
Overview of the SMART-BEAR Technical Infrastructure
Vadim Peretokin
1
, Ioannis Basdekis
2
, Ioannis Kouris
3
, Jonatan Maggesi
4
, Mario Sicuranza
5
, Qiqi Su
6
,
Alberto Acebes
7
, Anca Bucur
1
, Vinod Jaswanth Roy Mukkala
4
, Konstantin Pozdniakov
6
,
Christos Kloukinas
6
, Dimitrios D. Koutsouris
3
, Elefteria Iliadou
8
, Ioannis Leontsinis
9
, Luigi Gallo
5
,
Giuseppe De Pietro
5
and George Spanoudakis
2
1
Philips Research, Eindhoven, The Netherlands
2
SPHYNX Technology Solutions AG, Zug, CH, Switzerland
3
Biomedical Engineering Laboratory, School of Electrical and Computer Engineering,
National Technical University of Athens, Athens, Greece
4
Computer Science Department, Università degli Studi di Milano, Milan, Italy
5
Institute for High-Performance Computing and Networking, National Research Council of Italy,
ICAR - CNR, Naples, Italy
6
Department of Computer Science, City, University of London, London, U.K.
7
Atos Research and Innovation. Madrid, Spain
8
1st Otolaryngology University Department, National and Kapodistrian University of Athens, Athens, Greece
9
1st Cardiology Clinic, Medical School, National and Kapodistrian University of Athens, Athens Greece
giuseppe.depietro}@icar.cnr.it, {Qiqi.Su, Konstantin.Pozdniakov, C.Kloukinas}@city.ac.uk
Keywords: Cloud, AI, Semantic Interoperability, HL7 FHIR, Healthcare, GDPR, Evidence-based, Ageing, Hearing Loss,
Cardiovascular Disease, Balance Disorder.
Abstract: This paper describes a cloud-based platform that offers evidence-based, personalised interventions powered
by Artificial Intelligence to help support efficient remote monitoring and clinician-driven guidance to people
over 65 who suffer or are at risk of hearing loss, cardiovascular diseases, cognitive impairments, balance
disorders, and mental health issues. This platform has been developed within the SMART-BEAR integrated
project to power its large-scale clinical pilots and comprises a standards-based data harmonisation and
management layer, a security component, a Big Data Analytics system, a Clinical Decision Support tool, and
a dashboard component for efficient data collection across the pilot sites.
1 INTRODUCTION
Providing support for healthy living to an ageing
population is a central challenge for EU societies;
ageing has a significant social and financial impact
due to a higher incidence of health-related issues such
as hearing loss, cardiovascular diseases, cognitive
diseases, and balance disorders. The current focus in
elderly care is to develop solutions for the prevention
and effective treatment of age-related ailments.
In this paper, we present the cloud-based data
harmonisation and management platform
implemented in the SMART-BEAR project
1
that
aims to facilitate evidence-based personalised
1
SMART-BEAR: Smart Big Data Platform to Offer
Evidence-based Personalised Support for Healthy and
support for elderly patients in their home
environment.
The EU-funded SMART-BEAR project develops
a platform integrating a variety of sensors and mobile
instruments that actively collect data of enrolled
patients during their daily life, harmonise these data
and analyse them to provide effective
recommendations and personalised interventions.
The SMART-BEAR solution will be tested in large-
scale pilots involving approximately 5 000 senior EU
citizens in Portugal, Spain, France, Italy, Romania,
and Greece. Prior to the full-scale study, in September
2021, a first small-scale pilot, namely the "Pilot of the
Pilots" (PoP) has already started in Madeira, Portugal,
targeting to enrol 100 patients by June 2022.
Independent Living at Home. https://www.smart-
bear.eu/
Peretokin, V., Basdekis, I., Kouris, I., Maggesi, J., Sicuranza, M., Su, Q., Acebes, A., Bucur, A., Mukkala, V., Pozdniakov, K., Kloukinas, C., Koutsouris, D., Iliadou, E., Leontsinis, I., Gallo, L.,
De Pietro, G. and Spanoudakis, G.
Overview of the SMART-BEAR Technical Infrastructure.
DOI: 10.5220/0011082700003188
In Proceedings of the 8th International Conference on Information and Communication Technologies for Ageing Well and e-Health (ICT4AWE 2022), pages 117-125
ISBN: 978-989-758-566-1; ISSN: 2184-4984
Copyright
c
2022 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
117

The main components of the SMART-BEAR
cloud platform include databases and its underlying
information model, clinical repository interfaces, a
Big Data Engine, a data collection dashboard, and
analytics. The analytics and personalisation
components leverage the SMART-BEAR FHIR-
based Information Model. Separately from the cloud
platform, a smartphone application collects
information on the patient's basic physiological,
medical and behavioural parameters (such as steps
walked daily or weekly, weight in Kgs, or blood
pressure). This information is collected by means of
smart devices that are provided for one year (12
months) to each participant according to their
comorbidities and needs.
In recent years, there has been an increased
interest in e-health monitoring systems situated at
homes, leading to the creation of Health Smart
Homes. Such technologies can facilitate monitoring
patients' activities and enable efficient, decentralised
healthcare services at home. This type of monitoring
may improve the quality of care for the elderly
population and increase their well-being in a non-
obtrusive way. This approach allows for greater
independence and empowerment, maintaining good
health longer, preventing social isolation for
individuals, and delaying their placement in
institutions such as nursing homes and hospitals. The
recent advancements in the IoT technology, the
improvements with respect to user-friendliness, and
the significant cost reduction need to be considered as
well. This current wide use (compared to previous
periods) was enabled by major advances in wireless
technology and computing power, leading to a
plethora of diverse and specialised Medical IoT
(MIoT) that can generate and transmit data via open
protocols – and later, to be picked up and analysed.
