of a suspect skin area and presenting
them to a remote attending practitioner for evaluation
(Fig 1.). The technology was initially evaluated in
treating incidences in rural areas (Sáenz et al, 2018),
where dermatology services are commonly managed
by healthcare personnel with minimal specialty
training.
There are two models for processing these images.
One model uses on store and forward mechanisms,
which are less expensive, but require more wait time
for diagnosis and treatment. The alternative uses a
video conference or “synchronous session”, between
the patient and the specialist. The patient gets an
instant treatment plan. The difference lies in the cost
of the two methods, and the diagnosis referral time
(Livingstone & Solomon, 2015; Vidal-Alaball et al.,
2018; Wang et al., 2020a).
Figure 1: Tele-Dermatology (Source: DermEngine).
At the turn of the 21
st
century, even prior to the
recent COVID-19 pandemic, tele-dermatology
(TDM) had received acceptance among patients,
because of the instantaneous nature of the diagnosis
and management regimen for the condition, and
because it had educational value to the primary care
physician (Eedy and Wootton, 2001). Initially,
diagnostic reliability, image quality and storage
requirements were central notions to the adoption
conversation (Whited, 2006). Web consultations in
dermatology became possible shortly after (Massone
et al, 2008). The continued evolution in technology
improved TDM accuracy and its cost effectiveness
brought the product to the mainstream of practice
(Lee and English, 2018). The main advantages were
prioritization in cancer screening and rapid screening
for trivial conditions (Romero et al, 2018), as
administrative, regulatory, privacy, and
reimbursement policies surrounding this dynamic
field continued to evolve (Lee and English, 2018).
During the Covid-19 pandemic, TDM was seen as
an alternative to in-person visits, as the number of
people using medical applications increased by 50%
compared to 2019 (Koonin, 2020). Many specialists
encouraged patients to perform Telehealth from the
comfort of their homes (McGee et al., 2020), to
minimize unnecessary clinical visits and avoid
endangering their lives through transmission with the
virus (Mostafa & Hegazy, 2020). Therefore, TDM
was considered effective in decreasing the risk of
Covid-19 transmission by minimizing clinical visits
and avoiding overcrowdings of the hospitals both in
private and public facilities (Cartron et al, 2020).
1.2 Motivation
The global TDM market accounted for US$ 4.5
billion in 2019 and is estimated to be US$ 44.8 billion
by 2029 and an anticipated CAGR of 26.0%.
Studies conducted in several countries, such as the
United States (Cartron et al, 2020), United Kingdom
(Nicholson et al, 2020) and Australia (Abbott et al,
2020) have shown how people embraced TDM as a
mobile application to diagnose their skin lesions.
Patients with better health status, those of younger
age and those with less frequent visits to a
dermatologist were more accepting of Tele-
Dermatology (Nicholson et al, 2020); noting that
issues of image quality, privacy concerns, image
storage and retention are indicated as impediments to
wider use (Abbott et al, 2020). In countries where
they have adopted Mobile TDM for skin diagnosis,
users have reported the technology to be a cost-
effective application, which they would prefer using
rather than face-to face clinical visits to reduce cost
and waiting time (Wang et al., 2020b).
In the country of Lebanon, a developing country
where cases of skin cancer have been doubling over
10 years (2006-2016) (Moph, n.d.) there has been
little insight on the adoption of TDM. Telehealth
adoption in Lebanon has been informal and TDM has
not reached mainstream use by practitioners (Shaarani
et al, 2021). We therefore, find it interesting to
investigate this phenomenon and evaluate the factors
that could influence the adoption of mobile medical
application.
In our study, we intend to answer the question:
What are the factors that can influence the intention
to use of TDM in Lebanon?
2 BACKGROUND
Technology acceptance models (TAM) is a
theoretical framework to assess people’s perception
regarding the adoption of new technologies. It is a
HEALTHINF 2022 - 15th International Conference on Health Informatics
16
tailored representation of factors influencing one’s
intention to use a certain technology, in our case, this
technology is TDM.
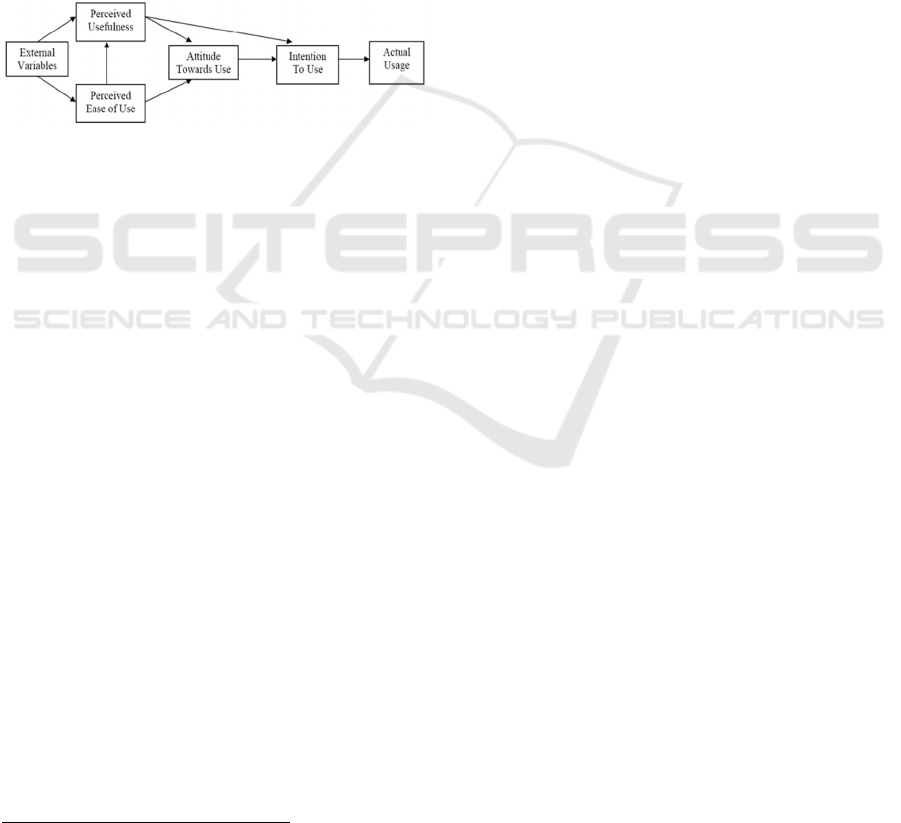
Technology Acceptance Model (TAM) has been
used to investigate how perceived usefulness of a
technology and its perceived ease of use, can
influence the users’ intention to use that technology
(Fig. 1) (Davis, 1989; Szajna, 1996; Venkatesh and
Davis, 2000). TAM suggests that an individual’s
technology usage behaviour is determined by the
attitude toward technology usage, predicted by the
extent to which an individual believes that using a
technology will enhance his or her task performance
(perceived usefulness) and the extent to which an
individual believes that using a technology will be
free of significant effort (perceived ease of use).
