Cardiovascular Disease Risk Prediction with Supervised Machine
Learning Techniques
Elias Dritsas, Sotiris Alexiou and Konstantinos Moustakas
Department of Electrical and Computer Engineering, University of Patras, 26504 Rion, Greece
Keywords:
CVDs, Machine Learning, Risk Prediction.
Abstract:
Cardiovascular diseases (CVDs) are the leading cause of death worldwide and a major public health concern,
with heart diseases being the most prevalent ones, thus the early prediction is being considered as one of the
most effective measures for CVDs control. The risk evaluation for CVD occurrence on participants (men
and women) especially aged older than 50 years with the aid of Machine Learning (ML) models is the main
purpose of this research paper. The performance of supervised ML models is compared in terms of accuracy,
sensitivity (or recall) in identifying those participants that actually suffer from a CVD and Area Under Curve
(AUC) score. The experimental analysis demonstrated that the Logistic Regression classifier is the most
appropriate against Naive Bayes, Support Vector Machine (SVM) and Random Forest with 72.1% accuracy,
recall and 78.4% AUC.
1 INTRODUCTION
The term ”cardiovascular disease” contains a wide
range of disorders, including all pathological changes
involving the heart and/or blood vessels. These dis-
eases include hypertension, coronary heart disease,
heart failure, angina, myocardial infarction and stroke
(Kumar and Ramana, 2021). Cardiovascular diseases
have been the leading cause of death in developing
countries for the past 15 years, and by 2030 deaths
will exceed 20 million per year. A taxonomy of CVDs
is presented in Table 1.
Heart diseases and stroke constitute one of the
biggest causes of morbidity and mortality among
the population worldwide (Roth et al., 2017), with
the most important behavioral risk factors being un-
healthy diet, sedentary lifestyle, smoking and exces-
sive use of alcohol. The effects of behavioral risk
factors may show up as raised blood pressure, raised
blood glucose, raised blood lipids, and overweight
and obesity. In detail, the main risk factors for the oc-
currence of cardiovascular diseases include (Wilkins
et al., 2017), (Abdalrada et al., 2022):
• Obesity/High BMI: obesity alone is a high-risk
factor for CVDs
• Physical activity: sedentary lifestyle increases the
risk of CVDs
• Alcohol consumption: excessive alcohol use can
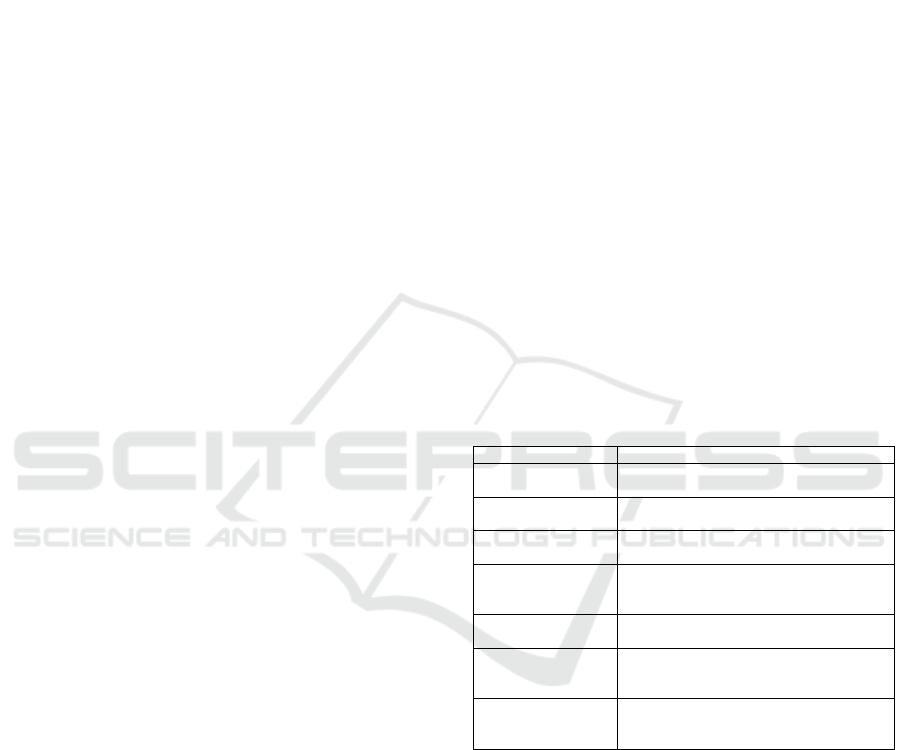
Table 1: Taxonomy of CVDs.
Heart Disease Description
Coronary disease of the blood vessels supplying the
heart muscle
Cerebrovascular disease of the blood vessels supplying the
brain
Peripheral arterial disease of blood vessels supplying the arms
and legs
Rheumatic damage to the heart muscle and heart valves
from rheumatic fever
caused by streptococcal bacteria
Congenital malformations of heart structure existing at
birth
Deep vein thrombosis blood clots in the leg veins, which can dis-
lodge and move to the heart and lungs
Pulmonary embolism
Heart attacks, strokes acute events mainly caused by a blockage
that prevents blood from flowing to the heart
or brain
raise blood pressure levels and increase levels of
triglycerides, thus increasing the risk for cardio-
vascular diseases
• Smoking and secondhand smoke: nicotine raises
blood pressure
• Hyperlipidemia: also known as High cholesterol
or hypercholesterolemia
• Dyslipidemia: abnormal level of fat or cholesterol
in human’s blood vessels
• Family history, Psychosocial stress, the coexis-
tence of other chronic conditions: Type 2 dia-
betes, Arterial hypertension
The ”2013 ACC/AHA Guideline on the Assessment
Dritsas, E., Alexiou, S. and Moustakas, K.
