
Modeling Doctor-patient Shared Decision-making as Fuzzy
Constraint-based Agent Negotiation
Yong Liu
1a
, Ping Lu
1b
, Yimin Yang
2c
, Feiping Hong
3d
and Kaibiao Lin
1,* e
1
School of Computer and Information Engineering, Xiamen University of Technology, Xiamen, China
2
Department of Pediatrics, Xiamen Hospital of Traditional Chinese Medicine, Xiamen, China
3
Department of Neonates, Xiamen Humanity Hospital, Xiamen, China
yym216@126.com, 136897915@qq.com, kblin@xmut.edu.cn
Keywords: Shared Decision-Making, Fuzzy Constraints, System Structure, Agent Negotiation, Recommendation.
Abstract: Shared decision-making (SDM) has been widely advocated as a new medical decision-making model, but
limited time, uncertain information, and individual differences constrain its application and development.
To facilitate the application of SDM, a multi-issue agent negotiation approach based on fuzzy constraints is
proposed to solve the SDM problem between doctors and patients. The advantages of our approach can be
summarized into three points: 1) a general framework for knowledge representation and problem-solving in
SDM simulation; 2) a feasible system structure that includes negotiation and recommendation model, which
can simulate a real clinical scenario to complete SDM; 3) an efficient negotiation model that can improve
the negotiation efficiency of SDM by alleviating the constraints of issues and time and reducing the impact
of space and emotion. To verify the feasibility and effectiveness of our method, we simulated and solved the
asthma SDM between doctors and patients and then validated its performance under different deadlines and
issues constraints.
1 INTRODUCTION
1
Evidence-based medicine encourages patients to
participate actively in discussions of diagnosis,
treatment, and follow-up (Hoffmann et al. 2014). On
this premise, as a new medical decision-making
model in which doctors and patients participate and
fully negotiate about diagnosis and treatment, shared
decision-making (SDM) has received extensive
attention. Different from the paternalistic medical
decision-making model and informed consent
decision-making model, SDM is a patient-centered
decision-making model (Weston 2001). It aims to
make decision-making consistent with patients'
values to improve their compliance and strengthen
doctor-patient communication to promote the
harmony of the doctor-patient relationship
(Stiggelbout et al. 2015).
a
https://orcid.org/0000-0002-6839-4769
b
https://orcid.org/0000-0001-5666-0348
c
https://orcid.org/0000-0002-1830-5190
d
https://orcid.org/0000-0002-9453-1173
e
https://orcid.org/0000-0003-2648-2960
The studies on SDM mainly focus on the
establishment of theory and the development of the
application. The concept of SDM was first proposed
by Reimann (Reimann 1968) in 1968, defined by
Veatch (Veatch 1972) in 1972, and then perfected by
the American government in 1982 (States 1982).
Since then, many scholars have begun to enrich and
improve relevant theories, such as the Makoul model
(Makoul and Clayman 2006), the Talking model
(Elwyn et al., 2013), and the Stiggelbout model
(Stiggelbout et al. 2015). To promote the clinical
application of SDM, patient decision aids (O'Connor
2000, Poprzeczny et al. 2020), evaluation tools
(Scholl et al. 2012, Barr et al. 2014), auxiliary
standards, and laws (Holmes-Rovner 2007) have
been studied and developed.
Although the theoretical system of SDM has
been mature and widely used in the clinic, there are
still many problems to be solved (Pieterse et al.
2019). For example, uneven distribution of medical
resources, lack of awareness of doctor-patient
communication, limited time of doctors, lack of
medical knowledge of patients, etc. These problems
cannot be completely solved, and we can only
48
Liu, Y., Lu, P., Yang, Y., Hong, F. and Lin, K.
Modeling Doctor-patient Shared Decision-making as Fuzzy Constraint-based Agent Negotiation.
DOI: 10.5220/0011228100003438
In Proceedings of the 1st International Conference on Health Big Data and Intelligent Healthcare (ICHIH 2022), pages 48-55
ISBN: 978-989-758-596-8
Copyright
c
2022 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved

reduce the impact of these uncertain factors on the
clinical application of SDM.
The negotiations involved in SDM mainly take
place between doctors and patients. To make SDM
in-network and promote the theoretical study and
clinical application of SDM, a fuzzy constraint-
directed agent-based negotiation (FCAN) model and
a recommendation model for bilateral SDM are
proposed in this paper. We model the shared
decision-making problems (SDMPs) as distributed
fuzzy constraint satisfaction problems (DFCSPs) to
implement SDM and achieve treatment plan
recommendations to objectify SDM. The doctor
agent (DA) and the patient agent (PA) are designed
to interact in the form of offer and counteroffer until
they reach an agreement or withdraw from
negotiations. Then, we match the agreement with the
existing treatment plans by calculating the
recommendation score to achieve the
recommendation of the treatment plans.
