
Glaucoma and Brain Nerve Relation
Shuxin Jiang
1,† a
and Yuqi Wan
2,† b
1
Guangdong Experimental Highschool AP course, Guangzhou, Guangdong, China
2
Mounthouse School Alevel Barnet London, U.K.
†
These authors contributed equally
Keywords: Glaucoma, Retinal Ganglion Cell, White Matter, Cortex, Retinal, Central Nervous System, Optic Nerve
Neuropathy.
Abstract: Glaucoma is a common eye condition where optic nerve damage, this is not only the pathological changes in
the optic nerve its effect the brain nerve too, the human brain is a complex web of neurons and synapses,
however the eye correlated with the brain in a specific way, therefore when people study the diseases of the
eye the first thing that comes to mind is always the connection to the brain. Which means glaucoma lesions
are not limited to the retinal nerves, its damage reaches the white matter areas that are involved in the
processing and integration of visual information in the brain, which means that the damage caused by
glaucoma can reach the brain. We found researchers who used the VBM method to study whole brain
comparisons in glaucoma patients, to meticulously describing the effects of glaucoma lesions in the brain.
These two methods allow the comparison of multiple images of the brain with voxels to measure differences
in local concentrations of brain tissue, thus revealing intra cerebral differences between patients with
glaucoma and the general. It is also the relationship between glaucoma and the nerves in the brain that is at
the center of the title and exploration of this paper. The differences between the brains of glaucoma patients
and the general will be mentioned, as well as the pathogenesis of glaucoma, the treatment of the glaucoma
works through medical method and surgery are also be mentioned in this paper.
1 INTRODUCTION
Over 60 million people worldwide are diagnosed with
glaucomatous optic neuropathy, which is a disease
that could cause irreversible blindness. It is a leading
public health concern given the high prevalence. Are
large proportion of people with glaucoma still
remained undiagnosed, since the accurate decision of
glaucoma is challenging, particularly in early disease.
Patients with early glaucoma are typically unaware of
it, other patients with severer or more advanced
disease may see a shadow in their vision or a
reduction in their acuity of visual. There may be
difficulties when diagnosing glaucoma without
facilities to measure IOP and evaluate optic discs and
visual fields. A proportion of patients may experience
headache, ocular pain, nausea, vomiting, and blurred
vision if they are diagnosed as angle closure
glaucoma. Once diagnosed, glaucoma needs lifelong
a
https://orcid.org/0000-0001-9586-9021
b
https://orcid.org/0000-0001-7810-780X
monitoring, IOP is need to be monitored and
functional visual change is evaluated during the
visual field testing especially in the secondary care.
Glaucoma is referred to characteristic damage to the
optic nerve and patterns of visual field loss.
Degeneration of these nerves results in cupping, a
characteristic appearance of the optic disc and visual
loss. This results in the loss of Retinal ganglion
cells(RGCs) which carries the visual information
from the retina to the brain. After the damage, the
RGC undergo apoptosis resulting in visual loss.
Glaucoma can be classified into two broad categories:
Open angle glaucoma and angle closure glaucoma.
They can be classified by mechanism and appearance
of the anterior chamber angle. As shown in figure 1.
The dominant group of patients are diagnosed with
open angle glaucoma. While the others with severe
vision loss are diagnosed as angle closure glaucoma.
Both of the glaucoma can be primary diseases.
Jiang, S. and Wan, Y.
Glaucoma and Brain Nerve Relation.
DOI: 10.5220/0011245600003443
In Proceedings of the 4th International Conference on Biomedical Engineering and Bioinformatics (ICBEB 2022), pages 579-583
ISBN: 978-989-758-595-1
Copyright
c
2022 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
579
Secondary glaucoma can result from trauma or other
conditions such as pigment dispersion. The treatment
options for glaucoma are medical, laser, and surgical
options for them to lower IOP. Usually, patients starts
with glaucoma drop mono-therapy. However, if the
case is too difficult to control, extra drops will be
added as required. Furthermore, if the maximum
tolerant treatment is unsuccessful, a laser intervention
may be advised, in some cases, the patients may
proceed directly to surgery. Our goal is to identify the
connections between glaucoma and the brain, since
our visual function depends mostly on our nerves in
brain. Treatments for glaucoma and the nerves in our
brain which links our eyes and visions together will
be laid out.