Figure 2: Simplified Technology Acceptance Model.
Studies using TAM have extended the model to
cover multiple contexts (TAM2, etc.), indicating the
usage and acceptance behaviour towards technology
(Venkatesh et al, 2003). Certain TAM relationships
were found to be significant, whereas others were
inconsistent (Holden & Karsh, 2010). Others have
connected ease of use and usefulness to social impact,
facilitating conditions, attitudes and behaviour of
users in measuring intention to adopt of health
information technologies (Garavand et al, 2016). In
telemedicine, we can find long-standing evidence of
TAM use, for physician acceptance of telemedicine
and the related technologies (Hu, et al, 1999; Chau
and Hu, 2002; Kamal et al, 2020), implying that
acceptance of this technology was a major challenge
in the context of adoption. While the model has been
widely tested, validated and extended in health
informatics applications used by medical
professionals (Ketikidis et al, 2012; Rahimi et al,
2018) they have seldom been applied to the modelling
of consumer (patient) acceptance of health
informatics applications (Rahimi et al, 2018).
3
https://www.who.int/health-topics/social-determinants-
ofhealth#tab=tab_1
3 RESEARCH MODEL
3.1 Antecedents and Hypotheses
Based on previous evidence with TAM and the
extended model of Venkatesh and Davis (2000), we
developed our model to test the stated hypotheses and
learn about TDM usage and factors of acceptance.
Factors influencing the intention to use are therefore:
Social determinants, medical factors, result
demonstrability, perceived risk, subjective norms,
perceived usefulness and perceived ease of use.
We consider the following variables as latent
variables (Section 4):
SI: Subjective norms (Q: 29 and 30);
SDH: Social determinants (Q: 3 thru 5);
MED: Medical factors (Q: 1, 2, 6 thru 10);
RD: Result demonstrability (Q: 15, 17, 31, 32);
PR: Perceived risk (Q: 18, 20 thru 22, 25, 26, 33 thru
35);
PU: Perceived usefulness (Q: 11 thru 14, 19, 27 and
28);
PEOU: Perceived ease of use (Q: 16); UI: Intention
to Use (Q: 23 and 24).
3.1.1 Social Determinants
We identified social determinants as indicators of
educational level, work and marital status
3
. The
descriptive analysis found some relevance of
education specialty, and marital status, etc. (Table 2).
The technology acceptance model developed by
Davis et al. (1989) supports education specialty that
may indicate a varied experience with technology.
Consequently, we state our first hypothesis as
H1: Social Determinants such as marital status
and education specialty affect perceived usefulness of
mobile TDM by students
3.1.2 Medical Factors
Medical factors are included to examine the potential
significance of the existence of family cancer history
in the adoption context. Family history of skin cancer,
previous skin cancer removed and presence of moles
larger than 2 mm were considered significant in an
earlier study (Horsham et al., 2016). Therefore, we
included them in the initial model, as they are
contextual to the setting of TDM. We also included
age and gender, as potential indicators of the adoption
dynamics - as it was observed in the descriptive
Factors Influencing Tele-dermatology Adoption among the Lebanese Youth: A Pilot Study at Saint Joseph University
17

analysis (Table2) and is also supported by Venkatesh
& Morris (2000). Therefore, we formulate our second
hypothesis as:
H2: Medical factors such as family cancer history,
age and gender affect perceived usefulness of mobile
TDM by students
3.1.3 Result Demonstrability
Supported by Modified TAM (TAM2) model
(Venkatesh and Davis, 2000), the factor of result
demonstrability indicates the effectiveness of the
TDM in the early detection of the onset of the disease,
the user’s trust in technology. In the literature, some
studies reported that users expressed their concern
regarding their privacy if the application were to be
hacked, they also shared their anxiety of waiting for
the final diagnosis, and their doubt about the accuracy
of the image (Abbott et al, 2020). On the other hand,
medical practitioners expressed their concern towards
overloading their system with images, yet 55% of
informants in our study found TDM beneficial for
monitoring and self-examining skin lesions to detect
any suspicious lesions. About 40% of the students in
our study have expressed confidence in the accuracy
of the mobile application compared to face-to-face
diagnosis; and only 34% believed that a suspicious
mole or lesion diagnosis would be understandable
(thus able to provide the value expected). Therefore,
for our model, result demonstrability also relates to
the confidence of the user to receive comprehensible
prognosis – i.e. “the technology has to work, so that it
can be useful” –Survey Question (15, 17, 31 and 32).
Therefore, we formulate our third hypothesis as:
H3: Results Demonstrability (or effectiveness)
indicated by the user’s trust in technology
performance and the perceived ability of mobile TDM
to offer early detection, with accurate information and
an understandable outcome affects perceived
usefulness of mobile TDM by students
3.1.4 Perceived Risk
Perceived risk is an antecedent and a moderator of
user acceptance (Im et al, 2008; Kamal et al, 2020) –
as a moderator, it can either increase the strength of
the correlation or decrease it. In our model, we depict
three indicators for perceived risk:
a) The resistance to use (Im et al, 2008) (Q. 21); and
b) The efficiency of use in the context of selfservice
technology – i.e. saving time (Yang et al., 2019)
and money (Q. 25); and
c) Technology anxiety, learnability and reliability
(Mostafa & Hegazy, 2020) which characterizes
the user’s reluctance to use driven by lack of
familiarity with the technology (Q.33).
