
Identifying Sociodemographic Factors for a User Engaging Type 2
Diabetes Mellitus Mobile Self-management Application
Kuthethur Sneha Jagannath Das and Felix Janszen
Inpaqt Technology Solutions B.V., 16, Marconistraat, 3029 AK, Rotterdam, The Netherlands
Keywords: Type 2 Diabetes Mellitus, Mobile Health, User Engagement, Sociodemographic Factors, Behavior Change.
Abstract: Type 2 Diabetes Mellitus(T2DM) is a chronic condition affecting the elderly population across the globe.
Self-management from the patient’s side is a key factor for T2DM care. Growth in the information and
communication technology field has paved way for the rise of digital health interventions. Digital health
interventions (DHI) can support self-management behaviors in patients suffering from chronic conditions
through health coaching. Patient Engagement with DHI is crucial for the intervention to be effective on the
patient’s health. This paper discusses user engagement and focuses explicitly on identifying the
sociodemographic factors impacting user engagement with a mobile health intervention (mHealth) in T2DM
patients. The factors along with their interrelations have been identified through expert reviews, feedback
from T2DM patients and their family member through questionnaires and think aloud interview, and the
conduction of a literature study.
1 INTRODUCTION
Type 2 Diabetes Mellitus(T2DM) is a highly prevalent
chronic condition across the globe. By 2040, T2DM is
estimated to be prevalent in 642 million people
globally (den Braber et al., 2019). Prevalence of
T2DM is a risk factor for several comorbidities and
health complications such as obesity, cardiovascular
diseases, renal failure, and blindness to name a few,
and poses a burden on the healthcare system (Pardhan
et al., 2020; Stühmann et al., 2020; Sun et al., 2019).
Immense advancements in medical technology
have led to the growth of telemedicine. Telemedicine
is the crux of mHealth interventions, a subset of DHI
(Shan et al., 2019). Studies have shown that DHI
support the management of chronic conditions in a
home setting (Maresca et al., 2019). mHealth
implemented through smartphone applications (app)
and wearable can be personalized (Shan et al., 2019).
In T2DM management, the goal is to achieve and
maintain the blood glucose level (BGL) within the
optimal range (den Braber et al., 2019; Shan et al.,
2019). Pursuit of sufficient and regular physical
activity (PA), healthy diet, prescribed medication
(insulin doses) intake, sufficient sleep, stress
management and regular BGL monitoring are factors
integral to optimal T2DM management (den Braber et
al., 2019; Grandner et al., 2016; Shan et al., 2019;
Simon et al., 2014). These can be understood as
lifestyle factors (den Braber et al., 2019; Schoeppe et
al., 2016). Studies show that self-management is a
cornerstone for holistic T2DM management (Izahar et
al., 2017). Health coaching can support in facilitating
self-management (Gupta et al., 2018).
Health coaching involves targeting and improving
poor health behaviors such as lack of pursuit of PA,
smoking, and eating an unhealthy meal (Gupta et al.,
2018; Snaith et al., 2018). Previous studies reveal that
mHealth facilitates self-management of T2DM and is
effective in supporting the individual to maintain an
optimal BGL (Boyle., 2017; Kebede & Pischke, 2019;
Murray et al., 2016). Studies also suggest that an
engaging mHealth intervention is a prerequisite for
achieving the health effectiveness (Agarwal et al.,
2019; Yardley et al., 2016).
Despite this significant advantage of mHealth in
T2DM care, T2DM app usage in an individual’s daily
use scenario is not prevalent (Kebede & Pischke,
2019). Findings from literature show that lack of
thorough evidence in the areas of behavior change
models, less clinical focus addressed in the app
development, and minimal integration of T2DM care
functionalities in a single application (app) could be
some possible reasons (den Braber et al., 2019;
Helbostad et al., 2017; Yardley et al., 2016).
254
Das, K. and Janszen, F.
Identifying Sociodemographic Factors for a User Engaging Type 2 Diabetes Mellitus Mobile Self-management Application.
DOI: 10.5220/0011062800003188
In Proceedings of the 8th International Conference on Information and Communication Technologies for Ageing Well and e-Health (ICT4AWE 2022), pages 254-260
ISBN: 978-989-758-566-1; ISSN: 2184-4984
Copyright
c
2022 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
Hence, our goal in this project is to develop an
engaging mHealth app that is science-based,
evidence-based, and artificial intelligence (AI) driven,
supporting T2DM patients to self-manage their
condition in a remote setting. This paper solely
focuses on addressing the question of what
sociodemographic factors contribute to developing a
user engaging mHealth app that would support T2DM
patients in maintaining their BGL within the target
range.