2 GLAUCOMA
2.1 Profile of Glaucoma
Glaucoma is one of the major causes of irreversible
blindness over the world and is associated with
damages to the optic nerves and degeneration of the
retinal ganglion cell (RGC). The major risk factor is
Intraocular pressure (IOP) inside the eye. Over 60
million people worldwide are estimated with
glaucomatous optic neuropathy, in which about 8.5
million are blind (Review and MetaAnalysis). The
definition of clinical glaucoma could be defined as a
various multifactorial ocular disorders, combined
with clinically characteristic optic neuropathy, which
the optic nerve head (ONH) has potentially
progressive and clinically visible changes, including
focal or generalized neuroretinal rim thinning,
enlargement and excavation of the optic cups. This
represents the neurodegeneration of retinal ganglion
cell axons and the deformation of the lamina cribrosa;
in the early stage of glaucoma, corresponding diffuse
and localized nerve-fiber-bundle pattern visual field
loss might not be able to be detectable; while visual
acuity is initially spared, progression can lead to
complete loss of vision; The collection of clinical
features is diagnostic (Foster, Buhrmann, Quigley,
Johnson 2002).
Open-angle or angle-closure are the two subtypes
of glaucoma, where angle closure refers to the
presence of appositional or synechial iridotrabecular
contact leading to the obstruction of trabecular
meshwork and elevated IOP(Foster, Buhrmann,
Quigley, Johnson 2002).
2.2 The Human Visual Pathways
There are two parts in the human visual pathways; the
anterior visual pathway is composed of the retina,
optic nerve, and chasm and lateral geniculate nucleus
(LGN), while the optic radiations and visual cortex
are comprised in the posterior visual pathway. Over
90% of RGC axons in human project to the LGN, a
relay station which in turn projects its axons to the
visual cortex cia the optic radiation. The other 10%
of RGCs project to brain structures, including the
superior colliculus, which commands the movement
of the eye, pretectal area (pupillary reflex) and the
accessory optic system nuclei, that is the optokinetic
nystagmus (Goebel, Muckli LARS, Kim DS 2004).
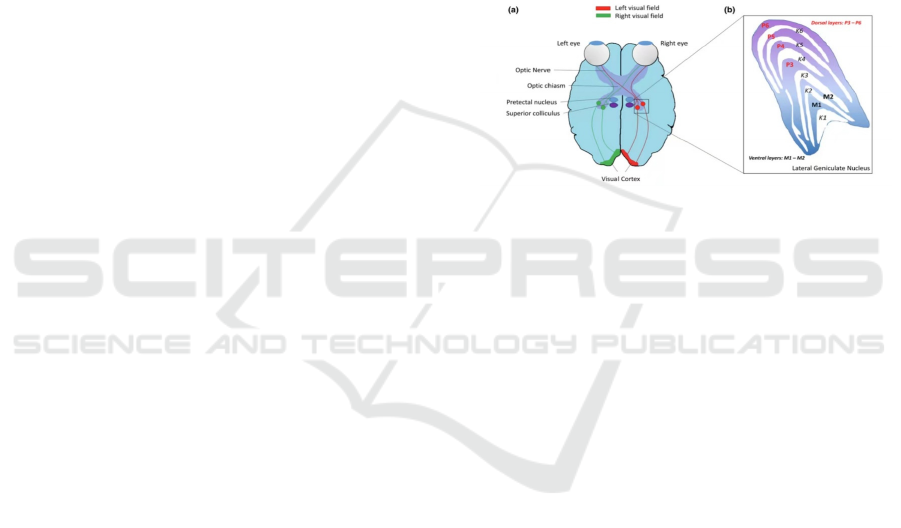
Figure 1: Overview of the human visual pathway. a
Diagrammatic representation of the human visual pathway.
b Overview of the structure of the lateral geniculate nucleus
illustrating the organization of magnocellular (M-cells),
parvocellular (P-cell), and Koniocellular cells (K-cells)
2.3 Visually Relates Imaginary
Structure
Most visual functions are controlled by the occipital
lobe, a small section of the brain near the back of the
skull. However, processing eyesight is a complicated
work, the other parts of the brain will also need to be
involved. The occipital lobe is responsible for
receiving the data from our visions. Thus, injuries or
illnesses which could affect the occipital lobe can
cause detrimental effects such as visual disturbances
or even blindness.
The connections throughout the eye and the brain
utilizes a structure in brain called the pons. It is
shaped as a horse-shoe composed of transversed
nerve fibres, lying above medulla oblongata and
bellow cerebellum. It controls the movements of the
eye, sending signals which helps the eye respond to
the correct stimulus of light. The lights reflects into
our eyes strikes photo-receptor cells in the retina
called rods and cones. Rod cells only respond when
the surrounding area is in a dim condition thus it is
responsible for our peripheral vision and night vision,
while cone cells react to brighter light, giving us
ICBEB 2022 - The International Conference on Biomedical Engineering and Bioinformatics
580

When light hits its corresponding rod or cone, the cell
activates, then it transmits a nerve impulse through
the optic nerve. This impulse ends up at the occipital
lobe, where it ’s processed and perceived as a visible
image. Occasionally, occipital lobe sends this visual
information to the hippocampus in the temporal lobe,
stored as a memory.