Therefore, for our model, we can define perceived
risk as factors of efficiency (saving time and money),
technology anxiety (training, technical assistance and
skill acquisition), presence or absence of facilitating
conditions (here shown as professional assistance
with the required dermatologists support to realize the
benefits from their mobile TDM APP (Gorrepati and
Smith, 2020; Giavina Bianchi et al, 2019). Hence, we
conclude that perceived risk can be conceived as an
antecedent for intention to use, and would have the
potential to moderate the association between
perceived ease of use and intention to use, similarly
between perceived usefulness and intention to use of
mobile TDM by students. We then state our next three
hypotheses as follows:
H4: Perceived risk, indicated by the resistance to
change, efficiency and technology anxiety affects
intention to use of mobile TDM by students
H5: Perceived risk, indicated by resistance to
change, efficiency and technology anxiety moderates
the relationship between perceived ease of use and
intention to use of mobile TDM by students
H6: Perceived risk, indicated by resistance to
change, efficiency and technology anxiety moderates
the relationship between perceived usefulness and
intention to use of mobile TDM by students
3.1.5 Subjective Norms
The descriptive analysis of the survey data indicated
that almost half (47%) of the sampled population
would be influenced by their family and friends to use
TDM. This phenomenon invokes the theory of
planned behaviour (Ajzen, 2011), where subjective
norms (indicated here by social influence) are
believed to shape an individual's behavioural
intentions, here the intention to use TDM. Our
seventh hypothesis therefore posits that:
H7: Subjective norms, indicated by social
influence, affects the intention to use of mobile TDM
by students.
3.1.6 Perceived Ease of Use and Perceived
Usefulness
Lastly, adapted from Venkatesh and Davis (2000) and
based on our background in Section 1, we defined
perceived ease of use as an indicator of user
perception of mobile TDM and perceived usefulness
as the perception of how useful the functionality of
TDM would be for the user. As a result, these two
latent variables directly affect a person’s intention to
HEALTHINF 2022 - 15th International Conference on Health Informatics
18
use TDM to diagnose skin lesions. In addition,
perceived ease of use directly affects the usefulness of
the application, in other words, if a consumer finds the
application easy to use, then it would be considered
useful. Consequently, the following final three
hypotheses are:
H8: Perceived usefulness, indicated by the
perception that the technology will serve the best
interest of the user, in a rapid, self-examination,
affects intention to use of mobile TDM by students.
H9: Perceived ease of use affects intention to use
of mobile TDM by students
H10: Perceived ease of use affects perceived
usefulness of Mobile TDM by students
We differentiated between two outcomes: (1) “I
will use Mobile TDM when it’s offered to me,” –
which implies readiness now (Q. 23); and (2) “I will
use Mobile TDM in my routine self-skin examination
in the future” – which implies readiness in the future
(Q. 24). The loading of UI1 and UI2 respectively then
assesses these outcomes, to their strengths and
relevance in indicating the “intention to use”.
4 MATERIALS AND METHODS
4.1 Approach and Study Design
We started our study on USJ students, after getting the
approval of the USJ ethics committee in February
2021. This pilot study, completed on May 2021, aims
to inform about assumptions and conditions for a
larger project scope (Hazzi and Maldaon, 2015). The
survey of TDM consumer acceptance was inspired
from an Australian study from Horsham et al. We
reformulated the questionnaire on Google docs. USJ
administration has approached students virtually. All
USJ students from different faculties, received emails
of the self-administered survey, only 89 participated.
After finishing data collection, we extracted the
answers on excel. Demographics were analysed by
descriptive statistics. Since the participant number
was not significantly high, we used SMART PLS 3 to
construct reliability and validity, path coefficient and
then we initiated the structural model to be able to test
for factors that influence the intention to use of the
participants.
4.2 Sample and Participants
We set out to investigate the use of TDM, a form of
telemedicine among the youth in Lebanese
Universities. We conduct this pilot at the University
of Saint Joseph in Beirut Lebanon. Eighty-nine (89)
students took part in this survey. Their demographics
are presented in Table 1.
Table 1: Sample description.
N=89
Gender Male 17%
Female 83%
Age < 20 years 25%
21 - 25 48%
26 - 30 13%
31 - 35 6%
36 - 40 2%
41 - 45 2%
Over 46 3%
Education Business Management 6%
Engineering & Sciences 16%
Humanities 20%
Medical & Health 47%
Political Science & Law 4%
Other 7%
Status Single 90%
Married 10%
The participants (N=89) with an average age of
25, were essentially females (n=74, 82%). Almost
half of the participants were from the Faculty of
Medicine (n=42, 47%). Slightly more than half the
participants work, either full time or part time, (n=52,
58%), while the majority of the participants were
single (n=80, 90%). Only 4 participants had skin
cancer history and only 3 had skin cancer previously
excised.
4.3 Survey Design
We developed a survey questionnaire of 27 questions
with two parts (Appendix) The first part, captured the
demographic and personal information of the
participants and the second explored the TDM context
using a 5-point Likert scale. We collected
demographics information about gender, age, field of
education, marital status as the literature indicated a
possible relation with intention to use (Section 4). We
also captured the prevalence of medical history of
cancer (Section 4.1.2), subjective norms (Section
4.1.5), and factors of risk (Section 4.1.4). We
exported the survey results to excel and normalized
the data in preparation for the descriptive and
statistical stages of the analysis.
Factors Influencing Tele-dermatology Adoption among the Lebanese Youth: A Pilot Study at Saint Joseph University
19
4.4 Descriptive Analysis
Indications from the descriptive analysis (Table 2)
show that, both genders are more or less equally ready
to embrace TDM now, but females are more prone to
use it in the future (12% more than males).
Table 2: Descriptive Analysis.
Readiness to Use (N=89) Now Future Intention
Among all participants 64% 57%
Gender
Male 60% 47%
Female 65% 59%
Age
< 20 years 77% 64%
21 - 25 60% 56%
26 - 30 67% 58%
31 - 35 60% 60%
36 - 40 0% 0%
41 - 45 50% 50%
46 - 50 67% 67%
Education
Business Management 60% 60%
Engineering & Sciences 71% 50%
Humanities 67% 67%
Medical & Health 64% 62%
Political Science & Law 50% 25%
Marital Status
Single 65% 56%
Married 56% 67%
Students aged less than 20 years old have reported
the highest intention to use. Engineering & Sciences
students are mostly ready to use TDM now (71%)
while political science students demonstrated the
lowest appetite (25%) Most single students are ready
now (65%), while the majority of married informants
were inclined towards future adoption (67%).