The main advantages of this paper can be
summarized into three points. First, it provides a
general framework for knowledge representation and
problem-solving for SDM simulation. Second, a
distributed computing model including negotiation
algorithm and recommendation algorithm is
established, which simulates SDM in the real world
more closely and naturally. Thirdly, an efficient
negotiation model is proposed to relax the
constraints of negotiation issues and time and
improve the negotiation efficiency. In addition, the
negotiation model can effectively reduce the
influence of space and the negotiator's emotions on
negotiation because of its automaticity.
The rest of this paper is organized as follows.
Section 2 generalizes the proposed methods. Section
3 describes the complete process of solving the
SDM problem with the proposed method. It includes
the problem formulation, negotiation and
recommendation strategies, interaction mechanism,
and system structure. Section 4 proves the feasibility
and effectiveness of our method applied to SDM by
an example and comparative test. Section 5
summarizes this paper.
2 METHODS
Study Subjects
The subjects were doctors and patients attending
the treatment for chronic diseases. Significantly, the
eligible patients with light or moderate conditions.
Ethical Requirement
This study was approved by the Medical Ethics
Committee of Xiamen Hospital of Traditional
Chinese Medicine, China, and the approval number
is 2021-K065-01. In addition, all participants
provided written informed consent after a complete
description of the study. There was no financial
compensation for the doctors and the patients.
Study Design
This study was designed as an exploratory study
to solve the problems of doctor-patient SDM
according to the agent negotiation and fuzzy
constraints. Thus, it is necessary to establish an
agent negotiation and recommendation method
based on fuzzy constraints for SDM (Section 3) and
validate it by experiments (Section 4). The proposed
method includes four parts: problem formulation
(Section 3.1), negotiation and recommendation
strategies (Section 3.2), interaction mechanism
(Section 3.3), and system structure (Section 3.4).
The experiments consist of two parts: an illustration
for judging its feasibility (Section 4.1) and a
negotiation performance comparison for evaluating
its effectiveness (Section 4.2).
Data Collection
The experimental data in this paper was related
to childhood asthma and were obtained from the
Department of Pediatrics at Xiamen Hospital of
Traditional Chinese Medicine. It consists of the
preference data of doctors and patients on issues and
the evaluation data of treatment plans provided by
doctors. In addition, the treatment plans come from
the Diagnosis and Treatment Guidelines of Asthma
published in 2016 (The Respiratory Group 2016).
Results Evaluation
The evaluation index of treatment
recommendation is the recommendation score. The
evaluation indicators of negotiation performance are
the combined ASV (the sum of DA's ASV and PA's
ASV) and the number of negotiation rounds.
3 FUZZY CONSTRAINT-BASED
AGENT NEGOTIATION FOR
SDM
In this section, we will introduce our proposed
method in detail. Our problem formulation is
summarized in Section 3.1. It describes the
theoretical basis of modeling SDM as DFCAN.
Section 3.2 introduces the negotiation and
recommendation strategies of our method that is the
behavior framework of the DA and PA. Section 3.3
Modeling Doctor-patient Shared Decision-making as Fuzzy Constraint-based Agent Negotiation
49
presents the interaction mechanism between the DA
and PA. Section 3.4 develops a system structure for
a prototyped agent-based SDM simulator.
3.1 Problem Formulation
Agent-based negotiation technology has been
successfully applied to solve the problems of
resource allocation (Voos 2006), e-commerce (Ateib
2010), cloud computing (Shojaiemehr et al. 2019),
etc. In clinical practice, SDMP is actually a problem
that needs to be negotiated by doctors and patients.
Thus, based on the agent concept (Wooldridge and
Jennings 1995), SDMP can be transformed into the
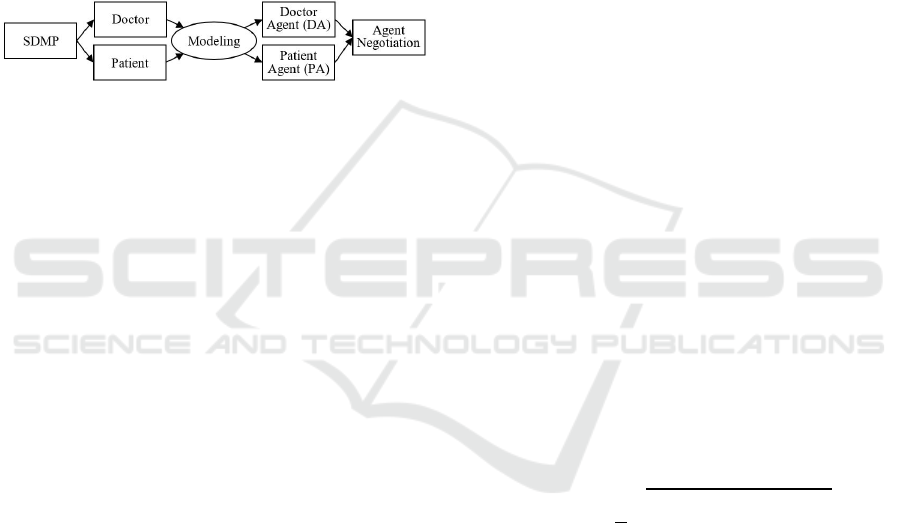
agent negotiation problems shown in Figure 1.
