
Research Progress on Air-liquid Interface Activity and Function in
Respiratory Tract and Digestive Tract
Xinghui Wu
1,2 a
, Mingjie Xia
1,2
, Shufang Cao
1,2
, Wenqi Cai
1,2
, Li Li
1,2
and Lina Yang
1,2,*
1
College of Food Science and Engineering, Bohai University, 121013, Jinzhou, Liaoning, China
2
Grain and Cereal Food Bio-efficient Transformation Engineering Research Center of Liaoning Province, 121013,
Jinzhou, Liaoning, China
*Corresponding author
Keywords: Air-Liquid Interface, Interfacial Activity, Functional Food.
Abstract: Air-liquid interface activity is closely related to the health of the body. The change of interfacial activity
affects the normal physiological functions, such as the internal environment, microecological balance and
nutrient absorption and utilization of the body. In order to provide a new idea for the evaluation and pre-
treatment of respiratory and digestive diseases, and provide theoretical support for the development of
functional food. The formation mechanism of gas-liquid interface is introduced, the relationship between gas-
liquid interface activity and respiratory tract and digestive tract is combed, and the factors affecting the
interface activity are summarized.
1 INTRODUCTION
The air-liquid exchange interface in the body has a
significant impact on the normal physiological
function of organs. In the unhealthy state, the activity
of the air-liquid interface will change accordingly.
The occurrence of respiratory diseases such as
asthma, bronchitis, chronic obstructive pulmonary
disease, oral, gastric and inflammatory bowel
diseases goes hand in hand with the change of air-
liquid interface activity. Asthma and other airway
inflammatory diseases are accompanied by a
significant increase in airway mucus viscoelasticity
(Johnson 2011). In the lungs of patients with
respiratory distress syndrome, protein rich pulmonary
edema can inhibit or destroy the habitual function of
surfactants, resulting in increased surface tension of
pulmonary fluid (Luo et al. 2017). Inflammatory
bowel disease is accompanied by lipid peroxidation
and decreased antioxidant capacity, resulting in an
imbalance between oxidation and antioxidant,
increasing surface pressure. The increase of surface
pressure causes damage to small intestinal mucosa
(Xie & Wan 2020).
a
https://orcid.org/0000-0001-8481-667X
Although more and more studies have found that the
air-liquid interface plays a key role in the occurrence
and prevention of diseases, the causal relationship
between the activity of the air-liquid interface and the
occurrence of diseases and the related molecular
mechanism is not clear. This review expounds and
summarizes the formation of air-liquid interface, the
application of air-liquid interface activity in the health
evaluation of respiratory system and digestive
system, and the factors affecting interface activity. In
order to provide a unique perspective for the
prevention and treatment of related diseases, and
provide a theoretical reference for the design and
production of functional foods for the treatment and
prevention of related diseases.
2 FORMATION OF GAS-LIQUID
INTERFACE
The surface of the oral cavity, airway, stomach,
intestine and other organs of the organism is covered
with a thickness of 2-10 μM mucus layer (Puchelle et
al. 1987), which is the first line of defense of human
immune system (Bajka et al. 2015). It plays a role in
124
Wu, X., Xia, M., Cao, S., Cai, W., Li, L. and Yang, L.
Research Progress on Air-liquid Interface Activity and Function in Respiratory Tract and Digestive Tract.
DOI: 10.5220/0011233200003438
In Proceedings of the 1st International Conference on Health Big Data and Intelligent Healthcare (ICHIH 2022), pages 124-130
ISBN: 978-989-758-596-8
Copyright
c
2022 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved

resisting the invasion of bacteria, viruses and harmful
compounds. Mucus is a gelatinous polymer
composed of glycosylated mucin, containing 90%-
95% of water, 1%-2% lipids and electrolytes (Paola
2020, Widdicombe & Wine 2015). Therefore, mucus
has complex rheological properties, such as shear
thinning, viscoelasticity, adhesion (Puchelle et al.