It is not just the increase in the supply of
affordable MIoT monitoring medical and well-being
measurements that is changing the landscape in
personalised medicine and consumer health. The
data, generated at a rapid rate, along with the devices
themselves, are creating a connected infrastructure of
medical devices, software applications and health
systems and services, that is transforming healthcare
delivery. Nowadays, the evolution of e-health
systems equipped with Big Data Analytics (BDA)
capabilities permits the provision of good quality
decision support, enhancing care delivery. The
efficient information exchange and data reusability,
together with the utilisation of data mining and ML
analytics help to convert information into knowledge
(Dash, Shakyawar, Sharma, & Kaushik, 2019).
With all the progress achieved in this domain,
challenges remain in how to use the information and
the derived knowledge productively and in a way that
can be evaluated systematically, as the scientific
community does not have a commonly accepted way
of capturing it, while industry traditionally invests in
technological solutions that can be commercially
exploited. The HL7 (Health Level Seven) FHIR (Fast
Healthcare Interoperability Resources) standard, a
well-known specification that can be used for the
representation of clinical data, provides the
underlying basis for our data harmonisation solution.
Accompanied by well-defined semantics captured
using widely adopted ontologies such as LOINC and
SNOMED-CT for the semantic representation of
data, the standardised data representation helps
streamline the development of analytics and decision
models with the potential to provide accurate,
personalised interventions via decision support tools.
These tools digest the harmonised information and
facilitate decisions that are vetted by health
professionals to ensure patient safety.
Along with the production of knowledge, the
dimension of data protection needs to be adequately
addressed. Processing of sensitive personal data must
be compliant with all relevant legal requirements and
privacy obligations laid down by national legislation
in addition to those imposed by the General Data
Protection Regulation (GDPR), a legal framework
that fundamentally transformed how personal data
must be managed lawfully. In this context, it is not
enough just to have in place organisational
procedures along with IT-supported processes for
exercising certain GDPR rights. Vulnerabilities do
happen, even within the best organised and best coded
IT systems. Therefore, mechanisms to ensure the
security and privacy of the data held, the integrity of
any platform storing and managing them (integrity,
confidentiality, and availability of data at rest, in
transit and processing for data flows), in a continuous
security and privacy assurance approach, are of
paramount importance. On this axis, and given the
legal obligations imposed by the GDPR and the state-
of-the-art guidelines (e.g., encryption guidelines of
NIST), data minimisation, pseudo/anonymisation,
transparency in processing personal data, and audits
support are among the appropriate technical (and
organisational) measures that must be taken into
account, preferably at early stages, to ensure that all
legal requirements are met.
Last but not least, Big Data Analytics (BDA)
systems for healthcare decision-making must not only
focus on the production of ML knowledge but also
convey it in an easy-to-use way, accompanied by
ICT4AWE 2022 - 8th International Conference on Information and Communication Technologies for Ageing Well and e-Health
118
information that aims to make AI algorithms more
understandable by people (AI explainability).
Diachronically, e-health systems do not appear to be
rated satisfactorily in terms of their usability
(Population ageing in Europe Facts, implications and
policies) (Basdekis, Sakkalis, & Stephanidis, 2011),
while understanding AI remains an open question
(Liao, Gruen, & Miller, 2020). These systems, in
particular, are being used within a high-stress
environment, by non-technical end-users, and
perhaps with time constraints that made the situation
even worse. Thus, the acceptance and usability by the
involved end-users of such functionality is a critical
factor for its success and a key requirement in the
SMART-BEAR project.
2 THE SMART-BEAR
ARCHITECTURE
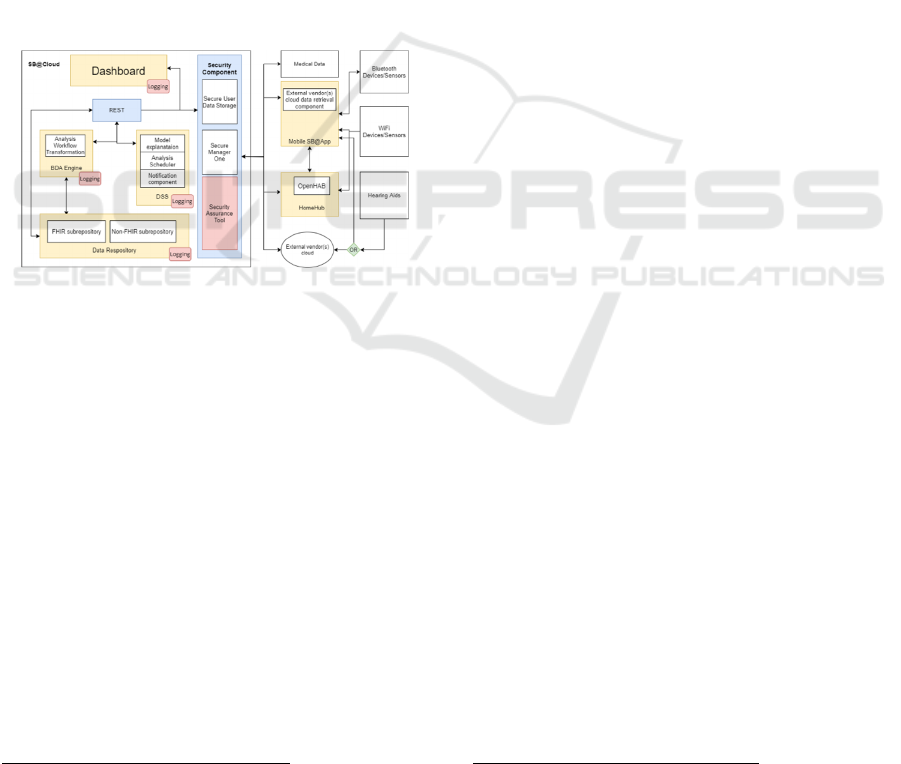
Figure 1: Overall SMART-BEAR architecture.