Figure 1: Problem conversion.
Furthermore, the real-world clinical environment
is heterogeneous, distributed, and with a great deal
of uncertain and inaccurate information. Therefore,
in our work, SDMP can be modeled as DFCSP. The
task of SDM simulation is to explore a satisfactory
agreement that meets all constraints and then make a
decision on treatment plans. A negotiation for
treatment in SDM can be modeled as a triple
(𝒟,𝒫,ℐ), where 𝒟 and 𝒫 represent the DA and PA,
respectively, and ℐ is the inter-relationships between
the two types of agents. The distributed fuzzy
constraint networks (DFCNs) are defined as follows.
Definition 1: A DFCN (𝑈,𝑋,𝐶) in a SDM
(𝒟,𝒫,ℐ) can be defined as a set of fuzzy constraint
networks (FCN) {𝑁
,...,𝑁
,...,𝑁
}, where 𝑁
=
(𝑈
,𝑋
,𝐶
) belongs to agent 𝑙, and
𝑈
is the universe of discourse for FCN, 𝑁
;
𝑋
={𝑋
,...,𝑋
,...,𝑋
} is a tuple of 𝑛 non-
recurring objects; and
𝐶
is a set of fuzzy constraints in the FCN, which
includes the internal constraints among objects in 𝑋
and external constraints between agent and its
opponent;
𝑈 is the universe of discourse for DFCN;
𝑋=(𝑈
𝑋
) is a tuple of all non-recurring
objects; and
𝐶=(𝑈
𝐶
) is a set of all fuzzy constraints in
the DFCN.
As stated in Definition 1, the solution to 𝑋
,
FCN, can be regarded as an intention Π
or Π
,
indicating that fuzzy set 𝑋
of non-recurring objects
satisfies all fuzzy constraints 𝐶
.
3.2 Negotiation and Recommendation
Strategies
Following the description of FCSP of SDM, the
FCAN model and recommendation model for SDM
can be described as follows.
Given an issue set 𝐼={𝐼
,𝐼
,…,𝐼
,…,𝐼
} and an
offer (or a counteroffer) 𝑆𝜖Π
, the aggregated
satisfaction value (ASV) about 𝑆 of agent 𝑙 is:
Ψ
(
𝑆
)
=𝑤
∗𝜇
(𝑆)
(1)
Where 𝜇
(𝑆) is the 𝑖
satisfaction degree
function of 𝑆, fuzzy membership function, 𝑛 is the
number of issues, and 𝑤
is the weight factor for 𝑖
issue.
For an auto-negotiation, the agent will determine
its new behavior state and generate a set of feasible
solutions by reducing its demands to reach an
agreement with its opponent. The feasible solution
set is the solution space, in which agents can explore
to a satisfactory consensus. Given FCN 𝑁, intention
Π, and a new behavior state 𝜀
∗
=𝜀−∆ε, a set of
feasible solutions 𝑃 can be acquired by:
𝑃=Γ
(
𝛱,𝜀
∗
)
={𝑆|(𝑆𝜖𝛱)Λ(𝜀≥Ψ
(
𝑆
)
≥𝜀
∗
)}
(2)
Where, 𝜀 is the behavior state in the last round,
and ∆𝜀 is the concession value.
In the offer exchange round, the agent trends to
select an "optimal" offer from the feasible solution
set to maximize their individual interest. The
selection condition can be defined as:
𝑆
∗
=𝑎𝑟𝑔(𝑚𝑎𝑥
∈
𝐻(𝑆,𝐵))
(3)
Where 𝐻(𝑆,𝐵) is a utility function that can
evaluate the similarity between counteroffer 𝐵 and
feasible solution 𝑆. It can be calculated by:
(
𝑆,𝐵
)
=1−
1
𝑛
(1−𝐷(
𝐴
,𝐵
))
(4)
Where 𝐴
and 𝐵
are the possibility distributions
of offer 𝐴 and counteroffer 𝐵 over the issue 𝐼
𝜖𝐼,
respectively, and 𝐷 is the distance measure between
a feasible solution 𝐴∈𝑆 (i.e., 𝐴
) and a counteroffer
𝐵 (i.e., 𝐵
).