Cardiovascular Disease Risk Prediction with Supervised Machine Learning Techniques.
DOI: 10.5220/0011088300003188
In Proceedings of the 8th International Conference on Information and Communication Technologies for Ageing Well and e-Health (ICT4AWE 2022), pages 315-321
ISBN: 978-989-758-566-1; ISSN: 2184-4984
Copyright
c
2022 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
315

of Cardiovascular Risk” (Yancy et al., 2013) provides
detailed recommendations for estimating cardiovas-
cular disease risk in the clinical practice, considering
several factors including age, gender, race, cholesterol
and blood pressure levels, diabetes and smoking sta-
tus, and the use of blood pressure-lowering medica-
tions. In Europe, the 10-year risk factor of fatal CVD
is estimated based on different charts established by
the European Society of Cardiology for high-risk and
low-risk populations across Europe, which may be
further adapted to national or regional specific charts
based on published mortality data.
In the literature, the CVDs risk prediction is ad-
dressed with either appropriate risk tools or the aid of
machine learning. In (Gale et al., 2014), the Fram-
ingham cardiovascular disease risk score and inci-
dent frailty studied on English cohort data for age-
ing participants. Moreover, the systematic coronary
risk evaluation (SCORE) has been suggested to pre-
dict the 10-year risk of cardiovascular death in Eu-
rope or the QRISK to predict the composite outcome
of coronary heart disease and ischaemic stroke. Oth-
ers employ machine learning techniques, also aiming
at predicting potential risk of CVDs (Mohan et al.,
2019), (Yang et al., 2020).
ML is a branch of artificial intelligence (AI) and a
powerful tool in the medical field, as it can help pre-
dict various diseases. In (Dinesh et al., 2018), var-
ious data-driven approaches are presented to predict
diabetes and cardiovascular disease with ML models.
Here, we will solely focus on its application to cardio-
vascular medicine (Haq et al., 2018). Our purpose is
to identify predictive data patterns and high-risk CVD
groups among the elderly. Moreover, we aim to create
personalized risk models that will be part of the pre-
dictive AI tools integrated into the SmartWork (Koc-
sis et al., 2019) and GATEKEEPER systems. The
presented method for the risk prediction of CVDs oc-
currence was developed and validated independently
with a publicly available dataset and, in parallel, as
part of the projects with pilot data. The incorporation
of the ML models into the Long-term Risk Prediction
tools of the SmartWork system aims to design a smart
age-friendly healthy living and working environment
for office workers. The GATEKEEPER system pur-
sues to sustain, as healthy as possible, the life of older
people living at home, preventing the occurrence of
CVD, type 2 diabetes mellitus (T2DM)(Fazakis et al.,
2021), high cholesterol, hypertension (Dritsas et al.,
2021), chronic obstructive pulmonary disease-COPD
(Hussain et al., 2021) (chronic conditions related to
Metabolic Syndrome-MetS).
Given that MetS combines risk factors that pro-
mote the development of cardiovascular disease
(CVD) and type 2 diabetes (T2DM)(Hoyas and Leon-
Sanz, 2019), as a first approach, our paper aims to
present a methodology for correctly identifying those
at risk of diagnosed with a CVD in long-term. For
this purpose, the classification performance of various
ML models is estimated on each test instance from a
CVD dataset. The ML models that achieve the high-
est recall (namely, high sensitivity) and Area Under
Curve (AUC) show that the CVD class can be pre-
dicted correctly. The main contribution of this work
is a comparative evaluation of different ML models
on a balanced dataset and the proposal of a Logistic
Regression model for the long-term CVD risk predic-
tion. In the upcoming sections, the main steps of the
employed process are demonstrated.
The rest of this paper is organized as follows. Sec-
tion 2 presents the main parts of the methods for the
long-term risk prediction of CVD. Section 3 makes
an analysis of the dataset features and Section 4 de-
scribes the pre-processing steps for the design of the
training and testing dataset and feature ranking. Sec-
tion 5 presents the experimental set up and the clas-
sification performance of ML techniques. Ultimately,
Section 6 concludes the paper and notes future direc-
tions of the current outcomes.
2 MACHINE LEARNING
METHODS
Data science and especially machine learning has
been widely used in the field of medicine for the risk
analysis of several chronic conditions. The most com-
mon application of these models aims to determine
the most suitable factors for the long-term risk pre-
diction to avoid serious health complications (due to
certain symptoms) and support health care manage-
ment.
In this study, the forecasting performance of four
different machine learning models is presented. In
particular, the Naive Bayes, SVM, Logistic Regres-
sion and Random Forest are utilized to estimate the
long-term risk of an older person being diagnosed
with cardiovascular disease.
The dataset is separated into a training set of size
M, a test set of size N. A categorical variable c which
captures the class label of an instance i in the dataset.
