
Juvenile Asthma in the U.S. Relate Asthma Incidence to Body Mass
Index
Linshuo Yang
1
, Zhijie Duan
2
and Jingchen Chai
3*
1
McMaster University, Canada
2
University of North Carolina at Chapel Hill, U.S.A
3
University of Alberta, Canada
Keywords: BMI, Asthma, Adolescent, Sex, Ethnicity, NHANES.
Abstract: Asthma is one of the most common chronic diseases among humans, juveniles. Obesity, as many studies
suggest, is related to the development of asthma. This research study intends to identify the strength of
correlation between BMI and asthma in different gender and ethnic groups and explore whether the incidence
of asthma increases with higher BMI. Here, researchers first divided the data collected from the National
Health and Nutrition Examination Survey into two groups by the variable _Have_Asthma_. T-tests for the
difference in means were then employed to show that the average BMIs for the two groups differ in a
statistically significant way. Quantile analyses were also used to compare the proportion of people having
asthma in each BMI quantile. To quantify the strength of correlation, a bootstrap confidence interval was built
and logistic regression models for the data from 2015 to 2016, and 2017 to 2018. To avoid the collinearity
between gender and BMI, the researchers also built separate logistic models for each gender. The authors
concluded that juveniles with higher BMI have a higher risk of getting asthma. Male juveniles have an overall
higher risk of getting asthma than female juveniles. Non-Hispanic black juveniles are more likely to have
asthma than Mexican American juveniles and non-Hispanic white juveniles.
1 INTRODUCTION
Asthma, a prevalent and variable disease, can range
in severity from mild, with few obvious symptoms, to
severe, which is characterized by acute or subacute
progressive exacerbations of asthma symptoms
(Lloyd, Price and Brown 2007, Mukherjee et al
2016). There is a large amount of epidemiological
evidence showing that obesity is one of the most
influential factors of asthma (Forno 2020). However,
few studies are targeting specific age groups,
especially juveniles (under 18 years old).
Bidirectional Mendelian randomized studies in
children and adults have shown an association
between genetic risk score for obesity and subsequent
development of asthma, but not between asthma
genes and subsequent obesity (Chen, Fan, Huang,
Liou and Lee 2019, Xu, Gilliland and Conti 2019). In
addition, studies have shown that weight loss can
significantly improve asthma symptoms and lung
function (Okoniewski, Lu and Forno 2019).
Similarly, some studies have found that obese asthma
patients are difficult to manage, with poor lung
function and weak response to asthma medication
(Boulet and Franssen, Dixon, Shade, Cohen et al
2006). As juvenile asthma and obesity are becoming
pressing public health issues around the globe,
investigating the strength of correlation between BMI
and asthma in the under-age population may benefit
the prevention and prognosis of juvenile asthma.
Based on the literature review, researchers in this
study hypothesized that the incidence of asthma
increases with higher BMI among juveniles. T-tests,
quantile analyses, bootstrap confidence intervals, and
logistic regression models were employed to identify
and quantify the correlation between BMI and asthma
incidence among juveniles grouped by different
ethnicities and genders.
2 METHODS
2.1 Data Source and Screening
Our data set was downloaded from the National
Health and Nutrition Examination Survey. The
194
Yang, L., Duan, Z. and Chai, J.
Juvenile Asthma in the U.S. Relate Asthma Incidence to Body Mass Index.
DOI: 10.5220/0011241600003438
In Proceedings of the 1st International Conference on Health Big Data and Intelligent Healthcare (ICHIH 2022), pages 194-199
ISBN: 978-989-758-596-8
Copyright
c
2022 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
researchers merged the 2015-2016 data frame and
2017-2018 data frame, getting a sample size of
19225. Then select all rows that have a value of age
less than 18, yielding a subset that has 7377
individuals. Next, screening the data, excluding
individuals that have a missing value in the columns
of Age, Sex, Ethnicity, Have Asthma, and BMI. The
final complete data frame includes 5666 individuals.