The negotiation result between the DA and PA is
an agreement on the value of all issues. However,
the purpose of real SDM is to obtain a treatment
plan that meets the preferences of both sides and
conforms to the patient's condition. Therefore, we
need to translate the results of the negotiations into
treatment plans for doctors and patients to make
decisions. The conversion method is as follows.
ICHIH 2022 - International Conference on Health Big Data and Intelligent Healthcare
50
(
𝑆,𝐵
)
=1−
1
𝑛
(1−𝐷(
𝐴
,𝐵
))
(5)
Where 𝑤
is the weight of the relevant issues
concerning treatment plans, and 𝑅
(
𝑆
)
∈[0,1] is the
similarity calculation on the negotiation issue level,
that is, the fuzzy membership function related to the
treatment plans.
3.3 Interaction Mechanism
The above-mentioned negotiation process can be
summarized as a universal negotiation and
recommendation algorithm for the DA and PA,
which describes the method adopted by the DA and
PA in the negotiation process. Therefore, based on
the strategies given in Section 3.2, Algorithm 1
presents the details of the interaction process
between the DA and PA.
Initially, the negotiator will send a message with
the initial offer to its opponent. When its opponent
receives the message, it first determines the type of
the message. If it is an "Abort" message, it means
that the other party withdraws from the negotiation,
and the negotiation fails. If it is an "Accept"
message, it means that the other party agrees to
reach an agreement, and the negotiation is
terminated in a successful state. Otherwise, the
opponent will generate a set of feasible solutions and
judge whether it can reach an agreement with the
other party. If it can, it will send an "Accept"
message; if not, it will decide whether to generate
the "Ask" message with a new offer according to the
current time state. For another negotiator, the
response process is similar. The above negotiation
process will be repeated until the negotiation status
is failed or successful.
Al
g
orithm 1: Interaction Al
g
orithm
1: negotiation state "normal"
2: activate Timer 𝑇
3: generate an initial offer 𝐴
or 𝐵
and send it in
"Ask" to the opponent agent
4: Repeat
5: receive a message from its opponent
6: if the message is an "Abort", then
7: negotiation state "failure"
8: else if the message is an "Accept", then
9: negotiation state "success"
10: else
11: get a counteroffer 𝐵 or 𝐴 from the received
message
12: generate a new feasible set 𝑃
13: if 𝒟 and 𝒫 reach an agreement, then
14: send an "Accept" message with the agreement 𝑆
15: negotiation state "success"
16: else if Timer 𝑇 is counting, then
17: generate a new offer 𝐴 or 𝐵 based on feasible
set 𝑃
18: send an "Ask" message with the new offer 𝐴 or
𝐵
19: else
20: negotiation state "failure"
21: end if
22: end if
23: until the state is "success" or "failure"
3.4 System Structure
In the clinical environment, fuzzy-directed agent-
based automatic negotiation is an open simulation
platform for simulating SDM between doctors and
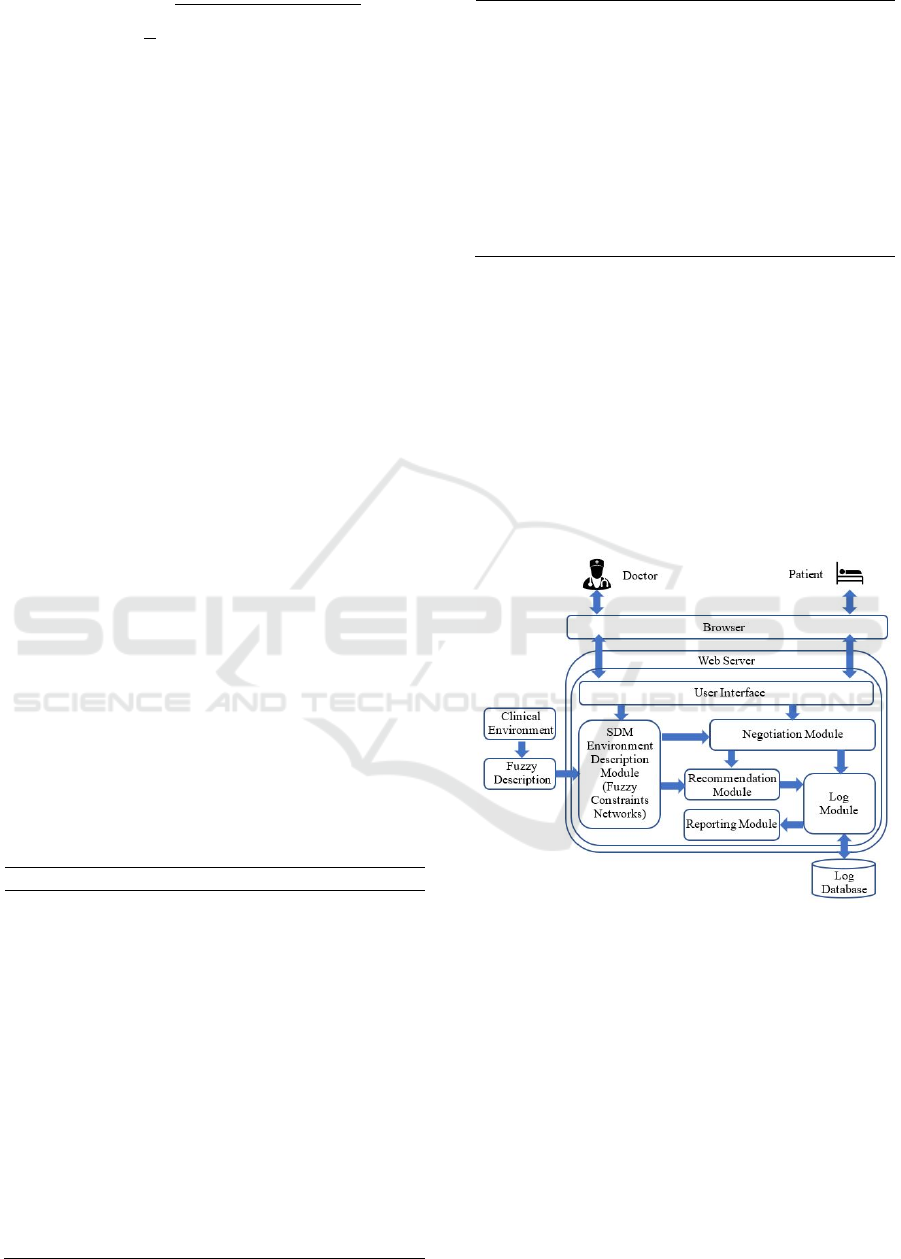
patients. Figure 2 shows the structure of agent-based
negotiation for simulating SDM. In this figure, based