In the beginning of this project, during the
conduction of an expert stakeholder analysis, the
possibility of sociodemographic factors affecting the
user engagement with the app was addressed. Hence,
that was taken as one of the problem statements in the
pursuit of this project. To solve this, a thorough
literature study was conducted followed by interaction
with T2DM patients and caregivers through
questionnaires and think aloud interview.
2 BACKGROUND
Diabetes education is closely related to the self-
management of T2DM as it induces self-care
behaviors in the individual (Kebede & Pischke, 2019;
Weston et al., 2015). Diabetes education includes
equipping the patient with knowledge about T2DM,
complications of T2DM, and the patient’s progress in
T2DM management (Weston et al., 2015). Education
about the health condition and self-awareness about
the progress is an integral part of health coaching
process. And this is associated with positive
engagement with the DHI and thus effectiveness on
the individual’s health (Weston et al., 2015; Yardley
et al.,2016) Enabling the patient with relevant and
timely health information is an essential benefit seen
in mHealth app adoption (Shan et al., 2019).
One aspect of engagement is related to the user’s
interaction with the digital intervention and is defined
as the “quality of user’s experience with technology”
(O’Brien & Cairns, 2015; O'Brien & Toms, (2008).
To address this definition of engagement, some
aspects such as feedback, awareness, aesthetics,
attention, interactivity, and challenge are considered
in building an engaging technology (O’Brien &
Cairns, 2015; O'Brien & Toms, (2008).
Another aspect of engagement with digital health
interventions focuses on the patient’s engagement
with the process of achieving behavioral and
physiological change (Yardley et al., 2016). Here,
engagement with a DHI is considered similar to
engaging with face-to- face intervention (Yardley et
al., 2016).
3 METHODS
In this project, the CeHReS roadmap (
Van Velsen et
al., 2013)
is being adopted for developing this T2DM
mHealth app. The initial set of designs were explicitly
focused on the content design of the app. This has
been done by taking into account the various
attributes of health coaching. We will not be
discussing about the app design process further since
it lies outside the scope of this paper.
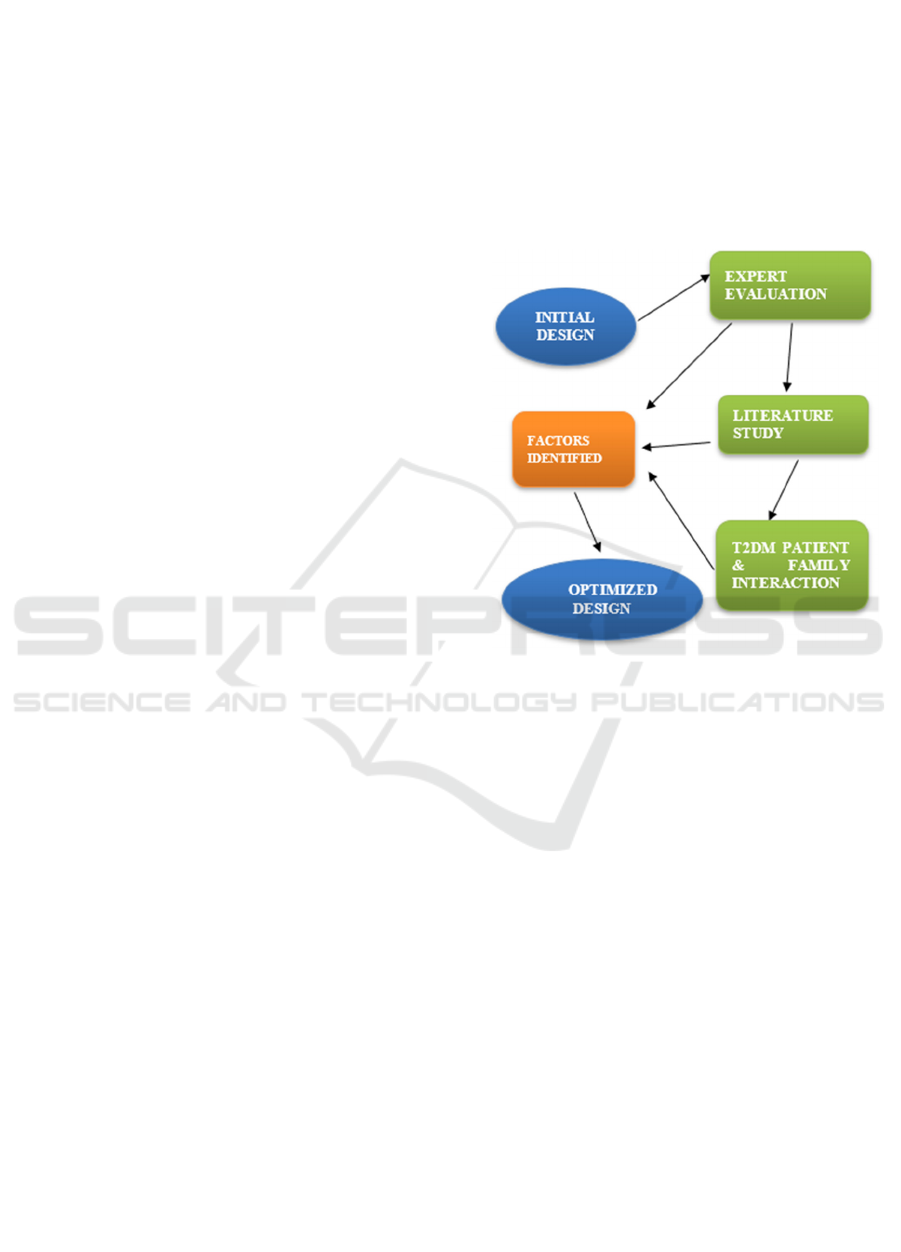
Figure 1: Outline of the steps taken in identifying the
sociodemographic factors affecting user engagement.
As shown in Figure 1, three steps were taken in
identifying the sociodemographic factors influencing
user engagement with the T2DM app. Expert
evaluation on the initial set of designs, literature study
and, questionnaire response by patient and family
caretaker are the three steps. These steps are
described below.
3.1 Expert Stakeholder Evaluation
The initial set of designs were created and as a part of
stakeholder evaluation, a qualitative evaluation with