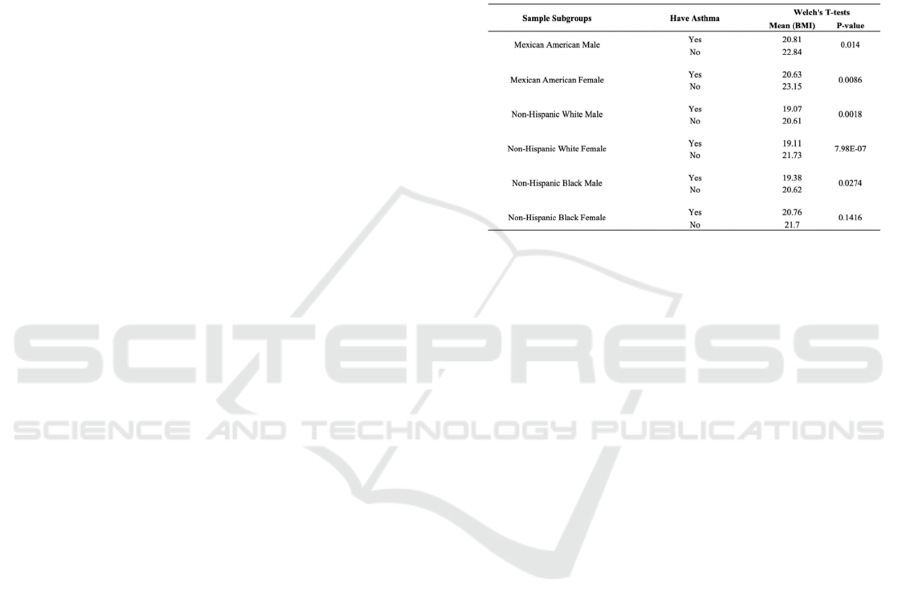
Welch’s T-tests
To avoid ambiguity and ensure enough data, Non-
Hispanic White, Non-Hispanic Black, and Mexican
American ethnicities were selected for further study.
To control variables, the whole data was subsetted
based on _Ethnicity_ (Mexican American, non-
Hispanic whites, and non-Hispanic black) and
_Gender_ (Male and Female). Six subgroups (e.g.
Male+Mexican American) were then obtained. Each
subgroup was further split by the categorical variable
_Have_Asthma_ into two groups, which are the
individuals that have asthma and the individuals that
do not have asthma. Two sample t-tests were then
conducted to compare the average BMI of asthma
patients and people without asthma in each subgroup.
Welch’s t-test was chosen because the two samples
compared have different sample sizes.
2.2 Quantile Analysis
Different from the previous subdivision, this time the
data was subgrouped by each gender and each
ethnicity separately, yielding five subgroups in total,
which were used to conduct quantile analysis. The
sample sizes of the five ethnic groups are 1678(Non-
Hispanic White), 1086(Mexican American),
1312(Non-Hispanic Black), 1000(Other Race), and
589(Other Hispanic). The sample sizes of the two
gender groups are 2842 (male) and 2823(female).
Q1 (First 25%), Q2(First 25%-50%), Q3(50%-75%),
Q4(Last 25%).
2.3 Model Building
A statistical comparison is made between two
classified sets. A preliminary hypothesis was made by
directly comparing the number of people who have
asthma in Q1-Q4. Case resampling will then be
utilized to obtain a 95% bootstrap confidence interval
for the correlation between BMI and asthma. Logistic
regression models were then built to explore the
correlation between asthma and other selected
variables.
3 RESULTS
Welch’s t-test for the Mexican American male group
shows that the average BMIs of people with and
without asthma are 20.81 and 22.84, respectively. The
other t-test for the Mexican American female group
showed that the average BMIs of people with and
without asthma were 20.63 and 23.15, respectively.
The p-values were both less than 0.05, indicating the
differences in means were statistically significant
(Figure 1).