The architecture consists of three main systems: a
mobile phone application (Mobile SB@App), the
SB@HomeHub and the SB@Cloud. The overall
architecture is depicted in Figure 1. The mobile
application allows collecting the data from all
portable devices connected to a person's mobile
phone (such as heart rate and steps measurements).
The HomeHub accumulates data from different
sensors of home-based devices (such as movement
sensors) directly, as well as from external vendor
clouds.
Finally, SB@Cloud is the core system responsible
for the secure storage and analysis of the data
collected. The main components of the cloud
platform include FHIR-compliant/non FHIR-
compliant data repository, its underlying information
model, the clinical repository interfaces, the Big Data
Engine including the synthetic data generation
2
Smart4Health: Citizen-centred EU-HER exchange for
personalised health. https://smart4health.eu/
component, the analytics, Decision Support System
(DSS) and the Dashboard – a user interface
component. The analytics and personalisation
components leverage the FHIR-based Information
Model. DSS provides the functionality for
interventions, reasoning behind the decisions
proposed, analysis scheduling and notifications. The
clinical repository interfaces allow the accumulation
of the data from Electronic Health Records (EHR)
external to the project’s infrastructure. On the
backend level, all components are interconnected via
RESTful interfaces. User interaction with the project
infrastructure is provided via the dashboard. The
communications between components, as well as
authentication at the dashboard, are secured
according to GDPR via the security component,
which assures all security mechanisms are working
correctly. The security component also enables
interoperability with external platforms that use the
FHIR standard to represent medical/usage data. A
secure, privacy-preserving machine-to-machine
bridge with two platforms, developed within the
Smart4Health
2
and Holobalance
3
EU-funded
projects, is currently being tested in the PoP (Pilot of
Pilots).
3 THE SMART-BEAR CLOUD
COMPONENTS
3.1 The Database Implementation
The clinical repository component of SB@Cloud is
utilising a combination of FHIR-compliant and non-
FHIR databases. All the data that represent medical
entities are stored in the FHIR database while data
related to non-medical entities are stored in the non-
FHIR database of the Cloud Backend. Those contain
elements that are not mapped to FHIR models (such
as dashboard user settings) and intermediate results of
the analytics models which some of them relay data
back to the FHIR database. The non-FHIR database
is also used to store data transmitted by the HomeHub
which is placed in the patient's home and monitors the
usage of light sources, temperature and humidity and
motion inside the home. The interventions, the
notifications and the alerts that are generated by the
DSS are stored in the non-FHIR database.
3
Holobalance: Holograms for personalised virtual
coaching and motivation in an ageing population with
balance disorders. https://holobalance.eu/
Overview of the SMART-BEAR Technical Infrastructure
119

3.2 Data Model Specification
Compliant with FHIR
HL7 FHIR is the latest standard from HL7, an
international standards development organisation that
has been publishing healthcare interoperability
standards since 1989. FHIR takes the best of, and
builds upon the lessons learnt from the different
directions taken previously by HL V2 and HL7 V3
and while applying well-known, modern technologies
such as REST and JSON. The standard focuses on
implementers first, provides out-of-the-box tooling,
is published for free and is free to use.
The standard is spreading rapidly in the
international context and the most important
international organisations that provide solutions to
specific problems in healthcare, like Integrating the
Healthcare Enterprise (IHE) (Integrating the
Healthcare Enterprise, n.d.), that is an initiative by
healthcare professionals and industry to improve the
way computer systems share health information and
Personal Connected Health Alliance
(PCHA) (Personal Connected Health Alliance, n.d.),
that is a membership-based Healthcare Information
and Management Systems Society (HIMSS)
Innovation Company that works for advancing
patient/consumer-centred health, wellness and
disease prevention by means of the Continua Design
Guidelines. The IHE and PCHA are updating their
technical specifications to include FHIR.
FHIR was chosen as the standard for clinical data
within SMART-BEAR for its speed and ease of
implementation, and the fact that modern web
technologies such as REST and JSON are an
especially good fit for mobile applications, which the
project makes use of. FHIR is used nationally in The
Netherlands as part of the MedMij project (MedMij,
2022) and Estonia makes use of it in their national
electronic health record system, among other
countries. Countries such as the Netherlands,
Switzerland, Belgium have defined national core
profiles for FHIR that standardise clinical
information relevant for the countries within. In this
context, using a standard that is gaining adoption in
Europe enables us to be open-minded about the
possibilities of future data exchange.
The nature of the data treated in the project, in
accordance with the rules of the FHIR standard, led
to the necessity of using a specific Implementation
Guide (IG). For this reason, an analysis of the IGs
published on the FHIR registries was carried out.
Among these, particular attention was paid the
Personal Health Device (PHD) (HL7, Personal
Health Device Implementation Guide, n.d.) and
International Patient Summary (IPS) (HL7,
International Patient Summary Implementation
Guide, s.d.) IGs.
The PHD IG adapts FHIR resources to convey
measurements and supporting data from PHDs to
different kind of systems, like platforms for electronic
medical records, clinical decision support, etc. The
interest for this IG was captured considering that it is
based on the Continua Design Guidelines and upon
the ISO/IEEE 11073 PHD Domain Information
Model (DIM) (Huang, Wang, & Wang, 2020).