1987). The exertion of various physiological
functions of the body largely depends on the
appropriate rheological properties of mucus. In the
respiratory system, the protective and scavenging
function of airway mucus is dependent on the
appropriate rheological properties of mucus,
otherwise airway mucus may become a factor of
airway obstruction. For example, the airway of
asthmatic patients will over secrete mucus with high
viscosity, resulting in poor fluidity of mucus and
difficult to discharge from the airway. In severe cases,
airway mucus embolism will be formed in the airway
(Johnson 2011), resulting in atelectasis, asphyxia,
respiratory failure and even sudden death (Luo et al.
2017). In the digestive system, human digestive tract
mucus plays an important role in the digestion and
transportation of food in the gastrointestinal tract and
the lubrication and protection of gastrointestinal
mucosal surface (Zhou et al. 2004). Moreover,
intestinal fluid rheology is also closely related to the
colonization, distribution and growth of intestinal
flora, and then affects the absorption effect of
nutrients and drugs (Boegh et al. 2014).
There is a surface layer of the contact between the
mucus layer and the external atmospheric
environment, referred to as the air-liquid interface.
The surface response of air-liquid interface to
dynamic conditions is closely linked to the stability
and health of various tissues and organs. In the
development of natural science and light industry, the
application of air-liquid interface activity has been
widespread. For example, the production principle of
Yuba is to denature the protein in soybean milk by
heating. The hydrophobic groups inside the protein
are exposed, while the hydrophilic groups outside the
protein are transferred to the inside of the molecule.
The protein is concentrated, collided and condense,
precipitate, and gradually grow into a film. Then, the
sugar is adsorbed on the protein by van der Waals
force or hydrogen bond to gradually form a certain
toughness of Yuba (Chen 2010). However, there is
little understanding of how the air-liquid interface in
a human body affects the normal physiological
function of various tissues and organs. The main
reason is that the structure of the human body is much
more complex than that of other organisms. And it
belongs to soft matter from the perspective of
materials, which are essentially different from
inorganic materials (Jin 2014). Therefore, it’s great
significance for understanding the mechanism of
physiological activities and disease occurrence and
development to study the air-liquid interface with
special functions in the human body at the micro
scale.
3 ACTIVITY AND FUNCTION OF
AIR-LIQUID INTERFACE IN
RESPIRATORY TRACT
3.1 Nose
The surface of nasal mucosa is the subject with a
mucus blanket with a thickness of 5-10 μm. It can
adsorb about 80% of the particles in the gas, and the
mass of these particles is greater than 12.5 μg (Zhang
et al. 2006). Mucociliary blanket and ciliated
epithelial layer below it constitute nasal mucociliary
transmission system, which is an important
mechanical defense system of human body. Guo
Yongqing (Guo et al. 2004) tried to construct a
Construction of ciliary differentiation model of
cultured human nasal epithelial by using air-liquid
interface culture technology, and quantitatively
analyzed the degree of ciliary differentiation. The
research provide an advanced research means for
exploring the physiological and pathological
characteristics of respiratory epithelial cells. Zhao
Yanyan (Zhao et al. 2020) infected human nasal
epithelial cells cultured at the air-liquid interface with
Staphylococcus aureus standard strains and clinical
isolates of chronic rhinosinusitis, and analyzed the
effects of Staphylococcus aureus infection on the
tight junction and cell viability of nasal epithelial
cells.
3.2 Hung
The human airway is covered by mucus layer. The
changes of rheological properties such as mucus
viscosity and surface tension affect the physiological
functions such as airway stability, lung defense
barrier and mucociliary clearance. Long Yun (Long
et al. 2006) and others think that the collapse of
airway compliance largely depends on the pressure
load of surface tension on airway wall. Due to the
compression of the airway, the increase of the
curvature of the air-liquid interface will increase the
surface tension, resulting in the increase of the load
on the airway wall, and finally affect the compliance
Research Progress on Air-liquid Interface Activity and Function in Respiratory Tract and Digestive Tract
125

of the airway wall. Pulmonary surfactant (PS) is a
lipid complex protein mixture. It covers the alveolar
surface and makes the respiratory function normal by
reducing the surface tension at the air-liquid interface
(Wang&Hu 2020). At the same time, it also has the
functions of stabilizing the airway and protecting
against the pulmonary edema (Liu et al. 2020). Ann
M. czyzewski (Czyzewski et al. 2018) et al. used
biomimetic lipid mixture to simulate the
physiological activity of pulmonary surfactant
proteins B and C at the air-liquid interface. The study
provides a strong theoretical basis for the new
medical research that natural surfactants can
effectively treat acute lung injury. Ji Xiaoli (Ji et al.