a group of experts was conducted. In total, five
experts participated in this evaluation. The expert
panel consisted of an mHealth specialist, Artificial
Intelligence (AI) expert, knowledge in the area of
behaviour change, diabetes and pharmacology
specialist, software developer along with a regular
non diabetic fitness app user. To conduct this
evaluation, a short video explaining the core
functionalities of the content design was pre-recorded
and sent to the expert panel prior to the expert session.
This was done one week before the expert session.
Identifying Sociodemographic Factors for a User Engaging Type 2 Diabetes Mellitus Mobile Self-management Application
255

During the expert meet up, the questions related to
engagement aspect were posed and discussed. The
questions discussed are as follows:
1. Do you think the app is engaging to the user?
2. How is sustained engagement affected in
this?
3. What factors can be addressed to make the
app engaging in terms of long-term user
engagement?
3.2 Literature Study
Based on the feedback received in this expert
evaluation session, a decision to update the current
designs based on a revised literature study was taken.
For the literature study, scientific papers from JMIR
(open access journal) were found through the
combination of the following keywords: T2DM,
diabetes, user engagement, mHealth, eHealth,
telemedicine, self-management and social
demographics. This literature study was conducted in
December 2020.
3.3 T2DM Patient and Family
Caretaker Questionnaire
Based on the expert evaluation feedback and
conclusions of the literature study, a decision to
collect insights from the T2DM patients and their
family caretakers was taken. Here, T2DM patients
and family caretakers of T2DM patients were
recruited to participate in a short questionnaire
survey. Two different questionnaires were made. One
was for the T2DM patient and the other was for the
family caretaker. The purpose of the questionnaire
was to understand the interest of the patients and
family in the scope of the app with emphasis on the
role of T2DM care education in remote self-
management and the possible involvement of a
family member as a caregiver in T2DM management.
13 people filled the questionnaire. 4 of them were
patients and 9 of them were family members. In
addition, 1 family member did a think aloud session
for 20 minutes discussing about the designs. The
patients were recruited through acquittances of the
people conducting this research.
With the expert evaluation feedback, the content
analysis results of the literature study and the
questionnaires results along with the think aloud
session, the current designs were further optimized.
In this paper, as illustrated in Figure 1, we report the
findings explicitly focusing on the engagement
dependent on sociodemographic aspect for an optimal
T2DM management.
4 RESULTS
From the methods discussed in the previous section,
three sets of results are obtained. These are discussed
in this section.