Regardless, considering that in SMART-BEAR many
health data are not acquired by PHDs, but by
collecting patients’ answers to specific
questionnaires, this IG was not considered adequate
for the SMART-BEAR project.
The IPS IG defines the rules to produce a
document containing the essential healthcare
information about a subject of care, designed for
supporting unplanned, cross-border care, although it
is not limited to it. Although this IG provides an
important contribution to identify a minimal,
specialty-agnostic, condition-independent, clinically
relevant dataset for a patient, it was not considered
relevant for the SMART-BEAR project.
For these reasons, in compliance with the FHIR
standard and in line with the choices adopted in many
European projects, the approach taken for the
definition of the information model for the project is
to define a dedicated SMART-BEAR IG by profiling
a set of identified FHIR resources and individuating
the terminologies from international standard code
systems as well as internal value sets. The tool chosen
for modelling the FHIR information model is
SUSHI (FSH School, n.d.), considering that it
integrates well with the IG publisher which is an
official tool provided by HL7.
Currently, the published IG (implementation
guide) consists of 84 profiles (of type Observation,
Condition, Questionnaires, Bundle, Patient,
DeviceUseStatement, FamilyMemberHistory,
MedicationStatement, ResearchSubject), 2
extensions, 33 value Sets, and 133 examples.
3.3 The Clinical Data Repository
The SMART-BEAR (SB) Clinical Data Repository
(CDR) is based on the Health Data Hub which is built
around the HL7 FHIR standard, structuring and
disposing of clinical information using this standard
as specification. Therefore, the SB CDR repository
stores and serves clinical information in HL7
standardised, safe and scalable way. This allows Big
Data Analytics (BDA) and Decision Support System
(DSS) developers to focus on having the algorithms
ICT4AWE 2022 - 8th International Conference on Information and Communication Technologies for Ageing Well and e-Health
120
or applications that best suit the SMART-BEAR
pilots requirements, enabling them to build a common
set of solutions and products smoothly connected
using standardised data. Medical terminology not
fully covered by FHIR will be annotated using
SNOMED-CT
4
. The interoperability with some
different clinical terminologies (ICD9, LOINC) used
across the healthcare industry will be reached by
adapting the Atos Terminology Server (ATS). ATS
will be customised and implemented in the second
phase, after the finalisation of the PoP, and it will
provide a RESTful API. This API will allow for safe
access to clinical information via interaction with the
FHIR database for terminology purposes.
3.4 The Security Component
Data protection is considered a critical issue,
especially when dealing with special categories of
personal data (Art 9, GDPR). In this context, the
SB@Cloud, by virtue of its design, supports privacy.
In particular, the Security Component (SB@SC)
provides mechanisms that handle data minimisation,
authentication and other security and privacy aspects
by performing pseudonymisation and resource
identifier re-associations (Basdekis, Pozdniakov,
Prasinos, & Koloutsou, 2019). This component
supports RBAC (Role-based access control)
authentication and authorisation of all RESTful API
endpoints (Token-based access via encrypted HTTPS
connections) to protect the transmission of any
(sensitive or not) data, and it also introduces services
to cope with the management of privacy-related
requests to demonstrate compliance with the GDPR.
The way the data is stored in 2 different repositories
(i.e., personal data and PII stored encrypted in a
separate one, while all pseudonymised medical and
usage data in the CDR), allows the analysis of the
fully anonymised data to continue after the end of the
project, provided that all personal data will be
deleted. Thus, after the completion of the SB project,
data kept in SB@SC will no longer be needed to
conduct the research (e.g., analytics, interventions),
and consequently will be erased and not further used
for any data process.
In parallel, SB@SC component is also
responsible for monitoring, testing, and assessing the
security and privacy of all operations of the platform.
It will also audit critical components and processes of
the infrastructure while leveraging monitoring
mechanisms developed in the context of the project to
provide an evidence-based, certifiable view of the
security posture of the whole platform, along with
4
https://www.snomed.org
accountability provisions for changes that occur in
said posture and the analysis of their cascading
effects. Several built-in security assessments
addressing the Confidentiality – Integrity –
Availability (CIA) principles among which are
custom metrics with respect to the platform's
components will be utilised, leveraging an evidence-
based approach to provide security and privacy
assurance assessments with certifiable results.
3.5 The SMART-BEAR Information
Model
As described above, data in SMART-BEAR is
partitioned across two databases – clinical data in the
FHIR database, and non-clinical or private
information that is not exposed to analytics in a non-
FHIR one.
FHIR is a platform specification (see section 3.2);
it is intended to be constrained for a specific use case
and so we profile various resources in the FHIR
database for our needs. We naturally use the Patient
resource to store basic demographic information such
as name, date of birth, and ethnicity, while the bulk of
the clinical data resides in Conditions and
Observations that are tied to the Encounter resource.