2021) constructed a primary culture model of mouse
tracheal epithelial cells by air-liquid interface culture.
It was applied to the evaluation of the inhalation
toxicological in vitro.
4 ACTIVITY AND FUNCTION OF
AIR-LIQUID INTERFACE IN
DIGESTIVE TRACT
4.1 Oral Cavity
Human saliva is mainly produced in the oral cavity by
the parotid gland, submersible gland and the
sublingual gland. It is a major biological liquid to
maintain oral health. Saliva not only serves as a
barrier to pathogens, but also promotes food intake. It
also provides a medium for dissolved and suspended
food substances to stimulate the taste. As the core
component of salivary membrane covering teeth,
mucin plays a role in helping lubricate, protect and
heal oral mucosa (Liu 2018). Rossetti (Rossetti et al.
2013, Rossetti et al. 2013) examined the effect of the
interaction between proteins of human oral saliva and
different polyphenols on the expansion
characteristics of air-liquid interface during oral
digestion. Firstly, the complexity of kinetics and
interfacial expansion rheology of salivary membrane
was investigated. The results showed that small
molecular weight protein components adsorbed on
the interface and produced solute like surfactant
reaction, but the adsorption of higher molecular
weight proteins makes the interface more and more
insoluble.
4.2 Stomach
There are many kinds of internal and external
secretory cells in gastric mucosa, such as principal
cells, parietal cells and G cells. Its synthetic and
released gastric juice and various gastrointestinal
hormones are widely involved in digestion and
absorption (Liu et al. 2020). Mucosa can protect the
stomach from gastric acid erosion. Once damaged,
the stomach will be invaded by gastric acid and
bacteria for a long time. In severe cases, it will be
expected to result in gastric ulcer, gastric perforation
and other diseases (Jin 2014). Helicobacter pylori
infection will destroy the structure and function of
gastric mucosal epithelium. Jin Lin (Jin 2014)
explored the mechanism of Helicobacter pylori
infection of gastric mucosal epithelium by
establishing H. pylori gastric mucosal epithelial air-
liquid interface. The study provides a theoretical basis
for the prevention and treatment of gastrointestinal
diseases caused by infection.
4.3 Intestine
In the intestine, the small intestine is the main port for
nutrient absorption. The lumen surface is composed
of intestinal epithelial cells and covered by a mucus
layer, which is a barrier against harsh digestive
environment (Huang 2021, Ou et al. 2021). Many
microbiota are colonized on the surface of intestinal
mucosa, which coexist with the human body and
maintains the normal physiological function of the
host. Once the flora structure is changed, the
proportion of bacteria is unbalanced, and the
metabolism will be disorder. It may lead to the
occurrence of various diseases such as diabetes
mellitus (Yao 2020). Studies have shown that
changes in duodenal fluid rheology usually affect the
colonization, distribution and growth of intestinal
flora, and then affect the absorption effect of nutrients
and drugs (Morrison & Preston 2016). Johansson
(Johansson et al. 2015) et al. further found that the
number of goblet cells in the intestinal mucus of green
fluorescent mice was depressed, and the intestinal
mucus was anchored on the goblet cells and could not
be sucked out through the experiment. Compared
with conventional mice, green fluorescent mice have
poor intestinal mucus rheology and reduced air-liquid
interface activity. It makes intestinal flora colonize
difficultly, and then affecting the distribution and
growth of intestinal flora. TARGO (Tamargo et al.