4.5 Statistical Data Analysis
We developed our model (Section 4) using SEM-PLS
via SmartPLS3.0, following the example of Aggelidis
& Chatzoglou (2009), Cepeda-Carrion et al. (2019)
and Kamal et al. (2020). Our sample (n=89) meets the
minimum sample size of 59, using the inverse square
root method (Kock and Hadaya, 2018). For reporting
purposes, we transformed the data captured on a
Likert scale to binary variables, where neutral
answers signified disagreement. That is, we
regrouped the results as either Agree (4-Agree, 5-
Strongly Agree), or Disagree (1-Strongly disagree, 2-
Disagree, 3-Unsure).
5 EVALUATION OF THE MODEL
AND RESULTS
5.1 Technology Acceptance Model
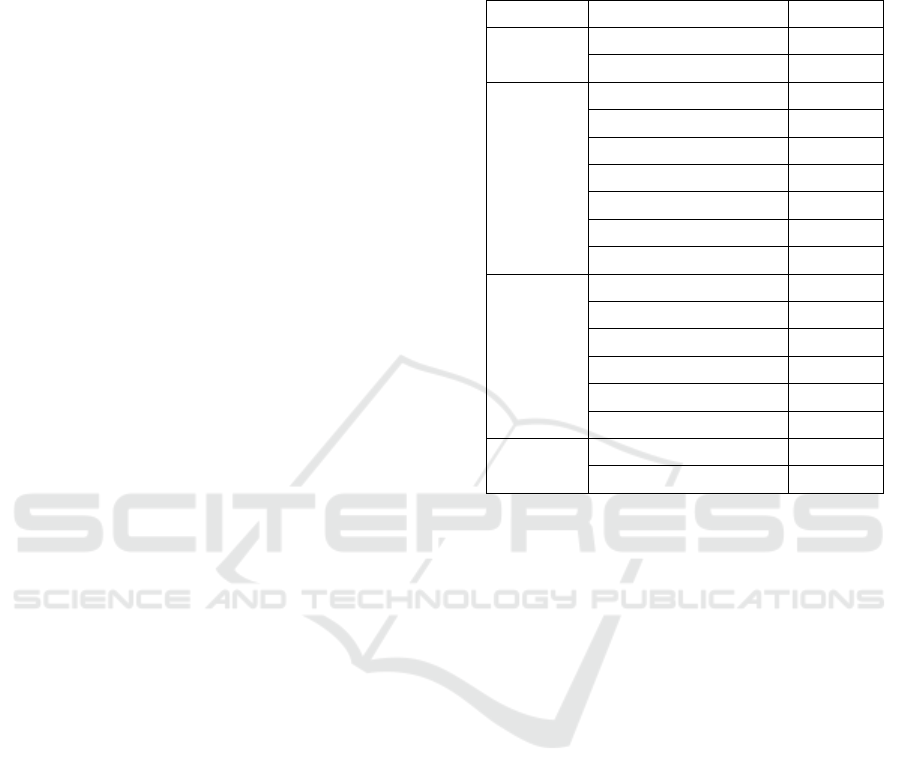
We loaded our model in SmartPLS3.0 and ran the
PLS algorithm. We then reduced the indicator
variables in order to reach convergent validity and
reliability. We accepted only the indicators with
loadings ≥ 0.708 as significant (Hair et al, 2019).
Figure 3 shows our valid model - with outer loading
factors.
Figure 3: Valid Model - with outer loading factors.
The model is of a reflective construct, therefore,
construct validation can be obtained through
Confirmatory Factor Analysis (CFA) (i.e. convergent
and discriminant validity) and reliability testing (i.e.
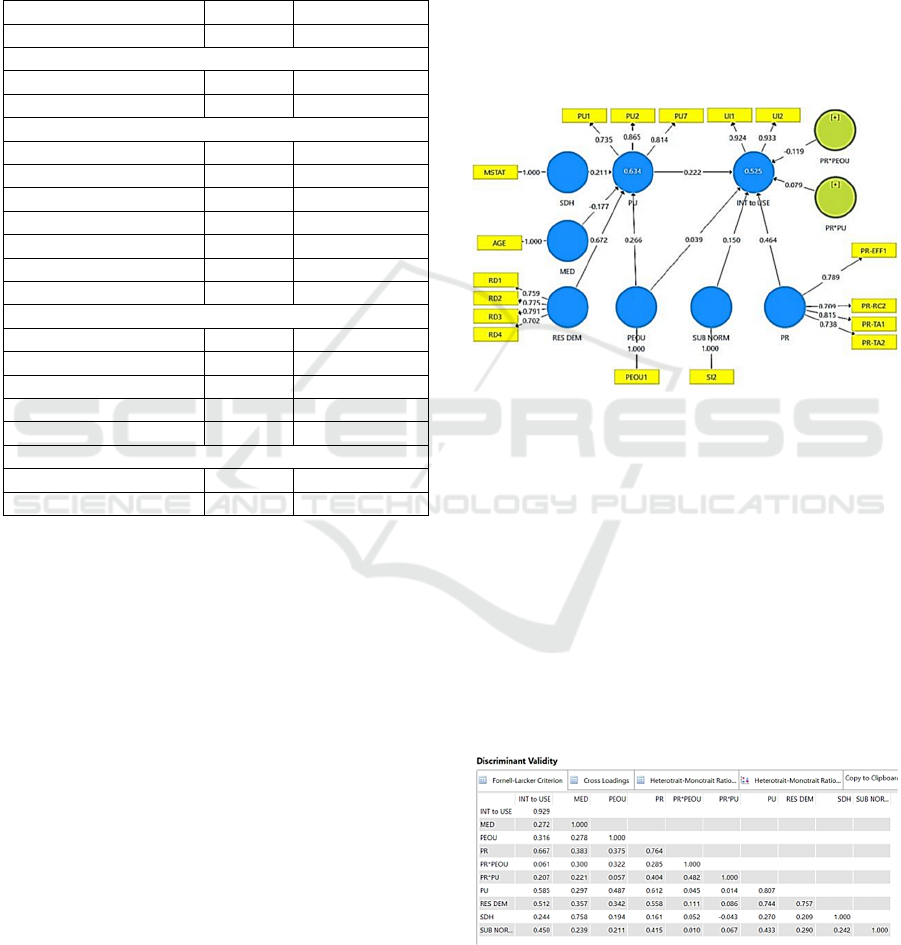
Cronbach's Alpha) (Hair et al, 2019). We find that the
model has good discriminant validity since the AVE
squared value of each exogenous construct (the value
on the diagonal) exceeds the correlation between this
construct and other constructs - see Fornell-Larcker
Criterion Values in Table 3 (values below the
diagonal).