Figure 1: T-test Result for Mexican American Samples.
Welch’s t-test for the non-Hispanic white male
group showed that the average BMIs of people with
and without asthma were 19.06 and 20.61,
respectively. The other t-test for the non-Hispanic
white female group showed that the average BMIs of
people with and without asthma were 19.11 and
21.73, respectively. The p-values were both less than
0.05, indicating the differences in means were
statistically significant.
Welch’s t-test for the non-Hispanic black male
group showed that the average BMIs of people with
and without asthma were 19.38 and 20.62,
respectively. The p-value was less than 0.05,
indicating the difference in means was statistically
significant. The other t-test for the non-Hispanic
black female group showed that the average BMIs of
people with and without asthma were 20.76 and
21.70, respectively. The p-values were greater than
0.05, indicating that the difference in means was not
statistically significant.
The BMI-based distribution quantile analyzed for
each gender group were in Figures 4 and 5. In general,
our male sample had a higher overall asthma
incidence (18.0%) than the female sample (13.5%).
Though the male sample had a higher proportion of
asthma population in all quantiles, there was not
much difference between the two samples in the
fourth quantile (23.7% vs. 21.2%), revealing the fact
that the incidence of asthma was nearly the same for
males and females with high BMI. In short, the
Juvenile Asthma in the U.S. Relate Asthma Incidence to Body Mass Index
195
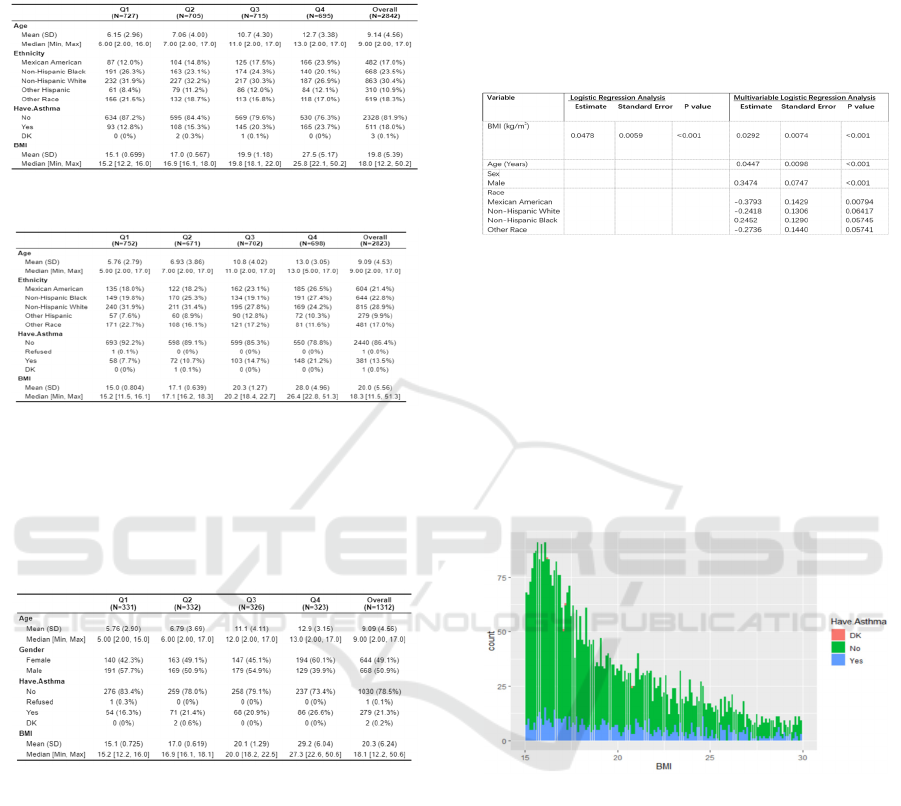
incidence of asthma increased with higher BMI for
both genders, and male juveniles were more likely to
get asthma than female juveniles did (figure 2).