In the context of this work, the investigating problem
has two possible classes, e.g., c = ”CVD” or ”Yes”
or c= ”Non-CVD” or ”No”. The features vector of
an instance i is captured by f
i
=
f
i1
, f
i2
, f
i3
, . . . , f
in
T
(with M n).
Our aim is to achieve high recall or sensitivity
and Area Under Curve (AUC) through supervised ma-
ICT4AWE 2022 - 8th International Conference on Information and Communication Technologies for Ageing Well and e-Health
316

chine learning, meaning that the CVD class can be
predicted correctly. Our methodology for CVD pre-
diction includes the following models which are ex-
plained below.
2.1 Naive Bayes
Naive Bayes (Dinesh et al., 2018) is a simple classifier
founded on the Bayes theorem that supposes highly
independent attributes known as predictors to achieve
probability maximization. The main interest is to find
the posterior probabilities
P(c
|
f
i1
, . . . , f
in
) =
P( f
i1
, . . . , f
in
|c)P(c)
P( f
i1
, . . . , f
in
)
(1)
where P( f
i1
, . . . , f
in
|c) =
∏
n
j=1
P( f
i j
|c) is the proba-
bility of predictors given class, P ( f
i1
, . . . , f
in
) is the
prior probability of predictors and P(c) is the prior
probability of class. The testing data is classified
based on the probability of association:
ˆc = argmaxP(c)
n
∏
j=1
P( f
i j
|c)
for c ∈ {CV D, Non −CV D},
2.2 Support Vector Machine
The SVM is a machine learning algorithm that has
been used in medicine due to its high classification
performance. It can be used to solve a binary classi-
fication problem (as the one investigated here), either
linear or non-linear using a Kernel function to map the
nonlinear data to high dimensional feature space. In
the linear case, the instances are separated with a hy-
perplane, called support vector, of the form w
T
f + b,
where w is n dimensional coefficient vectors normal
to the hyperplane of the surface and b is offset value
from the origin. The value of w and b are calculated,
and the linear discriminant function can be written as
g(w) = sign(w
T
f + b).
2.3 Logistic Regression
Logistic Regression predicts the class label of the in-
put features based on their values using a binary lo-
gistic regression model. Assuming p = P(c = ‘CVD),
log
b
(
p
1−p
) = β
0
+
∑
n
j=1
f
i j
β
j
, with (β
1
, β
2
, . . . , β
n
) be
the regression weights attached to features row vector
f
i
, i = 1, 2, . . . , M . Isolating p, if it is greater than the
threshold, it is set to CVDs class (Yes); otherwise, it
is set to Non-CVDs class (No). The β coefficients val-
ues of the logistic regression algorithm are estimated
from training data using maximum-likelihood estima-
tion.
2.4 Random Forest
The Random forest method (Yang et al., 2020) is a su-
pervised learning algorithm that can be employed for
the classification of instances as either CVD or Non-
CVD. A Random forest algorithm is an ensemble of
decision trees that are created on data samples. The
more decision trees are considered, the more robust
is the constructed forest. It combines the prediction
from each tree separately to finally select the best out-
come by means of majority voting.
3 DATASET DESCRIPTION
The training and test dataset for the cardiovascu-
lar diseases risk prediction model was constructed
based on the CVDs dataset (an open-source dataset
derived from Kaggle), which consists of 70000 par-
ticipants. It is a balanced dataset of approximately
equal healthy and diagnosed with CVD participants,
which contains 11 features (4 demographic, 4 ex-
amination, and 3 social history) which include age
(years), gender, weight (Kg) and height (m
2
) from
which BMI =
weight
(height)
2
was derived, cholesterol and
glucose levels characterized as normal, above normal
or well above normal, physical activity, drinking and
smoking habits with values yes or no, systolic and di-
astolic blood pressure (mmHg), physical activity. No-
tice that the blood pressure measurements have been
recorded at the moment of medical examination. To
identify linear correlations between the features and
the target class we employed Pearson’s correlation co-
efficient (CC) (Mukaka, 2012) defined as
C =
∑
N
i=1
(x
i
− ¯x)(y
i
− ¯y)
q
∑
N
i=1
(x
i
− ¯x)
2
∑
(y
i
− ¯y)
2
, (2)
where x
i
and y
i
are the values of features x and y for
the i-th individual.
The results presented in Table 2 were derived set-
ting an alpha value equal to 0.01 to compute a 99%
confidence interval. From Table 2, we verify high
linear dependence among BMI and weight features
as the corresponding coefficient is equal to 0.7620.
Also, a moderate correlation value of 0.4520 was ob-
served between glucose and cholesterol. A low corre-
lation value of 0.3400 was noted between smoke and
alcohol. Focusing on the CVD class and the features
that capture age and cholesterol, low correlation val-
ues are recorded (since 0.2 ≤ C ≤ 0.39 )from the cur-
rent dataset.