Table 3: Discriminant Validity.
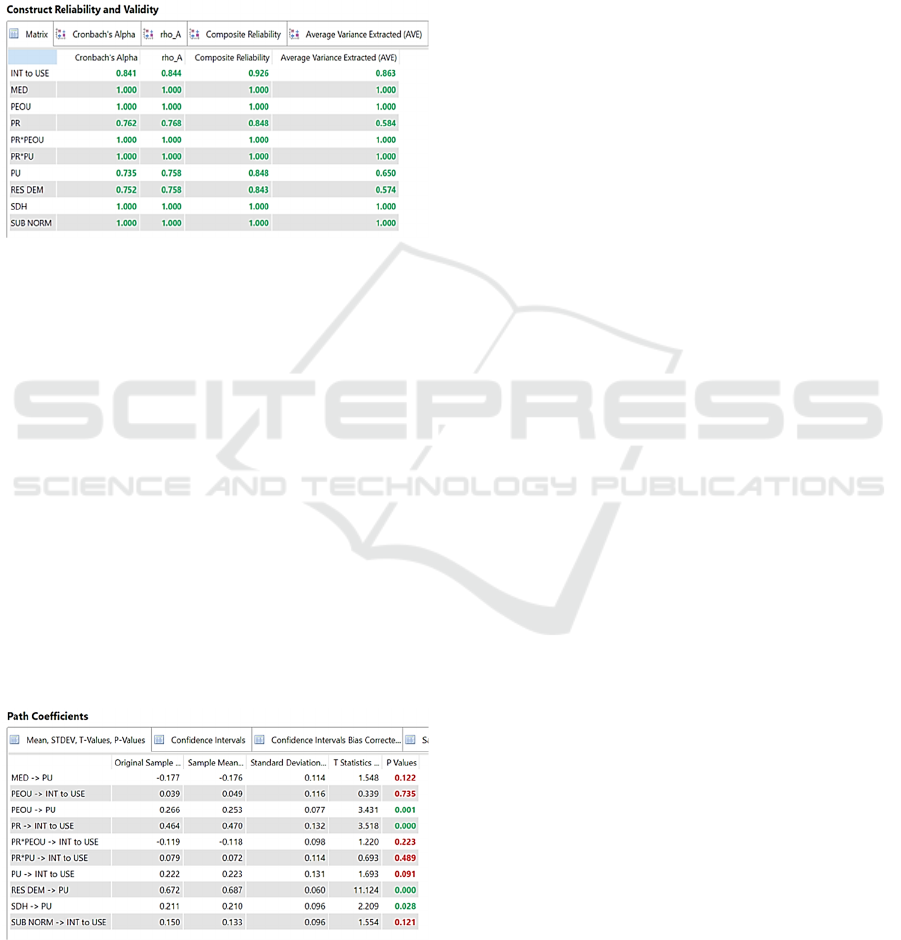
Subsequently, following Hair et al (2019), we
perform a convergent validity test by looking at the
loading factor value of each indicator against the
construct. We accept the indicators with loadings of
HEALTHINF 2022 - 15th International Conference on Health Informatics
20
≥ 0.708 as significant (Figure 2) with an AVE value
for each construct > 0.5. Subsequently, we assess the
construct reliability. The reliability test results in
table 4 show that all constructs have composite
reliability and Cronbach's alpha values greater than
0.7 (Hair et al, 2019). In conclusion, all constructs
have met the required validity and reliability.
Table 4: Construct Reliability and Validity.
5.2 Hypothesis Testing
We carried out the effect test using the p value tests
and t-statistics in the partial least squared (PLS)
analysis model of the SmartPLS 3.0 software (Table
5). A pvalue less than 0.05 (typically ≤ 0.05) is
considered statistically significant (Hair et al, 2019).
T-statistics show how many standard errors the
coefficient is away from zero. In our model, the t-
statistics are within the acceptable range. For the
hypotheses where p-values are ≤ 0.05, any t-value
greater than +2 or less than – 2 is acceptable (Hair et
al, 2019). The higher the T-value, the greater the
confidence we have in the coefficient as a predictor,
especially pointing to a significantly high confidence
(t=11.124) in the hypotheses of results
demonstrability – perceived usefulness (H3).
Table 5: Path Coefficient.
6 FINDINGS
6.1 Supported Hypotheses
Four Hypotheses are supported (H1, H3, H4 and
H10):
H1: Social determinants such as marital status
were found as antecedent to perceived usefulness
(p=0.028; t=2.209) with a predictability of 21.1 %
(path coefficient = 0.211). This makes sense as in the
descriptive analysis, we had observed that most single
students are ready now (65%) while most married
students will tend to use it in the future (67%). The
education indicator was is excluded from this finding
since it had to be removed to reach construct validity.
H3: The study results suggested that respondents
linked “results demonstrability” with “perceived
usefulness” of mobile TDM by students (p=0.000)
with a very high level of confidence (t= 11.124) and
with a very strong predictor of 67.2% (path
coefficient = 0.672).
Result demonstrability is indicated by the
effectiveness of mobile TDM to help detect skin
cancer in early stages, where the tool provides a
quality image, for an accurate assessment and
diagnostic by the practitioner reviewing the images.
This finding is aligned with the literature, where
patients have shown their willingness to use a medical
application if it’s beneficial for them. Moreover,
experts believe that comprehensibility and
functionality of the application play an important role
in encouraging people to adopt a certain technology
in their everyday life (Deng et al, 2018).