on the fuzzy description, the SDM Environment
Description Module can transform the clinical
environment (including the description of clinical
situations, disciplines, and rules) into the fuzzy
constraint network.
Figure 2: A system structure of SDM.
In the Negotiation Module, the DA and PA will
comply with the negotiation protocols to solve their
own FCSP by exchanging the offer and counteroffer
in the transformed clinical environment. In the
negotiation process, if the agent cannot reach an
agreement with its opponent in the current round, it
will relax its constraints, adopt a concession
strategy, and explore alternative agreements.
Meanwhile, the agent will update its cognition of the
opponent and the environment and modify its
negotiation status in the next round. The details can
be seen in Sections 3.1 to 3.3.
Modeling Doctor-patient Shared Decision-making as Fuzzy Constraint-based Agent Negotiation
51
When the DA and PA reach an agreement, the
Recommendation Module is applied to convert the
negotiation result into treatment plans and
accomplish the recommendation of treatment plans.
In this module, the recommendation scores of
treatment plans will be calculated and ranked.
The Log Module records the relevant data of the
Negotiation Module and Recommendation Module
into log files. The negotiation data includes the
process and results, and the recommendation data
includes all the recommended results. The
Reporting Module will generate a detailed report
according to the results of negotiation and
recommendation and send it to doctors and patients,
respectively. Finally, doctors and patients can
evaluate each other and make treatment decisions.
4 EXPERIMENTS
After defining the model and system structure, the
next step is to evaluate it. Given the purpose of our
work, we evaluated our method from the perspective
of feasibility and effectiveness. On the one hand, we
judged its feasibility by an illustration, as shown in
Section 4.1; on the other hand, we evaluated its
effectiveness by negotiation performance, as shown
in Section 4.2. Additionally, the clinical decision-
making scene used in the experiment was the SDM
of doctors and patients on the treatment of childhood
asthma. There are two roles, doctor and patient,
corresponding to the DA and PA, respectively.
4.1 An Illustration for Agent-based
SDM
The following content provides a case to illustrate
the application of the framework proposed in this
paper in simulating and solving SDM problems. For
negotiation, the initial satisfaction threshold of both
DA and PA is set to 1.0, the satisfaction retention
value is 0.0, and the maximum number of rounds is
15. Negotiated issues include cost, effectiveness,
side effects, risk, and convenience (Rivera-Spoljaric
et al. 2014).
According to the negotiation algorithm, the
negotiation is terminated when the DA and PA reach
an agreement, or the negotiator withdraws from the
negotiation, or the negotiation round is exceeded.
After full negotiation, the negotiation result between
the DA and PA is [Cost: 3.78, Effective: 9, Side-
effects: 0.06, Risk: 0.07, Convenience: 9], because
the ASV of DA for the received offer is greater than
its satisfaction threshold.