4.1 Expert Evaluation
Through the expert evaluation, the scope of user
engagement with the mHealth app was elaborately
explored. All the experts reinforced the point of the
current set of designs being engaging and effective
for the user in T2DM self-management. However, a
strong recommendation was provided by all the
experts to look into the long-term or sustained
engagement aspect. The expert panel felt that factors
such as age, ethnicity, education status, health
literacy, and digital skills could affect user
engagement.
In order to address this, the experts suggested
exploring the possible role of sociodemographic
factors in adopting and engaging with mHealth
technology for successful T2DM self-management.
4.2 Literature Study
For the literature study, ten articles from JMIR were
selected. The ten articles selected focused on T2DM
management via mHealth and eHealth (web-based)
solutions and had at least one barrier listed which
focused on the lack of engagement aspect. The
articles selected are based on studies conducted on
T2DM management through ICT in diverse
geographic locations such as the USA, Canada,
Norway, China and India. In this literature study, ten
barriers affecting the engagement have been
identified. Figure 2 provides an outlook of the
sociodemographic factors identified in the literature
study implementation.
Five articles identified low health literacy as a
barrier affecting the user engagement (Alvarado et
al., 2017; Desveaux et al., 2018; Williams &
Schroeder, 2015; Zhang et al., 2019). When
compared to patients with high health literacy,
patients with low health literacy dropped out of
mHealth and eHealth studies (Alvarado et al., 2017;
Williams & Schroeder, 2015).
Five articles identified ethnicity of the patient as a
barrier in engaging with the developed eHealth and
mHealth solutions for T2DM management (in the
ICT4AWE 2022 - 8th International Conference on Information and Communication Technologies for Ageing Well and e-Health
256
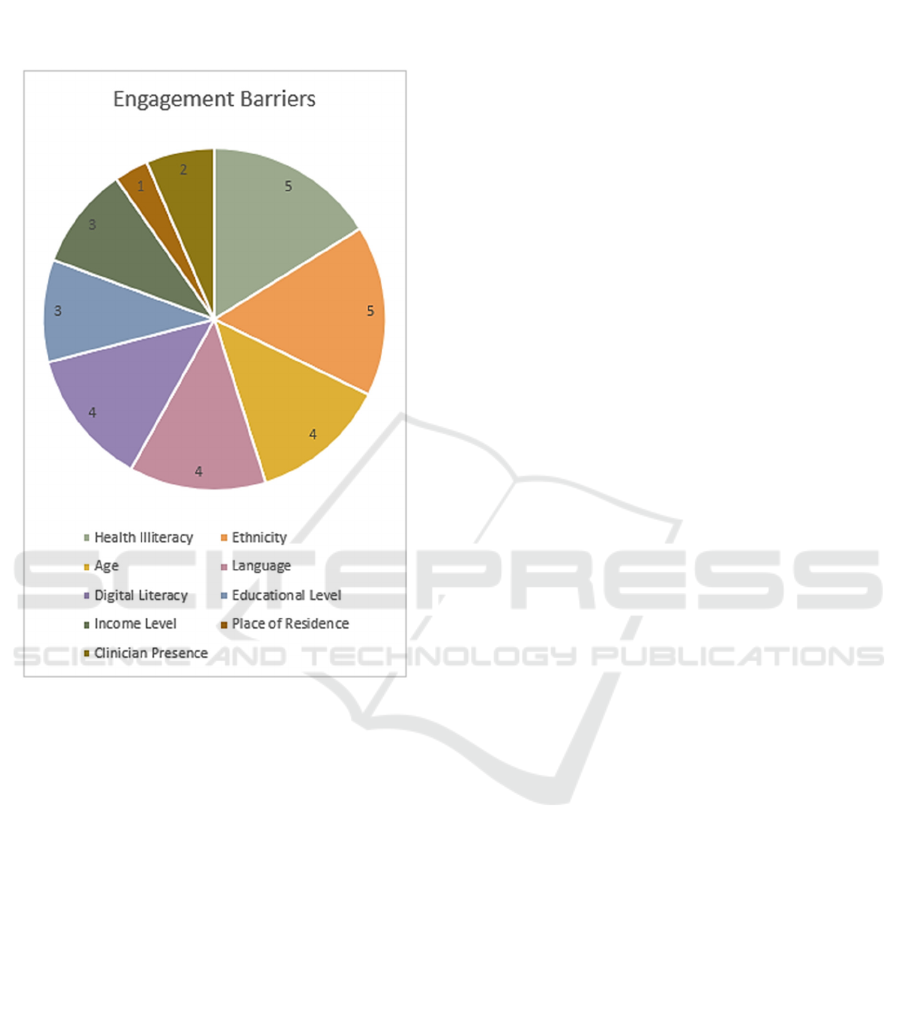
context of this paper, ethnicity can be understood as a
sense of belonging to a particular cultural or social
group) (Huang et al., 2019; Mold et al., 2018;
Muralidharan et al., 2017; Tatara et al., 2019;
Williams & Schroeder, 2015, 2015).