H4: Perceived risk is a strong antecedent to
intention to use of mobile TDM by students (p=
0.000; t= 3.518) with a predictability of 46.4% (path
coefficient = 0.464).
Hypothesis H4 is therefore supported. Perceived
risk (resistance to use, efficiency and technology
anxiety) predict the outcome by 46.4%. The
informants would use TDM if it is convenient
(loading factor = 0.773), and if it saves time (0.834)
as long as they receive the adequate training (0.776).
In this study, the indicator which weighed the most as
indicator of the risk variable was the technology
anxiety, which means professional assistance could
reduce the anxiety and may influence the behaviour
of the consumer in using TDM.
H10: Perceived ease of use is an antecedent to
perceived usefulness of mobile TDM by students
(p=0.002; t= 3.192) with a predictability of 26.6%
(path coefficient = 0.266). This finding agrees with
the theory of technology acceptance (Venkatesh and
Davis, 2000).
Factors Influencing Tele-dermatology Adoption among the Lebanese Youth: A Pilot Study at Saint Joseph University
21

6.2 Other Findings
We can also observe three findings that surprised us:
Medical factors do not appear to relate to the
perceived usefulness of mobile TDM by students
(H2). What is surprising here is that existing
conditions of cancer risk have not persuaded the use
of mobile TDM as a screening tool for early skin
cancer detection. Whilst dermatologists found TDM
useful for triage and diagnosis of most types of skin
conditions followed at primary care (Giavina et al,
2021), the patients use of the technology do not seem
influenced by their condition, in our study.
Perceived usefulness was not found to affect
intention to use (H8) – This is at odds with the
essential TAM theory. In our setting, even if the
application is thought of to be useful, the findings
inform that the Lebanese youth would not develop an
intention to use mobile TDM to diagnose skin lesions.
Similarly, as shown by hypothesis H9, perceived ease
of use was not a factor of intention to use in our
context.
6.3 Relevance of the Model
Our model produced R2 values of .634 and .525 for
perceived usefulness and intention to use
respectively. These moderate to substantial values
reinforce the value of our study and the findings (Hair
et al, 2019). They indicate that 63.4% of the
variability in the outcome in perceived usefulness and
52.5 % of the variability in the outcome in intention
to use may be explained by this study. In other words,
the information included in this study describes the
outcome at a considerable level. These results showed
up in similar studies, where the hypothesized model
accounted for 56 % of the variance in behavioral
intention to use by young users’ of a health
information portal (Tao et al, 2020) and elsewhere
57.1% of the variance in behavioral intention to use
diabetes management apps (Zhang et al, 2019).
7 CONCLUSION AND
LIMITATIONS
Wrapping up our results, the descriptive analysis
followed by a statistical study were successful in
detecting that the intention to use TDM among the
Lebanese youth is considerable – 64% of the
informants have indicated their readiness to use today
and 57% stated their intent to use it in the future.
Information from this study indicates that marital
status is most likely a factor for intention to use of
TDM among students – whereby, most single are
ready now (65%) while most married students will
tend to use it in the future (67%). The study also
informs that the Lebanese youth prioritize result
demonstrability as a factor in their intention to use
TDM. Further, Mobile TDM must save them time
must be easy to use to be perceived useful.
The manuscript has merit in addressing an
interesting topic through an empirical pilot research.
That said, the fact that the sample is composed by
students at a single university is a limitation of the
study. Other limitations are related to the gender
distribution (83% female and 17% male) to the
prevalence of medical and health students (i.e., almost
50% of the sample). This pilot survey adds
observations and findings that should be useful
among researchers and practitioners. A qualitative
study is encouraged to extend this pilot into a deeper
understanding of factors that influence the intention
to use. This work is extensible to a wider population
of different age groups and occupations, in a valuable
comparative of addressable markets and target user
base that could provide insight for manufacturers and
practitioners alike.
REFERENCES
Abbott, L. (2020) M., Miller, R., Janda, M., Bennett, H.,
Taylor, M., Arnold, C., Shumack, S., Soyer, H. P., &
Caffery, L. J. (n.d.). Practice guidelines for
teledermatology in Australia. Australasian Journal of
Dermatology.
Aggelidis, V. P., & Chatzoglou, P. D. (2009). Using a
modified technology acceptance model in hospitals. Int.
J. Med. Inform, 78(2), 115-126.
Ajzen, I. (2011). The theory of planned behaviour:
Reactions and reflections. Psychology & Health, 26(9),
1113–1127.
Cartron, A. M., Rismiller, K., & Trinidad, J. C. L. (2020).
Store‐and‐forward Teledermatology in the era of
COVID‐19: A Pilot Study. Dermatologic Therapy.
Cepeda-Carrion, G., Cegarra-Navarro, J. G., & Cillo, V.
(2019). Tips to use partial least squares structural
equation modelling (PLS-SEM) in knowledge
management. Journal of Knowledge Management.
Chau, P. Y., & Hu, P. J. H. (2002). Investigating healthcare
professionals’ decisions to accept telemedicine
technology: an empirical test of competing theories.
Information & management, 39(4), 297-311.
Davis, F. D. (1989). Perceived usefulness, perceived ease of
use, and user acceptance of information technology.
MIS quarterly, 319-340.
HEALTHINF 2022 - 15th International Conference on Health Informatics
22

Deng, Z., Hong, Z., Ren, C., Zhang, W., & Xiang, F. (2018).
What predicts patients’ adoption intention toward
mHealth services in China: empirical study. JMIR
mHealth and uHealth, 6(8), e172.
Desai, B., McKoy, K., & Kovarik, C. (2010). Overview of
international teledermatology. The Pan African Medical
Journal, 6.
Eedy, D. J., & Wootton, R. (2001). Teledermatology: a
review. British Journal of Dermatology, 144(4),
696707.
Ferlay J, Colombet M, Soerjomataram I, et al. Global and
Regional Estimates of the Incidence and Mortality for
38 Cancers: GLOBOCAN 2018. International Agency
for Research on Cancer/World Health Organization;
2018.
Garavand, A., Mohseni, M., Asadi, H., Etemadi, M.,
Moradi-Joo, M., & Moosavi, A. (2016). Factors
influencing the adoption of health information
technologies: a systematic review. Electronic physician,
8(8), 2713.