Furthermore, in Tables 4-8, the distributions of se-
lected participants considering different combinations
Cardiovascular Disease Risk Prediction with Supervised Machine Learning Techniques
317
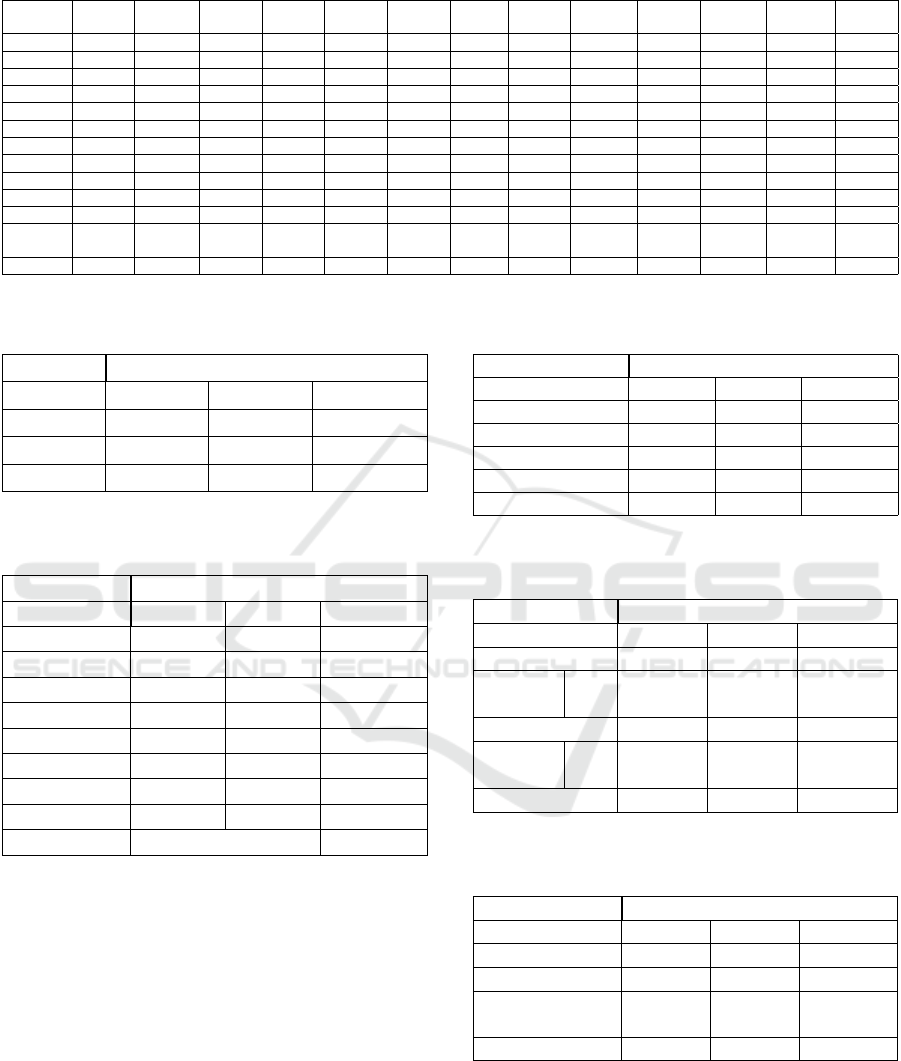
Table 2: Pearson Correlation Coefficients Matrix between the features and target CVD class.
Age Gender Height Weight BMI SBP DBP Chol Glucose Smoke Alcohol
Physical
Activity
CVD
Age 1.0000 -0.0230 -0.0810 0.0540 0.0850 0.0210 0.0180 0.1540 0.0990 -0.0480 -0.0300 -0.0100 0.2380
Gender -0.0230 1.0000 0.4990 0.1550 -0.0970 0.0060 0.0150 -0.0360 -0.0200 0.3380 0.1710 0.0060 0.0080
Height -0.0810 0.4990 1.0000 0.2910 -0.2910 0.0050 0.0060 -0.0500 -0.0190 0.1880 0.0940 -0.0070 -0.0110
Weight 0.0540 0.1550 0.2910 1.0000 0.7620 0.0310 0.0440 0.1420 0.1070 0.0680 0.0670 -0.0170 0.1820
BMI 0.0850 -0.0970 -0.2910 0.7620 1.0000 0.0250 0.0350 0.1460 0.1010 -0.0270 0.0140 -0.0140 0.1660
SBP 0.0210 0.0060 0.0050 0.0310 0.0250 1.0000 0.0160 0.0240 0.0120 -0.0010 0.0010 0 0.0540
DBP 0.0180 0.0150 0.0060 0.0440 0.0350 0.0160 1.0000 0.0240 0.0110 0.0050 0.0110 0.0050 0.0660
Chol 0.1540 -0.0360 -0.0500 0.1420 0.1460 0.0240 0.0240 1.0000 0.4520 0.0100 0.0360 0.0100 0.2210
Glucose 0.0990 -0.0200 -0.0190 0.1070 0.1010 0.0120 0.0110 0.4520 1.0000 -0.0050 0.0110 -0.0070 0.0890
Smoke -0.0480 0.3380 0.1880 0.0680 -0.0270 -0.0010 0.0050 0.0100 -0.0050 1.0000 0.3400 0.0260 -0.0150
Alcohol -0.0300 0.1710 0.0940 0.0670 0.0140 0.0010 0.0110 0.0360 0.0110 0.3400 1.0000 0.0250 -0.0070
Physical
Activity
-0.0100 0.0060 -0.0070 -0.0170 -0.0140 0 0.0050 0.0100 -0.0070 0.0260 0.0250 1.0000 -0.0360
CVD 0.2380 0.0080 -0.0110 0.1820 0.1660 0.0540 0.0660 0.2210 0.0890 -0.0150 -0.0070 -0.0360 1.0000
Table 3: Distribution per gender group of healthy and diag-
nosed with CVD in the dataset.