Figure 2: List of barriers affecting T2DM care engagement
of the patient (with their frequency of occurrence).
Four articles identified that age of the patients
affect their engagement with the T2DM care solution.
Elderly people face difficulty in this aspect (Agarwal
et al., 2019; Huang et al., 2019; Peters et al., 2017;
Williams & Schroeder, 2015).
Four articles have identified language as a barrier
in engaging with the T2DM solution (Alvarado et al.,
2017; Mold et al., 2018; Tatara et al., 2019; Williams
& Schroeder, 2015). A study conducted in the U.S.A
identified Latino population residing in the U.S.A had
issues in adopting the eHealth solution as the solution
was in English (Williams & Schroeder, 2015).
Four articles have identified digital or technical
illiteracy as a barrier for a successful engagement
with the T2DM services (Alvarado et al., 2019;
Huang et al., 2019; Peters et al., 2017; Tatara et al.,
2019). T2DM patients with lower digital skills have
dropped out of investigative studies faster in
comparison to patients with higher digital skills.
Three articles have identified educational level as
a barrier in adopting T2DM digital interventions
(Alvarado et al., 2019; Tatara et al., 2019; Williams
& Schroeder, 2015). Educational level has affected
the self-management aspect of T2DM causing lower
engagement in low level educated groups (Alvarado
et al., 2019).
Three articles have identified income level as a
barrier in T2DM ICT-based care (Alvarado et al.,
2019; Mold et al., 2018; Peters et al., 2017). Other
factors include specific lack of knowledge of medical
terms (Mold et al., 2018), cultural awareness
(Alvarado et al., 2019) and place of residence of the
patient (Mold et al., 2018).
Belief in the benefit of the solution (Agarwal et
al., 2019; Desveaux et al., 2018; Huang et al., 2019),
referral of the solution by the clinician team (Agarwal
et al., 2019; Huang et al., 2019) and continuous
interaction between the clinician team and patient
(Agarwal et al., 2019) have also been identified as
barriers for engagement.
Figure 2 shows the list of ten barriers identified in
the ten articles during the implementation of the
literature study. In Figure 2, cultural awareness has
been combined with ethnicity, specific lack of
medical terminology knowledge has been combined
with health illiteracy and the barriers listed in relation
to the clinician and patient engagement have been
grouped under clinician presence.
4.3 Patient and Family Caretaker
Questionnaire
13 participants filled in the questionnaire survey. 4
participants were T2DM patients and 9 participants
were family caretakers of T2DM patients. All the 13
participants were of the Indian origin.
Among the T2DM patients, 3 men and 1 woman
filled in the questionnaire. 2 of the participants have
indicated their age group. One person belonged to the
age group of 50 to 60 and another between 60 to 70
years.
Among the family members who filled in the
questionnaire, two participants were Indians based
out of Germany and the Netherlands. 4 men and 5
women filled in the questionnaire. 3 people were less
than 30 years, one person belonged to the age group
of 30 to 40, 4 of them belonged to the age group of 50
to 60 and one person to the age of 60 to 70.
Out of the 4 T2DM patients, 3 have indicated that
they have good knowledge about T2DM care and 1
patient has indicated that they want to have T2DM
care knowledge. All 4 have indicated that they like
Identifying Sociodemographic Factors for a User Engaging Type 2 Diabetes Mellitus Mobile Self-management Application
257

their family members being involved in the care. Out
of 9 family caretakers, only 2 have indicated that they
have good knowledge about T2DM care, 4 gave a
neutral response and 3 have indicated they don’t have
any knowledge about T2DM care. 7 family caretakers
have indicated that they want to have T2DM care
knowledge. All 9 participants have indicated that they
like to be involved in their family member’s T2DM
care.
One female family member participated in the
think aloud session. She is from India and belonged
to the age group of 50 to 60 years. Her spouse has
T2DM. During the session, she reinforced the idea of
the app was good and needed in T2DM management.
Further, she provided insights into how the health
information can be conveyed better to a potential user
based on the current content design of the app.
5 DISCUSSION
From the feedback received in the expert panel
discussion for the initial set of T2DM mHealth app
designs, the literature study implementation and the
interaction with T2DM patients and family caretakers
through questionnaires and interview,
sociodemographic factors which influence the user
engagement were identified.