Giavina Bianchi, M., Santos, A., & Cordioli, E. (2021).
Dermatologists’ perceptions on the utility and
limitations of teledermatology after examining 55,000
lesions. Journal of telemedicine and telecare, 27(3),
166-173.
Gorrepati, P. L., & Smith, G. P. (2020). Evaluating the
dermatology communities’ public health response to
COVID-19. Dermatologic Therapy, 33(4), e13775.
Hair, J. F., Risher, J. J., Sarstedt, M., & Ringle, C. M.
(2019). When to use and how to report the results of
PLS-SEM. European business review.
Hazzi, O., & Maldaon, I. (2015). A pilot study: Vital
methodological issues. Business: Theory and Practice,
16(1), 53-62.
Holden, R. J., & Karsh, B. T. (2010). The technology
acceptance model: its past and its future in health care.
Journal of biomedical informatics, 43(1), 159-172.
Horsham, C., Loescher, L. J., Whiteman, D. C., Soyer, H.
P., & Janda, M. (2016). Consumer acceptance of
patient-performed mobile teledermoscopy for the early
detection of melanoma. British Journal of
Dermatology,175(6),1301–1310.
https://doi.org/10.1111/bjd.14630 Hu, P. J., Chau, P.
Y., Sheng, O. R. L., & Tam, K. Y. (1999). Examining
the technology acceptance model using physician
acceptance of telemedicine technology. J Manag Inf
Syst, 16(2), 91-112
Im, Il & Kim, Yongbeom & Han, Hyojoo. (2008). The
effects of perceived risk and technology type on users’
acceptance of technologies. Information &
Management.
Jolliffe, V. M., Harris, D. W., & Whittaker, S. J. (2001). Can
we safely diagnose pigmented lesions from stored video
images? A diagnostic comparison between clinical
examination and stored video images of pigmented
lesions removed for histology. Clinical and
Experimental Dermatology, 26(1), 84–87.
Jr, H., Risher, J., Sarstedt, M., & Ringle, C. (2018). When
to use and how to report the results of PLS-SEM.
European Business Review, 31.
Kamal, S. A., Shafiq, M., & Kakria, P. (2020). Investigating
acceptance of telemedicine services through an
extended technology acceptance model (TAM).
Technology in Society, 60, 101212
Ketikidis, P., Dimitrovski, T., Lazuras, L., & Bath, P. A.
(2012). Acceptance of health information technology in
health professionals: An application of the revised
technology acceptance model. Health Informatics
Journal, 18(2), 124–134.
Kock, N., & Hadaya, P. (2018). Minimum sample size
estimation in PLS‐SEM: The inverse square root and
gamma‐exponential methods. Information Systems
Journal, 28(1), 227-261.
Koonin, L. M. (2020). Trends in the Use of Telehealth
During the Emergence of the COVID-19 Pandemic—
United States, January–March 2020. MMWR.
Lee, J. J., & English, J. C. (2018). Teledermatology: a
review and update. American journal of clinical
dermatology, 19(2), 253-260.
Lee, J. J., & English, J. C. (2018). Teledermatology: a
review and update. American journal of clinical
dermatology, 19(2), 253-260.
Livingstone, J., & Solomon, J. (2015). An assessment of the
cost-effectiveness, safety of referral and patient
satisfaction of a general practice teledermatology
service. London Journal of Primary Care, 7(2), 31–35.
Massone, C., Maak, D., Hofmann‐Wellenhof, R., Soyer, H.
P., & Frühauf, J. (2014). Teledermatology for skin
cancer prevention: An experience on 690 Austrian
patients. Journal of the European Academy of
Dermatology and Venereology, 28(8), 1103–1108.
McGee, J. S., Reynolds, R. V., & Olbricht, S. M. (2020).
Fighting COVID-19: Early teledermatology lessons
learned. Journal of the American Academy of
Dermatology, 83(4), 1224–1225.
Moph. (n.d.). Retrieved July 10, 2020, from
http://www.moph.gov.lb
Morbidity and Mortality Weekly Report, 69. Retrieved
November 29, 2020,
Mostafa, P. I. N., & Hegazy, A. A. (2020). Dermatological
consultations in the COVID-19 era: Is teledermatology
the key to social distancing? An Egyptian experience.
Journal of Dermatological Treatment, 1–6.
Nicholson, P., Macedo, C., Fuller, C., & Thomas, L. (2020).
Patient satisfaction with a new skin cancer
teledermatology service. Clinical and experimental
dermatology, 45(6), 691-698.
Rahimi, B., Nadri, H., Afshar, H. L., & Timpka, T. (2018).
A systematic review of the technology acceptance
model in health informatics. Applied clinical
informatics, 9(03), 604-634.
Romero, G., de Argila, D., Ferrandiz, L., Sánchez, M. P.,
Vañó, S., Taberner, R., ... & Moreno-Ramírez, D.
(2018). Practice models in teledermatology in Spain:
longitudinal study, 2009-2014. Actas Dermo-
Sifiliográficas (English Edition), 109(7), 624-630.
Sáenz, J. P., Novoa, M. P., Correal, D., & Eapen, B. R.
(2018). On using a mobile application to support
teledermatology: a case study in an underprivileged area
Factors Influencing Tele-dermatology Adoption among the Lebanese Youth: A Pilot Study at Saint Joseph University
23

in Colombia. International journal of telemedicine and
applications, 2018.
Shaarani, I., Ghanem, A., Jounblat, M., Jounblat, H.,
Mansour, R., & Taleb, R. (2021). Utilization of
Telemedicine by the Lebanese Physicians During Time
of Pandemic. Telemedicine and e-Health.
Sung, H, Ferlay, J, Siegel, RL, Laversanne, M,
Soerjomataram, I, Jemal, A, Bray, F. Global cancer
statistics 2020: GLOBOCAN estimates of incidence
and mortality worldwide for 36 cancers in 185
countries. CA Cancer J Clin. 2021: 71: 209- 249.
Szajna, B. (1996). Empirical evaluation of the revised
technology acceptance model. Management science,
42(1), 85-92.
Tao, D., Shao, F., Wang, H., Yan, M., & Qu, X. (2020).