CVD
Gender No Yes Total
Female 32,73% 32,31% 65,04%
Male 17,30% 17,66% 34,96%
50,03% 49,97% 100,00%
Table 4: Distribution per age group of healthy and diag-
nosed with heart disease in the dataset.
CVD
Age Group No Yes Total
30-34 0,01% 0,00% 0,01%
35-39 0,45% 0,13% 0,58%
40-44 9,62% 4,12% 13,74%
45-49 7,04% 5,41% 12,46%
50-54 14,95% 12,64% 27,59%
55-59 10,23% 12,68% 22,91%
60-64 7,56% 14,65% 22,21%
65-69 0,16% 0,35% 0,50%
50,03% 49,97% 100,00%
of the features and the target classes (yes or no) are
presented. In Table 3, the 32.31% of participants that
suffer from CVD are women which are almost twice
greater than men with CVD.
Moving on to Table 4, it is shown that approxi-
mately 70% of the total participants are elderly (age
≥ 50) which is the target group of people that concern
the current study. From older participants, about 40%
belongs to the CVD class.
Table 5 presents a classification of participants ac-
cording to the values of systolic and diastolic blood
pressure. The current data has shown that about 45%
of the participants have been diagnosed with a CVD
and are categorized as hypertensive (I or II).
Table 6 shows the distribution of participants in
Table 5: Distribution per blood pressure category of healthy
and diagnosed with heart disease in the dataset.
CVD
Blood Pressure No Yes Total
Elevated 3,02% 1,45% 4,46%
Hypertension I 31,44% 25,60% 57,05%
Hypertension II 4,89% 19,87% 24,76%
Normal 10,68% 3,05% 13,73%
Total 50,03% 49,97% 100,00%
Table 6: Distribution of healthy and diagnosed with CVD
in relation to smoke and alcohol features in the dataset.
CVD
Smoke No Yes Total
No 45,40% 45,79% 91,19%
No 44,10% 44,36% 88,46%
Alcohol
Yes 1,30% 1,43% 2,73%
Yes 4,63% 4,18% 8,81%
No 3,16% 3,01% 6,16%
Alcohol
Yes 1,47% 1,18% 2,65%
50,03% 49,97% 100,00%
Table 7: Distribution of healthy and diagnosed with CVD
in relation to glucose level feature in the dataset.
CVD
Glucose level No Yes Total
Normal 41,90% 32,94% 74,84%
Above Normal 5,43% 8,21% 13,64%
Well Above
Normal
2,70% 8,82% 11,52%
50,03% 49,97% 100,00%
Non-CVD and CVD classes according to smoke and
alcohol features. Here, it should be noted that a small
percentage of participants (1.18%) diagnosed with
CVD are simultaneous smokers and consume alcohol.
Tables 7, 8 show the distribution of participants
in Non-CVD and CVD classes according to glucose
ICT4AWE 2022 - 8th International Conference on Information and Communication Technologies for Ageing Well and e-Health
318
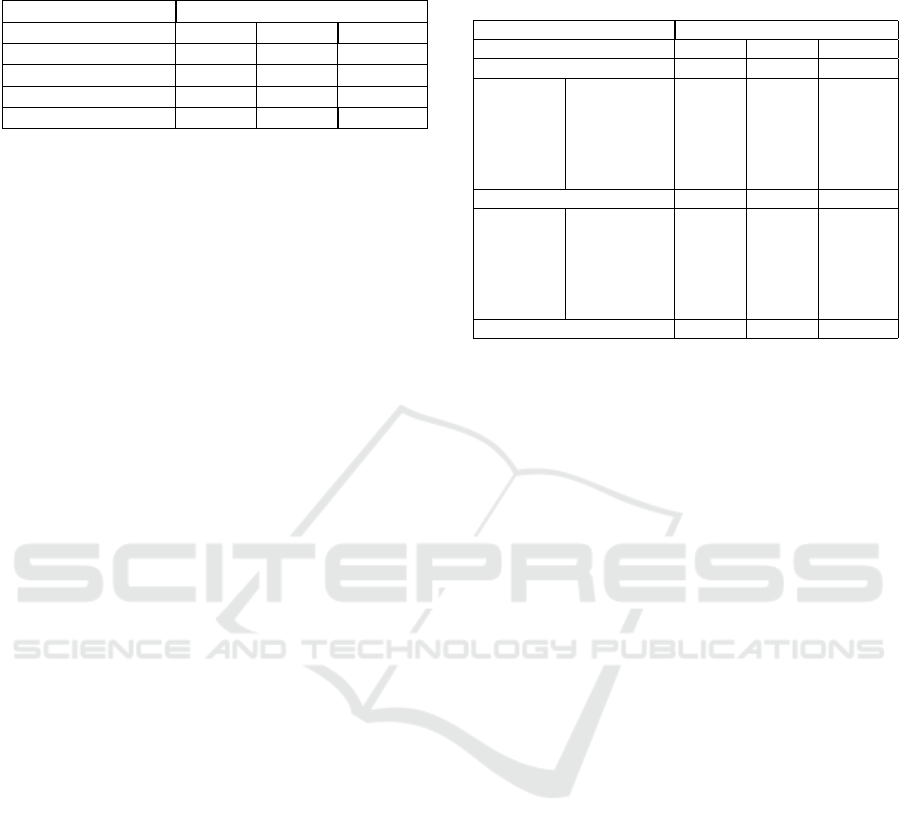
Table 8: Distribution of healthy and diagnosed with CVD
in relation to cholesterol level feature in the dataset.