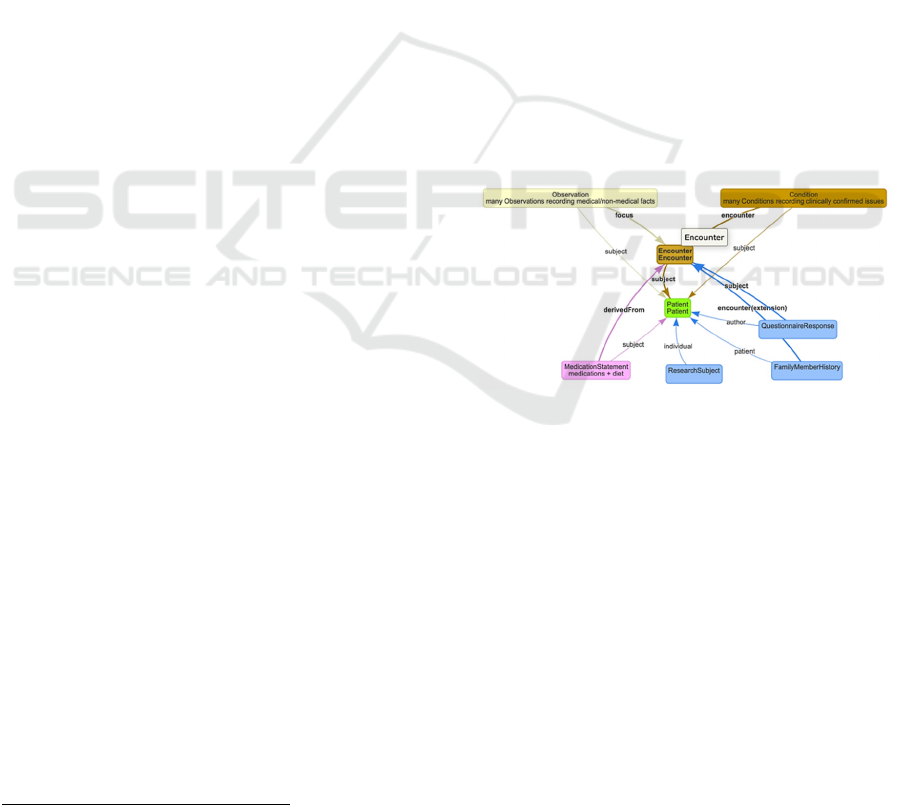
Figure 2: Information model of FHIR resources in use.
Given that we have clinicians performing patient
assessments, a single assessment is represented by an
instance of an Encounter resource. This Encounter
resource is key to the information model as all other
resources either link to or from it, creating a graph by
which you can reach all the relevant nodes
(resources). Any concerning clinical issues noted
during an assessment are stored in a Condition
resource. Issues or observations of lesser importance
are stored as FHIR Observations, which also house
'negations' – issues that a clinician has verified that
the patient does not have. This fine but important
difference between a lack of data (unknown value)
and a refuting observation (known negative) allows
us to build more accurate analytics algorithms.
Overview of the SMART-BEAR Technical Infrastructure
121
Most Observations follow a simple 'key-value'
pattern, where Observation.code identifies the type of
measurement and Observation.value[x] records the
measurement value. In case of Conditions,
Condition.code records the type of condition. As an
example, in case of the patient having anxiety
Condition.code will be populated with 197480006
|Anxiety disorder| from SNOMED – and should they
not be affected by anxiety, Observation.code will
have the same terminology code but
Observation.valueCodeableConcept will be
populated with 260385009 |Negative|.
Where possible, we align with FHIR Vital Signs
standard profiles – for example blood pressure, where
we record systolic/diastolic measurements using
Observation.component, we record the arm
(left/right) as bodySite and the patient's position
(standing/supine) is part of the LOINC code. Our
Implementation Guide (IG) contains a wealth of
Condition, and positive/negative Observation
examples to assist users in understanding of the FHIR
DB.
Specialised resources are used where appropriate;
FamilyMemberHistory for example is used to record
the family history of hearing loss and
ResearchSubject is used to record the source of
referral to our clinical study. MedicationStatement
records both the list of medications the patient is
taking using the WHO ATC value set, and the diet
they are prescribed.
A significant part of the data acquired by clinical
assessments comes in a form of over 20
Questionnaires; these are internationally recognised,
standard data collection points whose outcome scores
will be used for analytical purposes.
Previously mentioned Conditions and
Observations rely on over 120+ terminology
mappings, with most codes coming from SNOMED,
to link the semantic meaning within. Codes from
LOINC and MESH complement the rest of the
mappings. Special care was taken not to create
custom codes unless absolutely necessary to avoid the
creation of new medical knowledge - just 4 new codes
have been introduced that did not have equivalents in
any of the searched code systems. Several food/diet-
related concepts not available in the SNOMED
international core but available in the Australian
edition were also made use of for this reason. We
verified that this does not impose any additional
licensing constraints SNOMED-wise.
Following the theme of avoiding introducing new
codes as much as possible, two SNOMED post-
coordinated expressions were crafted to accurately
represent very specific concepts: "number of non-
scheduled visits due to volume overload in subjects
with heart failure" as:
4525004 |emergency department patient visit|
:362981000 |qualifier value| = 260299005
|number|, 42752001 |due to| = 21639008
|hypervolemia|
and “number of Visits to the ER due to HTN
peak” as:
4525004 |emergency department patient visit|
:362981000 |qualifier value| = 260299005
|number|, 42752001 |due to| = 38341003
|hypertension|
When it came to recording the patient's ethnicity,
and this is an interesting subject because data
recorded here really depends on where you happen to
be in the world, we chose to re-use the FHIR
extension and value set as published by the German
Corona Consensus Data Set (GECCO) project, which
itself is partially based on WHO ISARIC eCRF
valueset. Re-use of existing knowledge like these
bolsters long-term interoperability.
Analytics are a crucial aspect of the system,
giving it the necessary intelligence for the task at
hand. They are driven by the BDA Engine, which has
several requirements placed upon it – raw data
processing, incremental updates, and scalability.
As mentioned before, clinical data in the system
is stored in a FHIR repository. While a FHIR
interface has the advantages that make it an excellent
choice for clinical data, where it makes compromises
is the area of bulk data processing. For this reason, the
BDA engine requires a capability to convert and
flatten the hierarchical format of FHIR to a relational
one that lends itself better to bulk data processing. It
should be possible to do this conversion
incrementally as new data is arriving in the clinical
repository in order to run analytics continuously, and
it also needs to be able to scale with large volumes of
data.