2018) also show that the increase of colonic mucus
viscosity is conducive to the reproduction of
anaerobic bacteria, and the reproduction of the
intestinal flora will also increase the viscosity of the
culture system. The changes in the composition of
intestinal flora also reduce the thickness of the
intestinal mucus layer and increase mucus
ICHIH 2022 - International Conference on Health Big Data and Intelligent Healthcare
126
permeability (Wells et al. 2017). Some intestinal
probiotics have been proved to regulate intestinal
epithelial function by promoting the formation of
mucosal layer, secreting antibacterial factors,
promoting the secretion of secretory immunoglobulin
A and competitive adhesion with intestinal epithelial
cells (Liu et al. 2020), and reduce surface tension and
increase expansion modulus to maintain intestinal
barrier homeostasis and promote health.
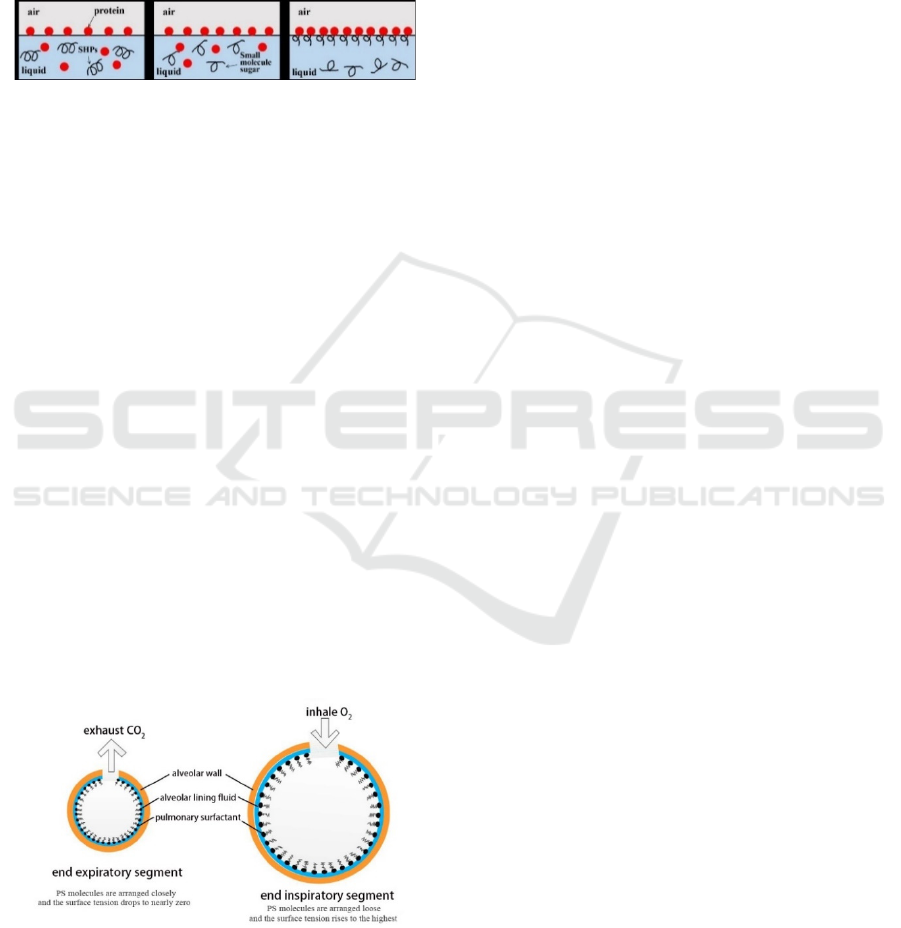
Figure 1: Model of soy hull polysaccharides-protein in
simulated intestinal fluid (Huang 2020).
5 IMPACT FACTORS OF THE
ACTIVITY OF AIR-LIQUID
INTERFACE
5.1 Effect of Surfactant on
Interfacial Activity
Surfactant plays a decisive role in regulating the
viscosity of mucus and the rheological properties of
air-liquid interface. As shown in Figure 2, natural PS
provides surface activity of alveoli during respiration.
During inhalation, PS forms a surface active
membrane which adsorbs to the air-liquid interface to
cover the alveolar area. When exhaling, PS forms a
compressible multilayer structure. The surfactant film
is filled with PS that greatly reduces the alveolar
surface tension. When the alveolar dilation is caused
by re inhalation, the surfactant membrane expands
again. And the phospholipids at the air-liquid
interface redistribute laterally to cover the alveolar
area.