Figure 2: Total Male Samples .
Figure 3: Total Female Samples.
In all four BMI quantiles, the Non-Hispanic Black
sample exhibits a higher asthma incidence rate than
the other two ethnic groups. In the Non-Hispanic
Black sample, all the quantiles except Q1 had an
asthma incidence rate higher than 20% (Figure 3).
Figure 4: Non-Hispanic Black Samples.
The 95% bootstrap confidence interval is
(0.09507, 0.10764), indicating that 95% of the time
the population correlation between BMI and asthma
fell within the range of 0.095 and 0.107. In the
univariable logistic regression model (Figure 4), the
p-value was smaller than 0.05, suggesting that it is
significantly associated with asthma status. In the
multivariable logistic regression model (Figure 5),
variables that were significantly associated with
asthma include sex, age, BMI, and Mexican
American. The rest of the variables had an
insignificant association with asthma. Researchers in
this study found that sex had the lowest p-value,
indicating a strong association between gender and
the probability of having asthma. The positive
coefficient of this predictor suggested that with all
other variables being equal, males were more likely
to have asthma. Being male increased the log odds by
0.3474. The accuracy of this model showed 0.82. The
dataset was then split into two subsets by gender. P-
values in logistic regression models for males and
females, respectively, were both less than 0.05.
Figure 5: Univariable and Multivariable logistic regression
analysis, NHANES, 2015-2016,2017- 2018(5,666)
Figure 6 was created to help explain the results
from the logistic regression. From the graph, it was
obvious to see that people who did not have asthma
were significantly higher than people who have
asthma in the low to medium range of BMI from 15-
25. Although there were fewer data within the range
from 25-30 compared with the range from 15-25, it
was still clear to see that the people with asthma
occupy a larger proportion of the whole.
Figure 6: Distribution of asthma outcomes on the range of
BMI.
4 DISCUSSION
A study shows that treating obese asthma patients has
become a challenge since these patients have worse
lung function and are less responsive to asthma
medications. For these patients, the best and easiest
treatment is to lose weight. Significant weight loss
can improve asthma symptoms, lung function, or the
rate at which asthma worsens (Dhabuwala and
Cannan 2000). It was shown that bariatric surgery had
significant effects on asthma controls, which led to an
approximately 60% reduction in having asthma
ICHIH 2022 - International Conference on Health Big Data and Intelligent Healthcare
196

exacerbation (Peters, Dixon and Forno 2018). Their
research has proved that the incidence of asthma is
highly related to obesity, and losing weight is the best
way to suppress asthma attacks, which also supports
our conclusion that weight gain increases the risk of
getting asthma. Moreover, some dietary habits and
nutrition they absorb are also risk factors that might
have impacts on children (Peters, Dixon and Forno
2018). Lack of vitamin D is a risk factor for the
development of asthma (Peters, Dixon and Forno
2018). Infant feeding also plays an important role in
the development of asthma among children (Figure 7)
(Miliku and Azad 2018). Breastfeeding had also been
considered as a factor, children who had been
breastfeeding while they were infants were associated
with a lower risk of asthma (Yan, Liu, Zhu, Huang
and Wang 2014). This is due to the fact that there
exists components in breast milk that can protect
against allergies (Figure 8) (Oddy 2017). Therefore,
there are multiple facets in life associated with having
asthma. Children are also expected to develop good
habits and diet to prevent asthma. Asthma
exacerbations can take place at any time, however,
there is a seasonal pattern among children (Herman,
Hannah, Moshe, Erez and Ran 2014) , it was shown
that there is an increased risk during the autumn
(Sears and Johnston 2007). However, our research
also has some flaws. Our study used BMI as the only
indicator of obesity and did not delve into some other
features that are shared by those obese people but
cannot be quantified by BMI. Another study also
pointed out that although the BMI indicator is a
measure of physical factors, it does not identify body
composition, adipose tissue, or metabolic
disturbance. The criteria represented by BMI are too
broad to capture a specific understanding of the
nature of the disease (Forno 2020).