Integrating usability and social cognitive theories with
the technology acceptance model to understand young
users’ acceptance of a health information portal. Health
informatics journal, 26(2), 1347-1362.
Venkatesh V, Morris MG, Davis GB, et al. User acceptance
of information technology: toward a unified view. MIS
Quarterly 2003; 27: 425–478.
Venkatesh, V., & Davis, F. (2000). A Theoretical Extension
of the Technology Acceptance Model: Four
Longitudinal Field Studies. Management Science, 46,
186–204.
Vidal-Alaball, J., Garcia Domingo, J. L., Garcia Cuyàs, F.,
Mendioroz Peña, J., Flores Mateo, G., Deniel
Wang, R. H., Barbieri, J. S., Nguyen, H. P., Stavert, R.,
Forman, H. P., Bolognia, J. L., & Kovarik, C. L.
(2020a). Clinical effectiveness and cost-effectiveness of
teledermatology: Where are we now, and what are the
barriers to adoption? Journal of the American Academy
of Dermatology, 83(1), 299–307.
Whited, J. D. (2006). Teledermatology research review.
International journal of dermatology, 45(3), 220-229.
Yang, X., Barbieri, J. S., & Kovarik, C. L. (2019). Cost
analysis of a store-and-forward teledermatology consult
system in Philadelphia. Journal of the American
Academy of Dermatology, 81(3), 758–764.
Zhang, Y., Liu, C., Luo, S., Xie, Y., Liu, F., Li, X., & Zhou,
Z. (2019). Factors Influencing Patients’ Intentions to
Use Diabetes Management Apps Based on an Extended
Unified Theory of Acceptance and Use of Technology
Model: Web-Based Survey. Journal of Medical Internet
Research, 21(8), e15023. https://doi.org/10.2196/15023
APPENDIX
Survey Questions and Possible Answers
1- Gender: Male, Female
2- Age: < 20 years; 21 – 25; 26 – 30; 31 – 35; 36 – 40; 41 – 45; Above 46
3- Education specialty: Business Management; Engineering & Sciences; Humanities; Medical & Health; Political Science
& Law; Other
4- Work: Part time; Full time; Other or Null
5- Marital status: Single; Married
6- Skin colour: Fair; Medium; Dark
7- Eye colour: Brown; Hazel; Blue; Green; Other or Null
8- Family history of skin cancer: No; Yes
9- Previous skin cancer removed: No; Yes
10- Presence of moles larger than 2 mm: None; Less than 10; 11+
11- Mobile Teledermatology will help me examine my skin more rapidly: Strongly agree; Agree; Unsure; Disagree; Strongly
disagree
12- Mobile Teledermatology will improve my self-skin examination: Strongly agree; Agree; Unsure; Disagree; Strongly
disagree
13- Mobile Teledermatology is useful to diagnose moles on my skin for suspicious lesions: Strongly agree; Agree; Unsure;
Disagree; Strongly disagree
14- Mobile Teledermatology will help save time: Strongly agree; Agree; Unsure; Disagree; Strongly disagree
15- Mobile Teledermatology will help detect skin cancer in early stages: Strongly agree; Agree; Unsure; Disagree; Strongly
disagree
16- Mobile Teledermatology will be easy to use: Strongly agree; Agree; Unsure; Disagree; Strongly disagree
17- A suspicious mole or lesion diagnosis through Mobile Teledermatology will be understandable: Strongly agree; Agree;
Unsure; Disagree; Strongly disagree
18- Mobile Teledermatology users will easily acquire the skills to preform it: Strongly agree; Agree; Unsure; Disagree;
Strongly disagree
19- Mobile Teledermatology will encourage me to examine my skin thoroughly: Strongly agree; Agree; Unsure; Disagree;
Strongly disagree
HEALTHINF 2022 - 15th International Conference on Health Informatics
24

20- The use of Mobile Teledermatology will change my self-skin examination practice: Strongly agree; Agree; Unsure;
Disagree; Strongly disagree
21- The use of Mobile Teledermatology can fit in my skin examination habit: Strongly agree; Agree; Unsure; Disagree;
Strongly disagree
22- The use of Mobile Teledermatology may interfere with my work: Strongly agree; Agree; Unsure; Disagree; Strongly
disagree
23- I will use Mobile Teledermatology when its offered to me: Strongly agree; Agree; Unsure; Disagree; Strongly disagree
24- I will use Mobile Teledermatology in my routine self-skin examination in the future: Strongly agree; Agree; Unsure;
Disagree; Strongly disagree
25- I will use Mobile Teledermatology if it will save me time: Strongly agree; Agree; Unsure; Disagree; Strongly disagree
26- I will use Mobile Teledermatology if it will save me money: Strongly agree; Agree; Unsure; Disagree; Strongly disagree
27- Mobile Teledermatology will be useful to diagnose skin cancer in general: Strongly agree; Agree; Unsure; Disagree;
Strongly disagree
28- Mobile Teledermatology will be for my best interest: Strongly agree; Agree; Unsure; Disagree; Strongly disagree
29- Health professionals (nurses, physicians...) will welcome the fact that I use Mobile Teledermatolog: Strongly agree;
Agree; Unsure; Disagree; Strongly disagree y
30- My friends and my family will welcome the fact that I use Mobile Teledermatology: Strongly agree; Agree; Unsure;
Disagree; Strongly disagree
31- I will completely trust the diagnosis of the dermatologist based on a photo I’ve sent using Mobile Teledermatology:
Strongly agree; Agree; Unsure; Disagree; Strongly disagree
32- I will rely on the Teledermatology process to supply accurate information about a mole or a spot: Strongly agree; Agree;
Unsure; Disagree; Strongly disagree
33- I will use Mobile Teledermatology if I receive adequate training: Strongly agree; Agree; Unsure; Disagree; Strongly
disagree
34- I will use Mobile Teledermatology if I receive technical assistance when I need it : Strongly agree; Agree; Unsure;
Disagree; Strongly disagree
35- There are health professionals available who will help me with Mobile Teledermatology: Strongly agree; Agree; Unsure;
Disagree; Strongly disagree
Factors Influencing Tele-dermatology Adoption among the Lebanese Youth: A Pilot Study at Saint Joseph University
25