Figure 2: Schematic diagram of alveolar structure and
function (Dong et al. 2016).
Studies have shown that there is a substance
similar to PS in the eustachian tube, mainly composed
of phosphatidylcholine and protein. It can reduce the
surface tension of the ciliated mucus blanket on the
surface of the eustachian tube, and prevent the
adhesion of the tube wall and contribute to the
discharge of secretions. The reduction of surfactant is
not conducive to the opening of the eustachian tube
and the discharge of secretions (Zhu et al. 2013).
Fornadley (Dong et al. 2016) et al. found that by
injecting exogenous surfactant, the open pressure of
eustachian tube in gerbils with secretory otitis media
model decreased significantly and closed to the
normal value.
Due to the electrostatic attraction of opposite
charges, intestinal mucin can combine with some
lipids or polysaccharides to form surfactant. It can
change the activity of air-liquid interface. Luo
Xinyou (Luo et al. 2015) et al. treated sinusitis of
children with a composite surfactant composed of
soybean based grain extract and cationic surfactant
(chitosan quaternary ammonium salt). Through the
inhibitory effect of Chitosan on the biological
interface of Streptococcus mutants and the reduction
of toxicity and enhancement of bactericidal effect of
grain extract, the nasal ventilation and sinus drainage
are improved. Guri (Guri et al. 2015) et al. used
epithelial mucus extracted from human colon
adenocarcinoma cell HT29-MTX to explore the
interaction between tea polyphenols and milk protein
and intestinal mucus at the air-liquid interface. It is
found that the main component of tea polyphenols
(epigallocatechin-3-gallate) can bind to milk protein.
The formed complex reduces the interfacial surface
tension and increases the expansion modulus. It
indicate that nutrient molecules are more likely to
interact with intestinal mucus before they are
effectively transported and absorbed by intestinal
cells. The research of Huang Jinghang (Huang et al.
2020) shows that soybean hull polysaccharide may
form a similar polysaccharide mucin complex in the
intestinal digestion in the delivery system. Therefore,
in the process of interfacial adsorption, the interfacial
tension decreases and the interfacial expansion
modulus increases are conducive to the release and
absorption of nutrients. The study provides
theoretical support for the development of beneficial
functional foods of soy hull polysaccharide.
5.2 Effect of pH on Interfacial
Activity
A large number of experiments have proved that the
change of pH value will affect the activity of air-
liquid interface. By studying the film-forming law of
protein at the air-liquid interface, Hua Jian (Hua
Research Progress on Air-liquid Interface Activity and Function in Respiratory Tract and Digestive Tract
127

2003) found that the surface pressure will gradually
increase with the increase of pH value. And at
isoelectric point nearly, the both of the interface
activity and the ability to reduce surface tension are
also inferior, and the surface pressure is small. This
may be because the change of pH of the system will
lead to the change of charge, which will affect its
stability. Dong Lei (Dong et al. 2014) et al. found that
the change of charge density can inhibit the formation
of a tight adsorption layer at the air-liquid interface of
protein molecules and the increase of surface pressure
and expansion modulus. In addition, the change of pH
value of mucus will also affect the viscosity of mucus,
and then change the activity of air-liquid interface.
For example, some people believe that Helicobacter
pylori will not only increase the pH value of mucus,
but also reduce the viscoelasticity of mucus and
increase the mobility of mucus. It also can reduce the
activity of the air-liquid interface.
5.3 Effect of Ions on Interfacial
Activity
Ionic strength affects the adsorption kinetics of
particles at the air-liquid interface, and then affects
the interfacial activity. Wang Mei (Wang et al. 2020)
et al. analyzed the change of air-liquid interface
pressure under the strength of Na
+
and Ca
2+
at pH 7.
They found that the greater the ionic strength, the
faster the surface pressure rises. This may be because
ions make the protein molecular structure more loose
and it is easier to adsorb to the air-liquid interface,
leading to the interfacial tension and increasing the
surface pressure. Moreover, the increase of ionic
strength will also enhance the flexibility of protein.