As mentioned above, the negotiation result is not
the real purpose of SDM. Thus, the
Recommendation Module will be applied to address
the problem of treatment recommendation. The final
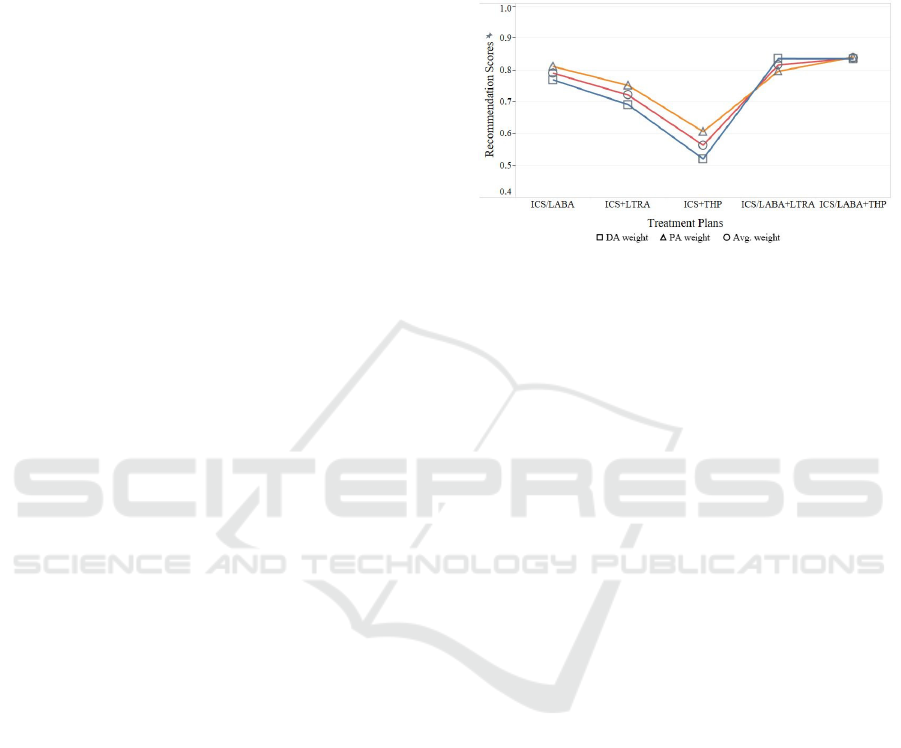
recommended results of treatment plans are shown
in Figure 3.
Figure 3: The recommendation scores of treatment plans
in different priority constraints [with the weights of issues
of DA, PA, and their average].
The recommended order of treatment plans is:
En-high dose ICS/LABA + Sustained-release
THP ≽ En-high dose ICS/LABA+LTRA ≽ En-high
dose ICS/ LABA ≽ En-high dose ICS+LTRA ≽ En-
high dose ICS + Sustained-release THP.
Where ICS means inhaled corticosteroid, LABA
is long-acting beta2-agonists, LTRA is leukotriene
receptor antagonists, THP is theophylline, and
ICS/LABA means a combination of inhaled
corticosteroids and long-acting beta2-agonists.
4.2 Negotiation Evaluation
To evaluate the effectiveness of our SDM
negotiation method, we compare it with the Time
model (time-dependent negotiation model) (Faratin
et al. 1998) in terms of negotiation rounds and
combined ASV. All the experimental results were
the average results of 200 repeated experiments. The
first experiment compared the negotiation
performance of agents on different issues but
subjects to the same deadline. The second
experiment compared the negotiation performance
of agents on the same issues but subjects to different
deadlines. Here, the negotiation environment is
defined by the number of issues (between 1 and 9)
and the number of deadlines (between 10 and 30).
The range of these parameters is selected according
to the experience of experts in the SDM field.