Figure 7: The impact of breastfeeding on lung health
(Miliku and Azad 2018).
Figure 8: Factors that indues and protects against food
allergies (Friedman and Zeiger 2005).
In this study, it was proven that the positive
correlation between BMI and asthma incidence is
significant, probably because obesity may affect free
air movement in the lungs and thus can have a severe
impact on the respiratory system (Azizipour and
Yosra et al 2018). However, we still cannot define a
causation relationship between BMI and asthma
incidence. One possibility people need to consider
was that having asthma might also influence BMI
through a confounding variable, which is exercise.
Though the value of exercise as a treatment aid was
emphasized by many studies, it is also pointed out
that vigorous physical activity can trigger bronchial
narrowing and may result in bronchospasm
(McFadden and Illeen 1994). Rapid breathing may
cause evaporation of mucosal surface water and an
increase in osmolarity, resulting in mast-cell
degranulation and contraction of airway smooth
muscle (Anderson 1984). In general, exercise-
induced asthma is seen more commonly among
children and young adults because of their high levels
of physical activity. Given the controversy of the
pathogenesis of exercise-induced asthma, some
physicians would advise asthma patients not to
overexert themselves. Thus, asthma patients may on
average have a lower level of physical activity than
people without asthma, putting them at a higher risk
of having higher BMI. In short, the authors can only
reveal a positive correlation at present. Whether there
is a causation relationship between BMI and asthma
incidence is still an unsolved question that needs
further research.
In an epidemiological related study, obese
individuals with a BMI greater than 30kg/m2 had a
92% increased risk of asthma (Beuther and
Sutherland 2007). This research supports our results
sufficiently. In a separate article of the effect of
obesity on the incidence of asthma, the authors noted
that analysis of both adults and children showed there
are no prominent differences between females and
males, which is consistent with our findings as well
(Julia st al 2015). Since BMI is a comprehensive
Juvenile Asthma in the U.S. Relate Asthma Incidence to Body Mass Index
197

measurement to evaluate an individual’s body
condition, to better study the relationship between
obese condition and asthma, a more precise definition
is needed. For example, to explore and reduce the risk
of asthma in obese individuals, nutritional indicators
can be used, which better describe the inner changes
of obese patients. Studies have shown that dietary
restriction in obese asthmatic patients can improve
bronchial hyperresponsiveness, airway inflammation
and other related diseases (Dixon et al 2011). In
contrast, a high-fat diet can increase airway
neutrophilia and impair bronchodilator recovery in
obese asthmatics (Wood, Garg and Gibson 2011).
Although the results cannot give strong evidence to
demonstrate that BMI plays a decisive role in the
prevalence of asthma, other studies reveal that an
unusual high BMI (>25kg/m2) often indicates an
individual is obese in most cases, and strict diet
control is proved efficient to reduce the incidence of
asthma. Therefore, our study can better suggest obese
individuals reduce the risk of having asthma
according to their BMI.
There are also some studies stating that girls with
high BMI would have a higher risk of having asthma
(Ulrik, Lophaven , Anderson, Sørensen and Baker
2018). However, in our study, the authors find that
there is no significant difference in asthma incidence
between boys and girls with high BMI. Apart from
sex and BMI, there are also other risk factors,
ethnicity is also considered as a risk factor of having
asthma. This is consistent with the results of our study
that the non-Hispanic Black set has a larger
proportion of people having asthma than others.
While many scientific research studies show that
more physical exercise is needed, clinical trials
should also be taken into action, as obese asthmatics
have multiple consequences related to mechanical or
physiologic effects, and immune or metabolic effects
(Baffi and Cynthia et al 2015).
5 CONCLUSIONS
In conclusion, this study reveals a significant positive
correlation between BMI and asthma incidence
among juveniles no matter if they are male or female.