The hydrophobic groups of protein molecules are
more likely to be exposed to the air-liquid interface,
it can reduces the tension of the air-liquid interface
and accelerates the rate of expansion and
rearrangement. Zhang Xuan (Zhang et al. 2020) et al.
found that the surface tension equilibrium value
decreased with the increase of Ca
2+
and Na
+
content.
It is mainly caused by the increase of adsorption
capacity of nanoparticles at the air-liquid interface. At
the air-liquid interface, the electrostatic repulsion
between particles is inversely proportional to the salt
content. Meanwhile, the negative repulsion between
particles and air-liquid interface will also decrease
with the increase of salt content, resulting in the
increase of particle adsorption density at the interface.
In addition, studies have shown that the contact angle
of particles will increase with the increase of ion
content (Wang et al. 2021), it makes the surface
tension decrease more obviously.
5.4 Effect of Antioxidants on
Interfacial Activity
At present, it has been found that a variety of
experimental intestinal mucosal injury and intestinal
diseases are related to the participation of aerobic free
radicals (Qian, et al. 2017). Lipid peroxidation and
the decrease of antioxidant capacity lead to the
imbalance between oxidation and antioxidant, the
increase of surface pressure and the damage of small
intestinal mucosa. Antioxidants can protect the
function of intestinal mucosal barrier by increasing
the activity of intestinal antioxidant enzymes,
scavenging oxygen free radicals, improving the state
of oxidative stress, improving tissue antioxidant
capacity and changing the activity of air-liquid
interface.
6 CONCLUSIONS
In recent years, with the development of science and
technology, air-liquid interfacial activity has long
been not only used to explain natural science and
applied in food industry, industry, manufacturing and
other production and processing. In terms of body
health evaluation, the air-liquid interface also plays
an important role. Although there are a few reports on
the formation of air-liquid interface, the function of
air-liquid interface activity in digestive tract and
respiratory tract and the factors affecting interface
activity, there are still many outstanding problems.
For example, the mechanism of air-liquid interface
activity regulating body health and the influence
mechanism of surfactant on interface activity are not
clear. However, based on the available information of
air-liquid interface activity, it can be determined that
air-liquid interface activity affects physiological
functions such as environmental stability of tissues
and organs, microecological balance and nutrient
absorption and utilization. It is hoped that with the
gradual deepening of people's research, the air-liquid
interface activity will provide unlimited possibilities
for the treatment of related diseases. And the idea that
the activity of air-liquid interface in vivo can be
adjusted by oral administration of exogenous
surfactants can be realized as soon as possible. At the
same time, the study of air-liquid interface also
provides multi angle demonstration for the functional
food to be developed.
ICHIH 2022 - International Conference on Health Big Data and Intelligent Healthcare
128

ACKNOWLEDGEMENTS
This study was supported by National Natural
Science Foundation of China (Grant No. 31901680).
REFERENCES
Ahluwalia, B. Moraes, L. Magnusson, M.K. (2018).
Immunopathogenesis of inflammatory bowel disease
and mechanisms of biological therapies. J. Scand J
Gastroenterol. 53(4):379-389
Bajka, B.H. Rigby, N.M. Cross, K.L. (2015). The influence
of small intestinal mucus structure on particle transport
ex vivo. J. Colloid Surface B. 135:73-80.
Boegh, M. Baldursdóttir, S.G. Müllertz, A.(2014). Property
profiling of biosimilar mucus in a novel mucus-
containing in vitro model for assessment of intestinal
drug absorption. J. Eur J Pharm Biopharm. 87(2): 227-
235.
Chen, Y.M.& One, T. (2010). The mechanisms for yuba
formation and its stable lipid. J. J Agr Food Chem.
58(10):6485-6489.
Czyzewski, A.M. Mccaig, L.M. Dohm, M.T.(2018).
Effective in vivo treatment of acute lung injury with
helical, amphipathic peptoid mimics of pulmonary
surfactant proteins. J. Sci Rep-UK. 8(1):6795.