Some of the factors identified during the expert
panel discussion are concurrent to the factors
identified during the implementation of the literature
study. These were the factors of age, education level,
health illiteracy, and digital illiteracy.
From the results of the literature study, it can be
understood that the factors are related to each other.
For instance, the article by (Williams& Schroeder,
2015) identified health illiteracy, age, language,
ethnicity and education level as barriers to the user
engagement. The article by (Alvarado et al., 2017)
identified health illiteracy, language, digital literacy,
education level, and cultural awareness as factors of
barrier for the user engagement. Articles by (Tatara et
al., 2019; Williams& Schroeder, 2015) reveal that
immigrant populations who form the minority ethnic
groups and Hispanic population in the U.S.A. face the
concerns of health illiteracy.
From the expert panel discussion, it was realized
design in terms of aspects such as aesthetics, feedback
or challenge alone would not be sufficient in
engaging the user. From literature, it can be
understood that these aspects arise from the definition
of engagement that is inclined towards the quality of
the user experience with the digital intervention and
focus on the initial reaction of the user to the digital
intervention (O’Brien & Cairns, 2015; O'Brien &
Toms, (2008).
The panel discussion yielded a strong conclusion
that inclusion of sociodemographic elements and
clinician presence to the existing design which
already focused on the areas of aesthetics and
feedback would benefit the part of user engagement.
The findings from the literature study implemented
also concurs with this.
In the work of (Yardley et al.,2016), “engagement
is understood as a dynamic process which involves a
trigger, followed with an initial use by the patient,
which may further lead to a sustained engagement,
disengagement or maybe a shift to another
intervention”. Thus, it can be realized that for
engagement to be effective, it should satisfy the
criterion of engagement with technology and
engagement with the behavior change pursuit
(O’Brien & Cairns, 2015; Yardley et al.,2016).
From the previous sections, it can be understood
that self-management is crucial for successful T2DM
management and diabetes education is an important
part of self-management as it plays a role in inducing
self-care behaviors in the patient.
The article by (Yardley et al., 2016) emphasizes
that digital health interventions need to address the
target group of people with low health literacy and
include design solutions to alleviate health illiteracy.
Health literacy focuses on the aspects of applying
knowledge and the ability to access, understand and
apply health-related information.
Interaction with subjects is an inherent component
of CeHReS roadmap as it is based on human centred
design. In the expert session, the experts strongly
recommended to address countries in Asia and Africa
as it would give a global perspective in the project.
Hence, as an initial step, the patient interaction took
place with the Indian patients and family members.
Although the number of participants were less, the
feedback from the participants concurred with the
expert evaluation feedback and literature study. The
insights from the questionnaire response of T2DM
patients and family caretakers also indicate that
knowledge of T2DM care would support optimal
T2DM self-care. These responses concur with the
feedback of expert session and literature study.
From the conclusions of the expert session, the
conduction of literature study and, responses of
T2DM patients and family caretakers, we realize the
role of health literacy in T2DM management. Hence,
in this paper, we come to the conclusion of health
illiteracy about T2DM being the most crucial factor
among the list of sociodemographic factors
ICT4AWE 2022 - 8th International Conference on Information and Communication Technologies for Ageing Well and e-Health
258

identified, which affects the user engagement with the
T2DM mHealth app intervention.
In the next phase of our project, we are optimizing
the initial set of designs by modelling the
sociodemographic factors into an Artificial
Intelligence model to drive the app content and
explicitly focus on addressing the T2DM education
aspect through chatbots and avatars (Das et al., 2019).
From the questionnaire, it was understood that family
caretaker also forms an important stakeholder group
and hence they would be included in the mHealth
intervention along with the physician team. The
designs would be developed into a functional
prototype and would be tested as a part of iterative
longitudinal studies with T2DM patients, their family
caretakers and clinician for aspects of usability,
sustained user engagement, and T2DM management
effectiveness.
6 CONCLUSIONS
The objective of this paper was to identify the
sociodemographic factors affecting user engagement
of a T2DM patient with an mHealth T2DM
intervention. Health illiteracy, digital literacy,
education level, age, ethnicity, language, place of
residence, income level, cultural awareness and
patient clinician interaction were found to be the
barriers for an effective user engagement with the
mHealth intervention.
Health illiteracy was identified as a crucial factor
in affecting the user engagement as it is closely linked
to diabetes education, an integral feature of self-
managing T2DM. These engagement barriers were
identified through an expert panel discussion,
followed with a literature study implementation and
questionnaire responses from T2DM patients and
family members.