As shown in Figures 4 and 5, it can be seen that
when the FCAN model and Time model negotiate
on different issues (the number of issues is between
1 and 9) and subject to the same deadline
ICHIH 2022 - International Conference on Health Big Data and Intelligent Healthcare
52
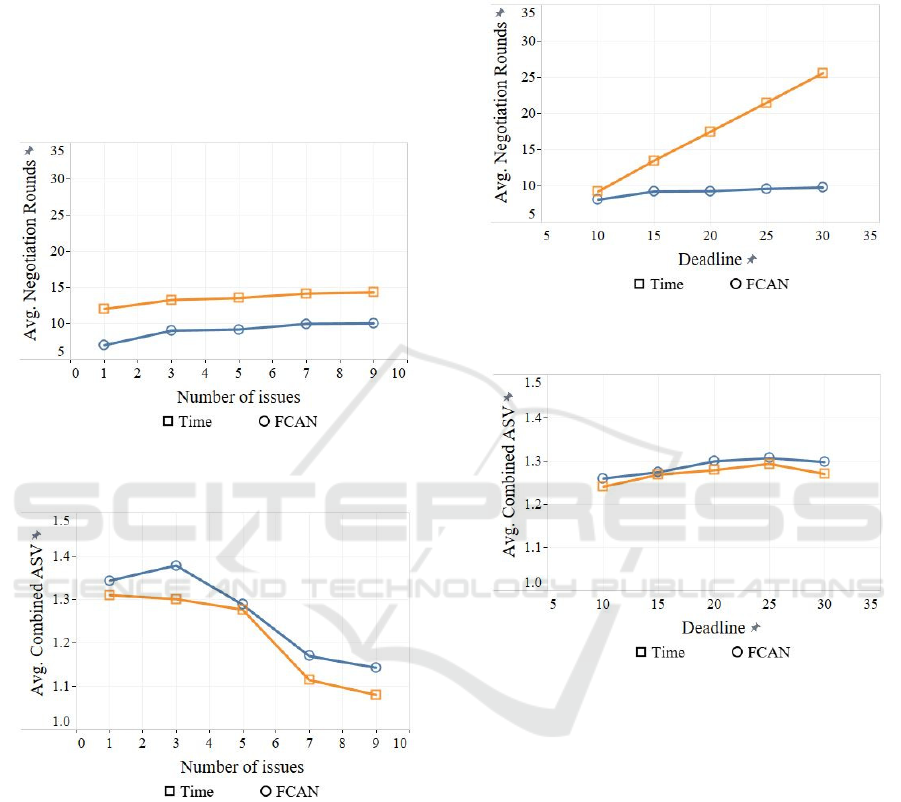
constraints, the negotiation rounds required by the
FCAN are lower than that of the Time model, and
the combined ASV obtained are higher than that of
the Time model. Figures 4-5 also show that when
the number of issues increases, FCAN and Time
usually need more negotiation rounds, but the
combined ASV may decrease. This corresponds to a
common phenomenon: when negotiation issues
increase, negotiators need more rounds to explore
and reach an agreement, and the final combined
ASV does not necessarily increase.
Figure 4: Average negotiation rounds of agents with
different issues [deadline = 15].
Figure 5: Average combined ASV of agents with different
issues [deadline = 15].
As can be seen from Figures 6-7, when the
negotiation is subject to the deadline constraints
between 10 and 30 and is not affected by the number
of negotiation issues, the number of rounds of the
FACN model is usually lower than that of the Time
model and the combined ASV is usually higher than
that of the Time model. When the deadline is
relaxed, the FCAN and Time can usually obtain a
higher combined ASV after more rounds for
negotiation. In addition, due to deadlines constraints,
the combined ASV obtained by the FCAN and Time
is close, but the number of negotiation rounds
required shows a great difference. This corresponds
to the common phenomenon that when agents
negotiate purely based on time, they need more
rounds to reach a satisfactory agreement.
Figure 6: Average negotiation rounds of agents with
different deadlines [the number of issues = 5].
Figure 7: Average combined ASV of agents with different
deadlines [the number of issues = 5].
In conclusion, when agents are eager to reach an
agreement, whether they are under the pressure of
deadlines or issues, the FCAN model performs
better than the Time model because compared to the
Time model, FCAN can obtain higher combined
ASV in fewer negotiation rounds. This satisfies the
general goal of automatic negotiation, that is, to
obtain a higher combined ASV in fewer rounds.
Therefore, the above experimental results fully
validate the feasibility and effectiveness of our
negotiation model.
5 CONCLUSIONS
A general framework and an open simulation
platform for the fuzzy constraint-based agent
Modeling Doctor-patient Shared Decision-making as Fuzzy Constraint-based Agent Negotiation
53

negotiation of SDM are presented in this paper.
Based on fuzzy constraints, we intuitively and
effectively transformed SDMP into DFCSP. Then,
in the Negotiation Module, the DA and PA were
designed to simulate the negotiation between doctors
and patients. After that, the Recommendation
Module converted the negotiation results into
treatment plans. Finally, the Reporting Module
provides a detailed report of negotiations and
recommendations to doctors and patients.
Experimental results demonstrate that our
proposed method can successfully implement the
negotiation and recommendation of SDM based on
fuzzy constraints and obtain higher combined ASV
in fewer rounds. Specifically, the presented method
effectively alleviates the constraints of issues and
time on negotiation and significantly improves
negotiation efficiency. Although our method has
received some feasible and effective results, further
exploration is needed, such as the learning
capabilities and convergence analysis and the
negotiation of our proposed method in more
complex scenarios.
ACKNOWLEDGEMENTS
This research was funded by the Science Foundation
of Fujian Province (No. 2021J011188), the Xiamen
Science and Technology Planning Project (No.
3502Z20206073), the Research Project of Xiamen
Overseas Students (No. XRS202017206), and the
Scientific Research Project of Xiamen University of
Technology (No. YKJCX2019108).