CVD
Cholesterol level No Yes Total
Normal 41,90% 32,94% 74,84%
Above Normal 5,43% 8,21% 13,64%
Well Above Normal 2,70% 8,82% 11,52%
50,03% 49,97% 100,00%
and cholesterol features. Here, it should be noted that
a small percentage of participants (1.18%) diagnosed
with CVD are simultaneous smokers and consume al-
cohol. Moreover, there is no knowledge of the amount
of consumption to understand to what extent the par-
ticipants’ habits are harmful to their health.
Table 9 records the distribution of participants in
Non-CVD and CVD classes according to physical ac-
tivity and BMI classes. It is observed that 11,55%
of participants although they belong to healthy BMI
class and are physically active, they have been di-
agnosed with CVD. Also, in obese and overweight
classes, the number of participants diagnosed with
CVD is approximately similar. Both in this case,
there is no knowledge of exercise-related character-
istics (intensity, duration, frequency, type) to under-
stand to what extent physical activity can be beneficial
for CVD patients health.
Finally, it should be highlighted that the small per-
centage of participants with CVD who smokes, con-
sumes alcohol and is physical activity in Table 3 is re-
flected as negatively low correlation with CVD class.
4 DATA PREPROCESSING
The data preprocessing was evaluated using Stata
V.14 tool kit. Stata is a general-purpose statisti-
cal software package developed by StataCorp for
data manipulation, visualization, statistics, and auto-
mated reporting. The constructed training and testing
dataset, which is based on the CVDs dataset, was cre-
ated by studying all attributes that are correlated and
potentially relevant for the identification of Cardio-
vascular Diseases. In order to establish a unified set
of attributes for each participant, we derived harmo-
nized variables for each attribute, by transforming all
numeric values to nominal values, according to prede-
fined attribute rules. Moreover, the class was created
based on CVD’s dataset cardiovascular diseases fea-
ture. The class distribution is balanced containing in
total 70,000 observations.
In order to examine all attributes’ correlation with
the class, we used a feature selection method that
ranks all attributes with respect to the relevance to
the specific class. More specific, we utilized a fea-
Table 9: Distribution of healthy and diagnosed with CVD
in relation to Physical Activity level and BMI class in the
dataset.
CVD
Physical Activity No Yes Total
No 9,11% 10,52% 19,63%
BMI Class Underweight 0,10% 0,05% 0,15%
Overweight 3,22% 3,71% 6,93%
Obese III 0,16% 0,45% 0,61%
Obese II 0,41% 0,90% 1,31%
Obese I 1,22% 2,27% 3,49%
Healthy 4,01% 3,14% 7,15%
Yes 40,92% 39,45% 80,37%
BMI Class Underweight 0,56% 0,21% 0,77%
Overweight 14,41% 14,63% 29,04%
Obese III 0,68% 1,41% 2,09%
Obese II 1,61% 3,36% 4,97%
Obese I 5,71% 8,29% 14,00%
Healthy 17,95% 11,55% 29,51%
50,03% 49,97% 100,00%
ture selection method based on a variation of Ran-
dom Forests (Genuer et al., 2010) and according to
this method, the attributes are ranked using the Gini
importance score of the model’s trees. The Gini in-
dex (Sundhari, 2011) is estimated as follows
Gini = 1 −
c
∑
i=1
p
2
i
, (3)
where c is the number of classes and p
i
is the relative
frequency of class i in the dataset. In our case param-
eter c = 2 captures the CVDs and non-CVDs classes.
5 EXPERIMENTS AND
EVALUATION
5.1 Experiments Setup
The experiments were evaluated using WEKA.
WEKA is a JAVA-based data mining toolkit created
and free software tool distributed under the GNU
General Public License that provides a large library of
methods and models for classification, clustering, pre-
diction, feature selection. For the purposes of this ex-
periment, we split the dataset into two parts, 30% test-
ing and 70% training. To do that, we first randomized
the dataset, in order to create a random permutation.
Then, we applied the RemovePercentage method with
30% and saved the resulting dataset as training. We
also applied the same filter choosing invertSelection
in order to pick the rest of the data (30%) which is the
testing dataset.