ACKNOWLEDGEMENTS
We thank the participants of the expert session and
the T2DM patients and family caretakers who
interacted with us on the scope of this mHealth
intervention through questionnaire and think aloud
session.
REFERENCES
Agarwal, P., Mukerji, G., Desveaux, L., Ivers, N. M.,
Bhattacharyya, O., Hensel, J. M., & Bhatia, R. S.
(2019). Mobile app for improved self-management of
type 2 diabetes: multicenter pragmatic randomized
controlled trial. JMIR mHealth and uHealth, 7(1),
e10321.
Alvarado, M. M., Kum, H. C., Coronado, K. G., Foster, M.
J., Ortega, P., & Lawley, M. A. (2017). Barriers to
remote health interventions for type 2 diabetes: a
systematic review and proposed classification scheme.
Journal of medical Internet research, 19(2), e28.
Boyle, L., Grainger, R., Hall, R. M., & Krebs, J. D. (2017).
Use of and beliefs about mobile phone apps for diabetes
self-management: surveys of people in a hospital
diabetes clinic and diabetes health professionals in New
Zealand. JMIR mHealth and uHealth, 5(6), e85.
Das, K. S. J., Beinema, T., Op Den Akker, H., & Hermens,
H. (2019, May). Generation of Multi-Party Dialogues
among Embodied Conversational Agents to Promote
Active Living and Healthy Diet for Subjects Suffering
from Type 2 Diabetes. In ICT4AWE (pp. 297-304).
den Braber, N., Vollenbroek-Hutten, M.M., Oosterwijk,
M.M., Gant, C.M., Hagedoorn, I.J., van Beijnum,
B.J.F., Hermens, H.J. and Laverman, G.D., 2019.
Requirements of an application to monitor diet,
physical activity and glucose values in patients with
type 2 diabetes: The diameter. Nutrients, 11(2), p.409
Desveaux, L., Shaw, J., Saragosa, M., Soobiah, C., Marani,
H., Hensel, J., & Jeffs, L. (2018). A mobile app to
improve self-management of individuals with type 2
diabetes: qualitative realist evaluation. Journal of
medical Internet research, 20(3), e81.
Grandner, M. A., Seixas, A., Shetty, S., & Shenoy, S.
(2016). Sleep duration and diabetes risk: population
trends and potential mechanisms. Current diabetes
reports, 16(11), 106.
Gupta, I., Di Eugenio, B., Ziebart, B., Liu, B., Gerber, B.,
Sharp, L., & Baiju, A. (2018, June). Towards building
a virtual assistant health coach. In 2018 IEEE
International Conference on Healthcare Informatics
(ICHI) (pp. 419-421). IEEE.
Helbostad, J. L., Vereijken, B., Becker, C., Todd, C.,
Taraldsen, K., Pijnappels, M., & Mellone, S. (2017).
Mobile health applications to promote active and
healthy ageing. Sensors, 17(3), 622.
Huang, Z., Tan, E., Lum, E., Sloot, P., Boehm, B. O., &
Car, J. (2019). A smartphone app to improve
medication adherence in patients with type 2 diabetes
in Asia: feasibility randomized controlled trial. JMIR
mHealth and uHealth, 7(9), e14914.
Izahar, S., Lean, Q. Y., Hameed, M. A., Murugiah, M. K.,
Patel, R. P., Al-Worafi, Y. M., & Ming, L. C. (2017).
Content analysis of mobile health applications on
diabetes mellitus. Frontiers in Endocrinology, 8, 318.
Kebede, M.M. and Pischke, C.R., 2019. Popular diabetes
apps and the impact of diabetes app use on self-care
behaviour: a survey among the digital community of
Identifying Sociodemographic Factors for a User Engaging Type 2 Diabetes Mellitus Mobile Self-management Application
259

persons with diabetes on Social Media. Frontiers in
Endocrinology, 10, p.135.
Maresca, G., De Cola, M. C., Caliri, S., De Luca, R.,
Manuli, A., Scarcella, I., ... & Bramanti, A. (2019).
Moving towards novel multidisciplinary approaches for
improving elderly quality of life: The emerging role of
telemedicine in Sicily. Journal of telemedicine and
telecare, 25(5), 318-324.
Mold, F., Raleigh, M., Alharbi, N. S., & de Lusignan, S.
(2018). The impact of patient online access to
computerized medical records and services on type 2
diabetes: systematic review. Journal of medical
Internet research, 20(7), e235.