REFERENCES
ATEIB, M. T. 2010. Agent based negotiation in e-
commerce. 2010 International Symposium on
Information Technology. Kuala Lumpur, Malaysia:
IEEE.
BARR, P. J., THOMPSON, R., WALSH, T., GRANDE,
S. W. & ELWYN, G. (2014). The psychometric
properties of collaboRATE: A fast and frugal patient-
peported measure of the shared decision-making
process. J. Journal of Medical Internet Research. 16,
e2.
ELWYN, G., TSULUKIDZE, M., EDWARDS, A.,
LéGARé, F. & NEWCOMBE, R. (2013). Using a
'talk' model of shared decision making to propose an
observation-based measure: Observer OPTION 5
Item. J. Patient Education and Counseling. 93, 265-
271.
FARATIN, P., SIERRA, C. & JENNINGS, N. R. (1998).
Negotiation decision functions for autonomous agents.
J. Robotics and Autonomous Systems. 24, 159-182.
HOFFMANN, T. C., MONTORI, V. M. & MAR, C. D.
(2014). The connection between evidence-based
medicine and shared decision making. J. The Journal
of the American Medical Association. 312, 1295-6.
HOLMES-ROVNER, M. (2007). International patient
decision aid standards (IPDAS): Beyond decision aids
to usual design of patient education materials. J.
Health Expectations. 10, 103-107.
MAKOUL, G. & CLAYMAN, M. L. (2006). An
integrative model of shared decision making in
medical encounters. J. Patient Education and
Counseling. 60, 301-312.
O'CONNOR, A. (2000). Using patient decision aids to
promote evidence-based decision making. J. Acp
Journal Club. 135, A11-2.
PIETERSE, A. H., STIGGELBOUT, A. M. &
MONTORI, V. M. (2019). Shared decision making
and the importance of time. J. The Journal of the
American Medical Association.
POPRZECZNY, A. J., STOCKING, K., SHOWELL, M.
& DUFFY, J. (2020). Patient decision aids to facilitate
shared decision making in obstetrics and gynecology:
A systematic review and meta-analysis. J. Obstetrics
& Gynecology. 135.
REIMANN, H. (1968). Shared decision making and
shared responsibility-a problem of modern educational
establishments. J. Die Agnes Karll-schwester, der
Krankenpfleger. 22, 102-103.
RIVERA-SPOLJARIC, K., HALLEY, M. & WILSON, S.
R. (2014). Shared clinician-patient decision-making
about treatment of pediatric asthma: What do we know
and how can we use it? J. Current Opinion in Allergy
and Clinical Immunology. 14.
SCHOLL, I., KRISTON, L., DIRMAIER, J. R.,
BUCHHOLZ, A. & HäRTER, M. (2012).
Development and psychometric properties of the
shared decision making questionnaire--physician
version (SDM-Q-Doc). J. Patient Education and
Counseling
. 88, 284-290.
SHOJAIEMEHR, B., RAHMANI, A. M. & QADER, N.
N. (2019). A three-phase process for SLA negotiation
of composite cloud services. J. Computer Standards &
Interfaces. 64.
STATES, U. (1982). Making health care decisions: a
report on the ethical and legal implications of
informed consent in the patient-practitioner
relationship; volume one, report. J. Psychiatric
Services. 34, 465.
STIGGELBOUT, A. M., PIETERSE, A. H. & DE HAES,
J. C. (2015). Shared decision making: concepts,
evidence, and practice. J. Patient Education and
Counseling. 98, 1172-1179.
THE RESPIRATORY GROUP, T. S. O. P., CHINESE
MEDICAL ASSOCIATION (2016). Guidelines for
diagnosis, prevention and treatment of bronchial
asthma in children (2016 Edition). J. Chinese Journal
of Pediatrics. 15.
ICHIH 2022 - International Conference on Health Big Data and Intelligent Healthcare
54

VEATCH, R. M. (1972). Models for ethical medicine in a
revolutionary age. What physician-patient roles foster
the most ethical realtionship? J. Hastings Center
Report. 2, 5.
VOOS, H. 2006. Agent-based distributed resource
allocation in technical dynamic systems. IEEE
Workshop on Distributed Intelligent Systems:
Collective Intelligence and Its Applications (DIS'06).
Prague, Czech Republic: IEEE.
WESTON, W. W. (2001). Informed and shared decision-
making: the crux of patient-centred care. J. Canadian
Medical Association Journal. 165, 438-439.
WOOLDRIDGE, M. & JENNINGS, N. R. (1995).
Intelligent agents: theory and practice. J. Knowledge
Engineering Review. 10, 115-152.
Modeling Doctor-patient Shared Decision-making as Fuzzy Constraint-based Agent Negotiation
55