Cardiovascular Disease Risk Prediction with Supervised Machine Learning Techniques
319
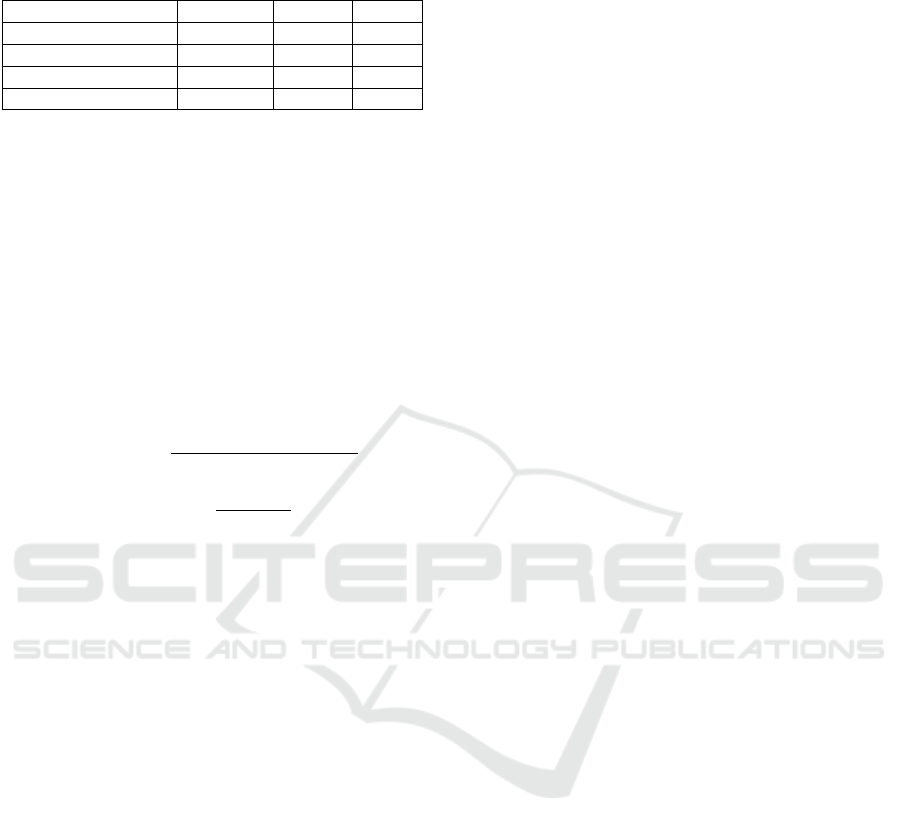
Table 10: Performance of ML models for CVDs risk pre-
diction.
Algorithm Accuracy Recall AUC
Naive Bayes 59.59% 59.60% 69.4%
SVM 70.61% 70.60% 70.6%
Random Forest 70.86% 70.90% 76.6%
Logistic Regression 72.06% 72.10% 78.4%
5.2 Experiments Results
For the specific experiment, accuracy, recall and AUC
were considered as performance metrics. Also, the
10-fold cross-validation procedure was used to eval-
uate four different classifiers: Na
¨
ıve Bayes, SVMs,
Logistic Regression and Random Forests. The mod-
els’ evaluation is executed based on the confusion ma-
trix, namely TP (True Positive), TN (True Negative),
FP (False Positive) and FN (False Negative). More
specifically, the measures used for the calculation of
the accuracy and recall are defined as
Accuracy =
(T N + T P)
(T N + T P + FN + FP)
(4)
Recall =
T P
T P + FN
(5)
The performance results of the ML algorithms, in
terms of the employed metrics, are shown in Table
10. The predictive ability of the Logistic Regression
model in cardiovascular diseases is promising and su-
perior in terms of accuracy, recall and AUC against
the rest of the ML models. The higher the AUC, the
better the performance of the model at distinguishing
between CVD and Non-CVD classes. In particular,
AUC shows that there is a 78.4% chance that the Lo-
gistic Regression model will be able to distinguish be-
tween CVD and Non-CVD classes.
6 CONCLUSIONS
In the context of this research study, a supervised ma-
chine learning methodology was employed and prop-
erly designed to assess the long-term risk of occur-
ring CVD. The outcomes of the study may provide
useful information in the clinic viewpoint and assist
clinicians in how to interpreting data and implement-
ing optimal algorithms for the dataset (Al’Aref et al.,
2019).
It is ongoing research in which, as a first step, sev-
eral traditional models were developed to investigate
data quality and determine that model with the best
predictive performance. The current outcomes will be
used to design the next steps of our research and iden-
tify the optimal models to improve the performance
metrics. The evaluation results presented similar ac-
curacy and recall, a fact that is justified by the bal-
anced distribution of participants into two classes. A
promising direction for enhancing the achieved out-
comes (accuracy, recall, AUC) is the utilization of
deep learning models and techniques (Swathy and
Saruladha, 2021), as they can provide complex de-
cision boundaries and thus better fit the training data.
Finally, our aim is to focus our analysis on i) anomaly
detection techniques to identify instances with in-
correct values and ii) dimensionality reduction tech-
niques to optimize the performance of ML models.
ACKNOWLEDGEMENTS
This work has been partially supported by the
European Union’s H2020 research and innovation
programme SmartWork under grant agreement No
826343, SC1-DTH-03-2018 - Adaptive smart work-
ing and living environments supporting active and
healthy ageing and GATEKEEPER under grant
agreement No 857223, SC1-FA-DTS-2018-2020 -
Smart living homes-whole interventions demonstra-
tor for people at health and social risks.
REFERENCES
Abdalrada, A. S., Abawajy, J., Al-Quraishi, T., and Islam,
S. M. S. (2022). Machine learning models for predic-
tion of co-occurrence of diabetes and cardiovascular
diseases: a retrospective cohort study. Journal of Di-
abetes & Metabolic Disorders, pages 1–11.