Muralidharan, S., Mohan, V., Anjana, R. M., Jena, S.,
Tandon, N., Allender, S., & Ranjani, H. (2017). Mobile
health technology (mDiab) for the prevention of type 2
diabetes: protocol for a randomized controlled trial.
JMIR research protocols, 6(12), e242.
Murray, E., Hekler, E. B., Andersson, G., Collins, L. M.,
Doherty, A., Hollis, C., & Wyatt, J. C. (2016).
Evaluating digital health interventions: key questions
and approaches.
O’Brien, H., & Cairns, P. (2015). An empirical evaluation
of the User Engagement Scale (UES) in online news
environments. Information Processing & Management,
51(4), 413-427.
O'Brien, H. L., & Toms, E. G. (2008). What is user
engagement? A conceptual framework for defining user
engagement with technology. Journal of the American
society for Information Science and Technology, 59(6),
938-955.
Pardhan, S., Nakafero, G., Raman, R. and Sapkota, R.,
2020. Barriers to diabetes awareness and self-help are
influenced by people's demographics: perspectives of
South Asians with type 2 diabetes. Ethnicity & Health,
25(6), pp.843-861.
Peters, R. M., Lui, M., Patel, K., Tian, L., Javaherian, K.,
Sink, E., & Bernal-Mizrachi, C. (2017). Improving
glycemic control with a standardized text-message and
phone-based intervention: a community
implementation. JMIR diabetes, 2(2), e15.
Schoeppe, S., Alley, S., Van Lippevelde, W., Bray, N. A.,
Williams, S. L., Duncan, M. J., & Vandelanotte, C.
(2016). Efficacy of interventions that use apps to
improve diet, physical activity and sedentary
behaviour: a systematic review. International Journal
of Behavioral Nutrition and Physical Activity, 13(1),
127.
Shan, R., Sarkar, S., & Martin, S. S. (2019). Digital health
technology and mobile devices for the management of
diabetes mellitus: state of the art. Diabetologia, 62(6),
877-887.
Simon, A. C., Gude, W. T., Holleman, F., Hoekstra, J. B.,
& Peek, N. (2014). Diabetes patients' experiences with
the implementation of insulin therapy and their
perceptions of computer-assisted self-management
systems for insulin therapy. Journal of medical Internet
research, 16(10), e235.
Snaith, M., De Franco, D., Beinema, T., Den Akker, H. O.,
& Pease, A. (2018). A dialogue game for multi-party
goal-setting in health coaching. In 7th International
Conference on Computational Models of Argument,
COMMA 2018 (pp. 337-344). IOS Press
Stühmann, L. M., Paprott, R., Heidemann, C., Baumert, J.,
Hansen, S., Zahn, D., & Gellert, P. (2020). Health App
Use and Its Correlates Among Individuals With and
Without Type 2 Diabetes: Nationwide Population-
Based Survey. JMIR Diabetes, 5(2), e14396.
Sun, C., Sun, L., Xi, S., Zhang, H., Wang, H., Feng, Y., &
Wang, G. (2019). Mobile phone–based telemedicine
practice in older chinese patients with type 2 diabetes
mellitus: randomized controlled trial. JMIR mHealth
and uHealth, 7(1), e10664.
Tatara, N., Hammer, H. L., Mirkovic, J., Kjøllesdal, M. K.
R., & Andreassen, H. K. (2019). Associations Between
Immigration-Related User Factors and eHealth
Activities for Self-Care: Case of First-Generation
Immigrants From Pakistan in the Oslo Area, Norway.
JMIR public health and surveillance, 5(3), e11998.
Van Velsen, L., Wentzel, J., & Van Gemert-Pijnen, J. E.
(2013). Designing eHealth that matters via a
multidisciplinary requirements development approach.
JMIR research protocols, 2(1), e2547.
Weston, A., Morrison, L., Yardley, L., Van Kleek, M., &
Weal, M. (2015). Measurements of engagement in
mobile behavioural interventions?.
Williams, J. P., & Schroeder, D. (2015). Popular glucose
tracking apps and use of mHealth by Latinos with
diabetes. JMIR mHealth and uHealth, 3(3), e84.
Yardley, L., Spring, B. J., Riper, H., Morrison, L. G., Crane,
D. H., Curtis, K., & Blandford, A. (2016).
Understanding and promoting effective engagement
with digital behavior change interventions. American
journal of preventive medicine, 51(5), 833-842.
ICT4AWE 2022 - 8th International Conference on Information and Communication Technologies for Ageing Well and e-Health
260