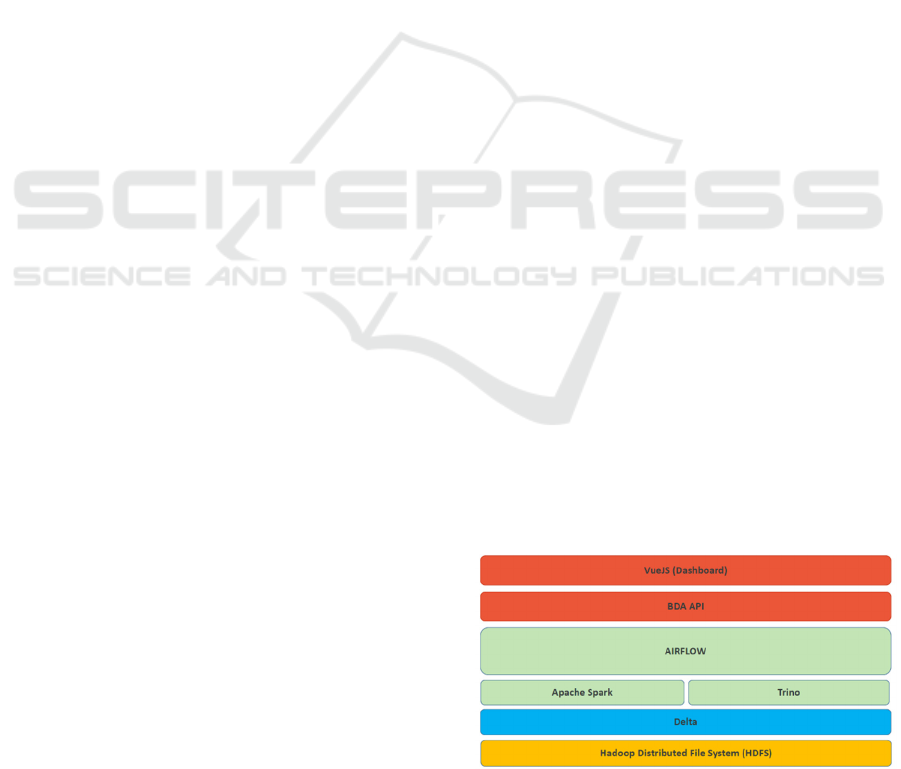
3.6 The BDA Engine
Figure 3: The BDA Engine architecture.
ICT4AWE 2022 - 8th International Conference on Information and Communication Technologies for Ageing Well and e-Health
122

The BDA Engine mainly addresses the functionalities
required for processing Data Analysis Workflows
(DAWs) and providing/storing the execution results.
The BDA Engine exposes a set of APIs to compute
and to get raw data to perform analyses. In terms of
Machine Learning, a preliminary extraction of data
analytics - that will be carried on the pre-processed
datasets - are going to indicate variables or
combinations of variables for the feature selection
approaches. All ML methods and techniques are data-
driven, and the "best" method will be decided after its
application.
The preliminary extraction of data analytics is
performed by the following subcomponents featured
in the BDA Engine architecture: Delta Lake
5
, Spark
6
,
Trino
7
, Airflow
8
. The components are described here
below by following a bottom-up approach, the layer
at the bottom being the closest to the data repositories.
The architecture is shown in Figure 2 and it is an
extended version of the one presented in (Anisetti, et
al., 2021).
Delta Lake is an ACID table storage layer over
cloud object stores and is the closest component to the
repositories. Delta Lake enables to build a Lakehouse
Architecture on top of existing storage systems such
as Amazon S3, Azure Data Lake Storage (ADLS),
Google Cloud Storage (GCS), and Hadoop
Distributed File System (HDFS)
9
(Armbrust, et al.,
2020). In the case of SMART BEAR, the adopted
standard is HDFS.
Spark and Trino are the components collocated on
the third layer from the bottom and provide the
capability to access data and perform queries on the
datasets. Spark is a multi-language engine for
executing data engineering, data science, and
machine learning on single-node machines or
clusters. Spark was chosen because it is capable of
processing tasks encompassing custom analytics on
large data volumes, and in addition, it features many
bindings with other commonly used Data Science and
Machine Learning libraries. Spark is also capable to
work both on batch and streaming data. Trino is the
component providing the capability to access and
perform highly parallel and distributed queries on
data from multiple systems. Trino was chosen
because it provides the BDA Engine with the
capability of managing On-Line Analytical
Processing (OLAP) queries and data warehousing
tasks, and because it can operate on many data
sources in addition to data that are stored on HDFS.
5
https://delta.io/
6
https://spark.apache.org/
7
https://trino.io/
Airflow is the component providing the capability
to programmatically author, schedule, and monitor
workflows that are written in Python programming
language. Airflow is the fourth layer from the bottom.
3.7 Decision Support System
The DSS is designed to assist the clinicians in the
initial assessment of every patient in terms of the
optimal assessments that must be performed to assess
the patient and then provide them with the optimal
combination of the devices to monitor their health
during the pilot study. This component is designed to
evolve throughout the project, as it will continuously
be trained by the data that will be digested into the
platform. The initial version of DSS available for the
PoP has adopted the rules and the medical guidelines
that have been provided by the clinicians to have a
ground truth system based on the most updated
medical knowledge. For each of the monitoring
conditions of the SMART-BEAR project (Hearing
Loss, Cardiovascular Diseases, Mild Cognitive
Impairment, Mild Depression, Balance Disorders,
and Frailty) the medical teams are providing the
rules-based scenarios and the relevant interventions
that should be provided to the participants. The rules-
based algorithms are taking into consideration the
personalised thresholds that are set for each patient
individually. For example, for CVDs, optimal and
extreme cut-off values are set for the blood pressure,
which trigger the generation of notifications and alert
to the patient and the clinical care team.