Although the incidence of asthma is nearly the same
for males and females with high BMI, male juveniles
have an overall higher risk of getting asthma than
female juveniles, probably because boys are more
likely to have an inconsistent growth of their airway
diameter and their lung volume in their early life
(Fuseini, Hubaida and Dawn 2017). Additionally,
other factors such as ethnicity also exert some
influence on asthma outcomes. Non-Hispanic black
juveniles are more likely to have asthma than
Mexican American juveniles and non-Hispanic white
juveniles as their weight increases. However, as
mentioned previously, there are some limitations in
this study. For example, BMI is the only indicator of
obesity used in this study. Possible improvements can
be made by including more obesity indicators and
even other measurements of body condition. This
study can provide a reference for future prevention
and treatment of juvenile asthma. One of the
takeaways is that obese juveniles should be aware of
the importance of losing weight given our result that
the risk of having asthma increases with higher BMI.
Additionally, having balanced nutrition and a good
eating habit is also a key to preventing asthma. Future
research studies should also pay more attention to
both asthma prediction and prevention. Developed to
tackle asthma problems, personalized prediction
models not only can prevent attacks but can also
reduce attacks (Fleming 2018).
REFERENCES
Azizpour, Yosra et al. “Effect of childhood BMI on asthma:
a systematic review and meta-analysis of case-control
studies.” BMC pediatrics vol. 18,1 143. 26 Apr. 2018,
doi:10.1186/s12887-018-1093-z
Anderson, S. “Is There a Unifying Hypothesis for Exercise-
Induced Asthma?” Journal of Allergy and Clinical
Immunology, vol. 73, no. 5, 1984, pp. 660–65.
Crossref, doi:10.1016/0091-6749(84)90301-4.
Beuther, D. A. & Sutherland, E. R. Overweight, obesity,
and incident asthma: a meta-analysis of prospective
epidemiologic studies. Am. J. Respir. Crit. Care Med.
175, 661–666 (2007).
Baffi, Cynthia Wilson et al. “Asthma and obesity:
mechanisms and clinical implications.” Asthma
research and practice vol. 1 1. 4 Jun. 2015,
doi:10.1186/s40733-015-0001-7
Boulet LP, Franssen E. Influence of obesity on response to
fluticasone with or without salmeterol in moderate
asthma. Respir Med. 2007;101(11):2240 -2247.
doi:10.1016/j.rmed.2007.06.031
Chen YC, Fan HY, Huang YT, Huang SY, Liou TH, Lee
YL. Causal relationships between adiposity and
childhood asthma: bi-directional Mendelian
Randomization analysis. Int J Obes (Lond).
2019;43(1):73-81.
Dixon AE, Shade DM, Cohen RI, et al. Effect of obesity on
clinical presentation and response to treatment in
asthma. J Asthma. 2006;43(7):553-558.
doi:10.1080/02770900600859123
Dhabuwala A, Cannan RJ, Stubbs RS. Improvement in co-
morbidities following weight loss from gastric bypass
surgery.Obes Surg2000;10:428–435.
ICHIH 2022 - International Conference on Health Big Data and Intelligent Healthcare
198

Dixon, A. E. et al. Effects of obesity and bariatric surgery
on airway hyperresponsiveness, asthma control, and
inflammation. J. Allergy Clin. Immunol. 128, 508–
515.e2 (2011).
Fuseini, Hubaida, and Dawn C Newcomb. “Mechanisms
Driving Gender Differences in Asthma.” Current
allergy and asthma reports vol. 17,3 (2017): 19.
doi:10.1007/s11882-017-0686-1
Fleming L. Asthma exacerbation prediction: recent
insights. Curr Opin Allergy Clin Immunol.