Dong, C.G. Li, L. Liu, Z.L. (2016). Detection of eustachian
tube and nasopharynx surfactant in children with
secretory otitis media. J. Journal of Audiology and
speech diseases. 24(01):93-94.
Dong, L. Liu, T.J. Kong, L.S. (2014). Research Progress
on the interaction between protein and polysaccharide
at the interface. J. Science and technology of food
industry. 35(23):397-400.
Guri, A. Li, Y. Corredig. M. (2015). Interfacial dilational
properties of tea polyphenols and milk proteins with gut
epithelia and the role of mucus in nutrient adsorption. J.
Food Funct. 6(12): 3642-3651.
Guo, Y.Q. Zhao, X.D. Yang, Z.Q.(2004). Ciliary
differentiation of nasal mucosal epithelial cells cultured
at gas-liquid interface. J. Clin Otolaryngol. (02):88-90.
Hua, J. (2003). Physicochemical properties of protein at gas
/ water interface and monolayer formation. D. Sichuan
University
Huang, J.H. (2020). Study on the regulation mechanism of
soybean seed coat polysaccharide on intestinal flora
based on intestinal fluid rheology. D. Bohai University.
Huang, J.H. Yang, L.N. Zhao, Y.F.(2020). Effects of
soybean seed coat polysaccharide on rheological
properties of simulated intestinal fluid and intestinal
flora. J. Chinese Journal of food. 20(12):48-55.
Huang, Y.K.(2021). Effects of gastrointestinal mucosal
barrier dysfunction and intestinal bacterial or endotoxin
translocation on the body. J. Journal of Clinical
Pediatrics, (10):908-911.
Jin, L.J.(2014).“Study on the adhesion behavior of
Helicobacter pylori gastric mucosal epithelium
biological interface. D. Southern Medical University.
Ji, X.L. Hu, Y. Sheng, Y.H.( 2021). Construction of mouse
tracheal epithelial cell model cultured at gas-liquid
interface. J. Chinese pharmacology bulletin, (02):282-
288.
Johansson, M. Jakobsson, H. Holmén-Larsson, J. (2015).
Normalization of host intestinal mucus layers requires
long- term microbial colonization. J. Cell Host
Microbe. 18:582-592.
Liu, D.W. (2018). Effect of citric acid on the structure and
lubrication of salivary protein adsorption membrane. D.
Southwest Jiaotong University.
Liu, L.S. Liu, W.J. Xu, X.Z. (2020). Study on the
expression of mitochondrial autophagy related proteins
in gastric mucosal cells of spleen qi deficiency rats. J.
World science and technology - modernization of
traditional Chinese medicine. 22(09):3089-3093.
Liu, Q. Yu, Z. Tian, F. (2020). Surface components and
metabolites of probiotics for regulation of intestinal
epithelial barrier. J. Microb Cell Fact. 19(1):23.
Liu, Y.Y. Chen, Z.L. Song, Y.L. (2020). Clinical
significance and measurement methods of pulmonary
fluid viscosity and surface tension. J. Medical
biomechanics, 35(03):378-384.
Luo, X.Y. Li, Y. Zhao, S.J. (2015). Effect of grain extract
and cationic surfactant on sinusitis in children. J.
Chinese medical engineering. 23(02):107-110.
Long, Y. Liu, D.W. Jin, Y.Z.(2006). Application of static
pressure volume curve in pulmonary recruitment and
collapse in acute respiratory distress syndrome. J.
Chinese Journal of tuberculosis and respiration, (07):
452-457.
Luo, M.Z. Wang, J.L. Zhang, Q. (2017). Study on
rheological properties and influencing factors of airway
mucus in asthma. C. Chinese society of mechanics,
Beijing University of technology.1218-1225.
Morrison, D.J. Preston, T. (2016). Formation of short chain
fatty acids by the gut microbiota and their impact on
human metabolism. J. Gut microbes. 7(3): 189-200.
Ou, Y.J. Li, X.P. Zhou, F.( 2021). Effects of pingyanghuang
Decoction on intestinal barrier and intestinal flora in
rats fed with high-fat diet. J. Food science, 1-12.