Starting with the PoP, the data that will be
collected feed the models of the BDA engine and
output of the analytics will be combined with the
measured parameters to identify the degree of
satisfaction of the patients and to what degree are the
personalised thresholds requiring modifications. If
the results of the analytics provide insights that lead
to a new intervention, the DSS is capable to be
extended to support all the new interventions that will
be provided by the clinicians. It must be noted that
any new intervention must first be validated by the
clinicians before it is included in the interventions
provided to the patient.
8
https://airflow.apache.org/
9
https://hadoop.apache.org/docs/r1.2.1/hdfs_design.html
Overview of the SMART-BEAR Technical Infrastructure
123
3.8 Dashboard
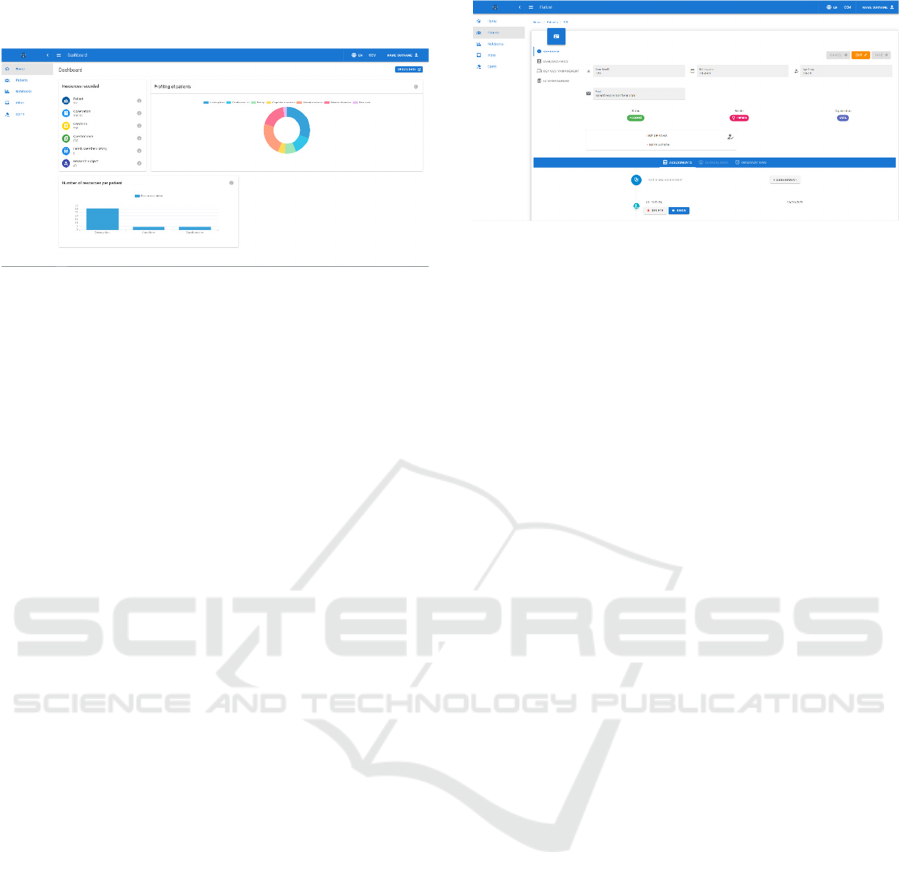
Figure 4: Dashboard homepage.
The SMART-BEAR Dashboard is a component
aimed at providing clinicians with a user-friendly
graphical user interface. The Dashboard home page is
shown in Figure 3. The Dashboard can be used by the
clinicians to create and manage a patient, considering
his/her devices and medications, conduct the first
visit and the check-ups, perform analytics on data and
create interventions to be delivered. All the data
collected are stored in the FHIR and non-FHIR
repositories depending on their clinical value: the first
collection is made during the Baseline Assessment
from a patient and it concerns the medical history, the
physical examinations, and the questionnaire
responses, and on the basis of the information
provided the dashboard visualises suggestions about
the eligibility of the prospective participants of
SMART-BEAR pilot studies. A profiling
functionality is also featured that suggests the
clinician the specific tabs and questionnaires to be
activated based on the conditions detected. Although
a patient’s profile is eventually chosen by a clinician,
the profiling functionality redirects the users to the
clinical tools and the devices that are required to
match a patient’s profile consistently with the
SMART-BEAR protocol. After a patient is created
and deemed eligible, the Dashboard shows specific
tabs that enable the patient management and contain
information concerning the demographic data,
including the living situation and ethnic group, the
participation in synergies, and the type and status of
provided devices. The patient management tab is
shown in Figure 4. Another functionality is featured
that is the visualisation of the notifications delivered.
The analytics and intervention mechanisms are in
the development phase, and they will make it possible
for the clinicians to perform analytics on collected
data targeting all patients or only a specific subgroup
defined by parameters to monitor in a determined
condition in the future. Based on the outcome of the
analytics and with support from the DSS, the
Figure 5: Patient management page.
Dashboard visualises suggestions for clinicians on the
interventions to launch, although the final choice is
made by a clinician, who will also be able to monitor
the intervention outcome. Examples of analytics to be
made available in the Dashboard are discussed
in (Bellandi, et al., 2021).