2018;18(2):117-123.
doi:10.1097/ACI.0000000000000428
Forno E. Moving Beyond the Confines of Body Mass Index
in the Quest to Understand Obese Asthma. Am J Respir
Crit Care Med. 2020;201(3):271-272.
doi:10.1164/rccm.201910-2031ED
Forno E. Moving Beyond the Confines of Body Mass Index
in the Quest to Understand Obese Asthma. Am J Respir
Crit Care Med. 2020;201(3):271-272.
doi:10.1164/rccm.201910-2031ED
Herman Avner Cohen, Hannah Blau, Moshe Hoshen, Erez
Batat, Ran D. Balicer; Seasonality of Asthma: A
Retrospective Population Study. Pediatrics April 2014;
133 (4): e923–e932. 10.1542/peds.2013-2022
Julia, Valerie et al. “The impact of diet on asthma and
allergic diseases.” Nature reviews. Immunology vol.
15,5 (2015): 308-22. doi:10.1038/nri3830
Lloyd A, Price D, Brown R. The impact of asthma
exacerbations on health-related quality of life in
moderate to severe asthma patients in the UK. Prim
Care Respir J. 2007;16(1):22-27.
doi:10.3132/pcrj.2007.00002
Mukherjee M, Stoddart A, Gupta RP, et al. The
epidemiology, healthcare, and societal burden and costs
of asthma in the UK and its member nations: analyses
of standalone and linked national databases. BMC Med.
2016;14(1):113. Published 2016 Aug 29.
doi:10.1186/s12916-016-0657-8
McFadden, E. R., and Ileen A. Gilbert. “Exercise-Induced
Asthma.” New England Journal of Medicine, vol. 330,
no. 19, 1994, pp. 1362–67. Crossref,
doi:10.1056/nejm199405123301907
Miliku K, Azad MB. Breastfeeding and the Developmental
Origins of Asthma: Current Evidence, Possible
Mechanisms, and Future Research Priorities. Nutrients.
2018;10(8):995. Published 2018 Jul 30.
doi:10.3390/nu10080995
Okoniewski W, Lu KD, Forno E. Weight Loss for Children
and Adults with Obesity and Asthma. A Systematic
Review of Randomized Controlled Trials. Ann Am
Thorac Soc. 2019;16(5):613-
625.doi:10.1513/AnnalsATS.201810-651SR from
gastric bypass surgery.Obes Surg2000;10:428–435.
Oddy WH. Breastfeeding, Childhood Asthma, and Allergic
Disease. Ann Nutr Metab. 2017;70 Suppl 2:26-36.
doi:10.1159/000457920
Peters U, Dixon AE, Forno E. Obesity and asthma. J
Allergy Clin Immunol. 2018;141(4):1169-1179.
doi:10.1016/j.jaci.2018.02.004
Sears MR, Johnston NW. Understanding the September
asthma epidemic. J Allergy Clin Immunol.
2007;120(3):526-529. doi:10.1016/j.jaci.2007.05.047
Ulrik CS, Lophaven SN, Andersen ZJ, Sørensen TI, Baker
JL. BMI at school age and incident asthma admissions
in early adulthood: a prospective study of 310,211
children. Clin Epidemiol. 2018;10:605-612. Published
2018 May 25. doi:10.2147/CLEP.S156310
Wood, L. G., Garg, M. L. & Gibson, P . G. A high-fat
challenge increases airway inflammation and impairs
bronchodilator recovery in asthma. J. Allergy Clin.
Immunol. 127, 1 133–1 140 (2011).
Xu S, Gilliland FD, Conti DV. Elucidation of causal
direction between asthma and obesity: a bi-directional
Mendelian randomization study Int J
Epidemiol2019;48:899–907.
Yan J, Liu L, Zhu Y, Huang G, Wang PP. The association
between breastfeeding and childhood obesity: a meta-
analysis. BMC Public Health. 2014;14:1267. Published
2014 Dec 13. doi:10.1186/1471-2458-14-1267
Juvenile Asthma in the U.S. Relate Asthma Incidence to Body Mass Index
199