Al’Aref, S. J., Anchouche, K., Singh, G., Slomka, P. J.,
Kolli, K. K., Kumar, A., Pandey, M., Maliakal, G.,
Van Rosendael, A. R., Beecy, A. N., et al. (2019).
Clinical applications of machine learning in cardio-
vascular disease and its relevance to cardiac imaging.
European heart journal, 40(24):1975–1986.
Dinesh, K. G., Arumugaraj, K., Santhosh, K. D., and
Mareeswari, V. (2018). Prediction of cardiovascu-
lar disease using machine learning algorithms. In
2018 International Conference on Current Trends to-
wards Converging Technologies (ICCTCT), pages 1–
7. IEEE.
Dritsas, E., Fazakis, N., Kocsis, O., Fakotakis, N., and
Moustakas, K. (2021). Long-term hypertension risk
prediction with ml techniques in elsa database. In
International Conference on Learning and Intelligent
Optimization, pages 113–120. Springer.
Fazakis, N., Kocsis, O., Dritsas, E., Alexiou, S., Fakotakis,
N., and Moustakas, K. (2021). Machine learning tools
for long-term type 2 diabetes risk prediction. IEEE
Access, 9:103737–103757.
Gale, C. R., Cooper, C., and Sayer, A. A. (2014). Fram-
ingham cardiovascular disease risk scores and incident
ICT4AWE 2022 - 8th International Conference on Information and Communication Technologies for Ageing Well and e-Health
320

frailty: the english longitudinal study of ageing. Age,
36(4):1–9.
Genuer, R., Poggi, J.-M., and Tuleau-Malot, C. (2010).
Variable selection using random forests. Pattern
recognition letters, 31(14):2225–2236.
Haq, A. U., Li, J. P., Memon, M. H., Nazir, S., and Sun,
R. (2018). A hybrid intelligent system framework for
the prediction of heart disease using machine learning
algorithms. Mobile Information Systems, 2018.
Hoyas, I. and Leon-Sanz, M. (2019). Nutritional challenges
in metabolic syndrome. Journal of clinical medicine,
8(9):1301.
Hussain, A., Ugli, I. K. K., Kim, B. S., Kim, M., Ryu, H.,
Aich, S., and Kim, H.-C. (2021). Detection of dif-
ferent stages of copd patients using machine learning
techniques. In 2021 23rd International Conference
on Advanced Communication Technology (ICACT),
pages 368–372. IEEE.
Kocsis, O., Moustakas, K., Fakotakis, N., Vassiliou, C.,
Toska, A., Vanderheiden, G. C., Stergiou, A., Amaxi-
latis, D., Pardal, A., Quintas, J., et al. (2019). Smart-
work: designing a smart age-friendly living and work-
ing environment for office workers. In Proceedings
of the 12th ACM International Conference on PErva-
sive Technologies Related to Assistive Environments,
pages 435–441.
Kumar, M. D. and Ramana, K. (2021). Cardiovascular
disease prognosis and severity analysis using hybrid
heuristic methods. Multimedia Tools and Applica-
tions, 80(5):7939–7965.
Mohan, S., Thirumalai, C., and Srivastava, G. (2019). Ef-
fective heart disease prediction using hybrid machine
learning techniques. IEEE access, 7:81542–81554.
Mukaka, M. M. (2012). A guide to appropriate use of corre-
lation coefficient in medical research. Malawi medical
journal, 24(3):69–71.
Roth, G. A., Johnson, C., Abajobir, A., Abd-Allah, F.,
Abera, S. F., Abyu, G., Ahmed, M., Aksut, B., Alam,
T., Alam, K., et al. (2017). Global, regional, and na-
tional burden of cardiovascular diseases for 10 causes,
1990 to 2015. Journal of the American College of Car-
diology, 70(1):1–25.
Sundhari, S. S. (2011). A knowledge discovery using de-
cision tree by gini coefficient. In 2011 International
Conference on Business, Engineering and Industrial
Applications, pages 232–235. IEEE.
Swathy, M. and Saruladha, K. (2021). A comparative study
of classification and prediction of cardio-vascular dis-
eases (cvd) using machine learning and deep learning
techniques. ICT Express.
Wilkins, E., Wilson, L., Wickramasinghe, K., Bhatnagar,
P., Leal, J., Luengo-Fernandez, R., Burns, R., Rayner,
M., and Townsend, N. (2017). European cardiovascu-
lar disease statistics 2017.
Yancy, C. W., Jessup, M., Bozkurt, B., Butler, J., Casey,
D. E., Drazner, M. H., Fonarow, G. C., Geraci, S. A.,
Horwich, T., Januzzi, J. L., et al. (2013). 2013
accf/aha guideline for the management of heart fail-
ure: a report of the american college of cardiology
foundation/american heart association task force on
practice guidelines. Journal of the American College
of Cardiology, 62(16):e147–e239.
Yang, L., Wu, H., Jin, X., Zheng, P., Hu, S., Xu, X., Yu, W.,
and Yan, J. (2020). Study of cardiovascular disease
prediction model based on random forest in eastern
china. Scientific reports, 10(1):1–8.
Cardiovascular Disease Risk Prediction with Supervised Machine Learning Techniques
321