4 FURTHER WORK
SB@Cloud will operate for at least three years during
which the whole solution will be tested and validated
through five large-scale pilots involving 5.100 elderly
living at home in Greece, Italy, France, Spain,
Portugal, and Romania to demonstrate its efficacy,
extensibility, sustainability, and cost-effectiveness.
During this period, the analysis of the collected data,
driven by high level big data analytics and decision
models, expected to generate evidence (i.e., metrics,
observational evidence base) useful for offering
personalised health care and medicine in clinical
practice. Still, analysis upon anonymous data can be
continued even after the project’s lifecycle as the
pseudonymisation mechanism in place allows this
type of management. To support this notion,
SMART-BEAR aims to develop a data sharing and
valorisation model (DSVM). This model will identify
ways, at a technical and organisational level, for
extending the data collected in SMART-BEAR by
integrating new data providers and open sources and
use the outcomes of data analysis to improve the
platform performance, enhance further the
personalisation of its relation with its end users,
develop new services, and monetise data intensive
services out of the platform.
5 CONCLUSIONS
In this paper we have presented an overview of the
cloud-enabled standards-based integrated system
ICT4AWE 2022 - 8th International Conference on Information and Communication Technologies for Ageing Well and e-Health
124

developed in the SMART-BEAR project, which is
able to record assessments for, monitor, and deliver
clinician-vetted interventions to senior citizens to
assist in monitoring, to empower the patients and to
support healthy living at home. The system is
supported by an underlying semantic interoperability
solution based on widely-adopted standards, such as
HL7 FHIR, and advanced analytics. The platform will
be leveraged during the SMART-BEAR Pilot of
Pilots and further refined to support the planned
large-scale pilots in all the participating countries.
ACKNOWLEDGEMENTS
This work was supported by the European
Commission’s Horizon 2020 research and innovation
program under the SMART-BEAR project, grant
agreement No 857172.
REFERENCES
Anisetti, M., Ardagna, C., Braghin, C., Damiani, E.,
Polimeno, A., & Balestrucci, A. (2021). Dynamic and
Scalable Enforcement of Access Control Policies for
Big Data. Proceedings of the 13th International
Conference on Management of Digital EcoSystems.
Armbrust, M., Das, T., Sun, L., Yavuz, B., Zhu, S., Murthy,
M., . . . Zaharia, M. (2020). Delta lake: high-
performance ACID table storage over cloud object
stores. Proceedings of the VLDB Endowment, 13(12),
3411-3424.
Basdekis, I., Pozdniakov, K., Prasinos, M., & Koloutsou,
K. (2019). Evidence Based Public Health Policy
Making: Tool Support. 2019 IEEE World Congress on
Services (SERVICES), (pp. 272-277). Milan, Italy.
Basdekis, I., Sakkalis, V., & Stephanidis, C. (2011).
Towards an accessible personal health record.
International Conference on Wireless Mobile
Communication and Healthcare (pp. 61-68). Springer,
Berlin, Heidelberg.
Bellandi, V., Basdekis, I., Ceravolo, P., Cesari, M.,
Damiani, E., Iliadou, E., . . . Maghool, S. (2021).
Engineering Continuous Monitoring of Intrinsic
Capacity for Elderly People. 2021 IEEE International
Conference on Digital Health (ICDH) (pp. 166-171).
IEEE.
Broekhuis, M., van Velsen, L., Peute, L., & Halim, M.
(2021). Conceptualizing Usability for the eHealth
Context: Content Analysis of Usability Problems of
eHealth Applications. JMIR Formative Research, 5(7),
e18198.
Dash, S., Shakyawar, S., Sharma, M., & Kaushik, S. (2019).
Big data in healthcare: management, analysis and future
prospects. Journal of Big Data, 6(1), 1-25.
European Commission. (2015). The 2015 Ageing Report
Economic and budgetary projections for the 28 EU
Member States (2013-2060), Technical Report.
Brussels.
FSH School. (n.d.). SUSHI. Retrieved March 2022, from
https://fshschool.org
HL7. (n.d.). International Patient Summary
Implementation Guide. Retrieved March 2022, from
https://hl7.org/fhir/uv/ips
HL7. (n.d.). Personal Health Device Implementation
Guide. Retrieved March 2022, from
http://hl7.org/fhir/uv/phd/2019May
Huang, Z., Wang, Y., & Wang, L. (2020). ISO/IEEE 11073
Treadmill Interoperability Framework and its Test
Method: Design and Implementation. JMIR medical
informatics, 8(12), e22000.
Integrating the Healthcare Enterprise. (n.d.). Retrieved
March 2022, from Integrating the Healthcare
Enterprise: https://www.ihe.net/
Liao, Q., Gruen, D., & Miller, S. (2020). Questioning the
AI: informing design practices for explainable AI user
experiences. Proceedings of the 2020 CHI Conference
on Human Factors in Computing Systems, (pp. 1-15).
MedMij. (2022, March). Retrieved from The MedMij
Project: https://medmij.nl
Personal Connected Health Alliance. (n.d.). Retrieved
March 2022, from Personal Connected Health Alliance:
https://www.pchalliance.org
Population ageing in Europe Facts, implications and
policies. (n.d.). Retrieved from
https://ec.europa.eu/research/social-
sciences/pdf/policy_reviews/kina26426enc.pdf
Population structure and ageing. Electronic. (2017).
Retrieved from http://ec.europa.eu/eurostat/
statisticsexplained/index.php/Population_structure_an
d_ageing
World Health Organisation. (2015). World report on
Ageing and Health. Retrieved from http://apps.who.int
/iris/bitstream/handle/10665/186463/9789240694811_
eng.pdf.
Overview of the SMART-BEAR Technical Infrastructure
125