Paola, P. Patrice, D.C. (2020). Mucus barrier, mucins and
gut microbiota: the expected slimy partners? J.
Gut.69(12):2232-2243.
Puchelle, E. Zahm, JM. Quemada, D. (1987).
Rheologicalproperties controlling mucociliary
frequency and respiratory mucus transport. J.
Biorheology. 24(6):557-563.
Qian, X. Li, Q. (2017). Phosphoglycerate Kinase 1
Phosphorylates Beclin1 to induce autophagy. J.
Molecular Cell.65(5):917-931.
Rossetti, D. Ravera, F. Liggieri, L. (2013). Effect of tea
polyphenols on the dilational rheology of human whole
saliva (HWS): Part 1, HWS characterization. J. Colloid
Surface B. 110: 466-473.
Ruan, D. Wang, Y.B. Jiang, S.Q. (2021). Biological activity
of curcumin and its molecular mechanism of regulating
Research Progress on Air-liquid Interface Activity and Function in Respiratory Tract and Digestive Tract
129

intestinal mucosal barrier function in animals. J. J Anim
Physiol An N. 1-10.
Tamargo, A. Cueva, C. Alvarez, M.D.(2018). Influence of
viscosity on the growth of human gut microbiota. J.
Food Hydrocoll. 77: 163-167.
Wang, L.F. Hu. X.F. (2020). Pulmonary surfactant and
related respiratory diseases. J. Chinese Journal of cell
biology. 42(04):721-728.
Wang, M. Yao, Y.J. Liu, K.L.(2020). Effect of ionic
strength on the gas-liquid interfacial behavior and foam
characteristics of rapeseed protein isolate. J. China
Journal of cereals and oils.1-7.
Wang, Z.L. Long, Y. Li, C.W.(2021). Role of intestinal
flora in Chinese herbal medicine against ulcerative
colitis. J. Journal of pharmacy.1-27.
Wells, J.M. Brummer, R.J. Derrien, M.(2017).
Homeostasis of the gut barrier and potential
biomarkers. J. Am J Physiol Gastrointest Liver
Physiol.312:G171-193.
Widdicombe, J.H. Wine J.J. (2015). Airway gland structure
and function. J. Physiol Rev. 95(4):1241-1319.
Xie, J.H. NIE, S.P. Ding, Q. (2015). Effect of carrot pulp
fermented by Lactobacillus plantarum ncu116 on
intestinal mucosal immunity in immunosuppressive
mice. J. Food science. 36(21):201-206.
Xie, L. Wan, H. (2020). Research progress on relationship
between gut microbiota and development of breast
cancer and mechanism. J. China Academic Journal
Electronic Publishing House. 28(21):3806-3810.
Yao, B.Y. (2020). Effect of lithocholic acid on intestinal
mucosal barrier function and its mechanism. D. China
Medical University.
Zhang, L. Han, D.M. Wang, Q. (2006). Evaluation of nasal
mucociliary transport system function. J. Chinese
otolaryngology head and neck surgery.13(7):507-510
.
Zhang, X. Zhang, T.C. (2020). Effect of surfactants on
adsorption law of nanoparticles at gas-liquid interface.
J. Journal of physics. 69(02):217-224.
Zhao, Q. (2019). Study on interfacial chemistry between
atmospheric fine particles and pulmonary surfactant. D.
Kunming University of technology.
Zhao, Y.Y. Wang, S. Zhang, J. HU. H. (2020). Effects of
Staphylococcus aureus infection on tight junctions and
cell viability of nasal mucosal epithelial cells cultured
at gas-liquid interface. J. Chinese otolaryngology head
and neck surgery. 27(08):469-472.
Zhou, D.H. Li, J.S. Li, N. Yan, G.Z. (2004). Study on
rheological properties of human digestive tract mucus.
J. Journal of biomedical engineering. (01):72-73.
Zhu, Z.H. Shan, Y.J. Han, Y.(2013). Pathological study of
otitismedia with effusion after treatment with intranasal
pulmonary surfactant. J. Laryngoscope, 123:3148.
ICHIH 2022 - International Conference on Health Big Data and Intelligent Healthcare
130