3 GLAUCOMA EXPERIMENT
3.1 Glaucoma Neuropathy
Glaucoma neuropathy is not limited to retinal
ganglion cells, it can affect the entire visual system.
In a series of studies conducted by Dr. Carlo Nucci, a
full professor of ophthalmology at the University of
Tower Vergara in Rome, and his colleagues observed
that in patients with early glaucoma, the optic nerve
damage is mainly located at the proximal end of the
eyeball, while in patients with advanced glaucoma in
the middle, the optic nerve damage is at the far back
of the eyeball. They also found that glaucoma damage
reaches the white matter areas, which are involved in
the processing and integration of visual information
in the brain. Because the retinal ganglion cell axon is
extended from the retina through the optic nerve to
the brain, the cells in its immediate vicinity can also
be damaged by glaucoma. (Gupta, Neeru,. Yücel
2007)
3.2 Use VBM to Compare
In the retina, other cells, such as anapestic cells,
regenerate and rejoin their connections after the
retinal ganglion cells are lost.Recently, researchers
have shown that glaucoma is not simply an eye
disease, but may be a disease of the central nervous
system. The central nervous system in glaucoma may
have similar or dissimilar pathogenesis to other
cranio-cerebral disorders. (Li, et al 2012) They are
using the VBM method to study whole brain
comparisons in glaucoma patients. When comparing
patients with glaucoma to those with normal
glaucoma, there were no differences in whole brain
grey matter, white matter, or brain parenchyma
volumes in patients with glaucoma. However in the
left middle frontal gyrus, right superior frontal gyrus,
right precuneus, and right angular gyrus, the volume
of the grey matter area decreased and the grey matter-
free area increased. While the volume of the white
matter area in the right middle occipital gyrus
decreased and the volume of the white matter area in
the right precentral gyrus increased, the areas of local
volume changes in brain structures in the NTG group
all correlated with GSS staging, this suggests that
glaucoma does not cause changes in the volume of
grey matter, white matter and brain parenchyma in
the whole brain, but the change have probability to
displayed and the analysis was generally based on
reduction. changes in brain structures in the NTG
group were mainly concentrated in frontal lobe (left
middle frontal gyrus, right superior frontal gyrus and
right precentral gyrus), occipital lobe (right
precuneus, right middle occipital gyrus) and parietal
lobe (right angular gyrus). The frontal lobe is not only
the processing and adjustment center for higher
cognitive functions, but is also responsible for
initiating, monitoring and modifying emotions. It has
a specific role in emotional decision-making and
emotional self-regulation and response inhibition.
(Iau, Ptc, et al. 2004) Numerous studies agree that
patients with glaucoma have varying degrees of
deficits in emotion regulation, which may be
associated with structural damage and dysfunction in
brain regions. Another study found a close
relationship between glaucoma and various
degenerative diseases of the central nervous system,
mainly manifesting as widespread brain atrophy. The
processing of visual information has extensive
connections with other brain regions and plays an
important role in the integration of visual information
with other sensory systems. Several studies have
shown a reduction in the volume of the right middle
gyrus of the group occipital lobe to support the NTG
In patients, there is indeed localized atrophy of the
occipital lobe, which is sufficient to suggest that
glaucoma damage extends beyond the visual cortex
and also affects the wider central nervous system. (
Iau, Ptc , et al. 2004)
3.3 The Pathogenesis of Glaucoma
The pathogenesis of glaucoma can be grouped into
two main categories: the mechanical theory and the
vascular theory. The mechanical theory emphasizes
the role of IOP and suggests that elevated IOP causes
deformation and displacement of the layers of the
sieve plate, resulting in shear forces that block the
axoplasmic flow of optic nerve cells in the sieve plate
area and reduced production and transport of axonal
proteins, leading to impaired cellular
metabolism.(Garaci, Francesco, et al., 2009) In
contrast, the vascular theory suggests that due to
various causes of impaired microcirculation in the
optic nerve papilla, the supply of nutrients to the optic
papilla and its surrounding tissues is reduced, causing
the tissue there to become stunted or damaged, and
Glaucoma and Brain Nerve Relation
581

damage to the optic nerve fibers occurs due to
ischemia and hypoxia and loss of protection from
surrounding tissues. A one-sided emphasis on the role
of mechanical or vascular theories in the pathogenesis
of glaucoma is biased. The mechanical theory does
not fully explain the occurrence of normal Intraocular
pressure glaucoma and signs of high Intraocular
pressure, while the vascular theory does not exclude
an important role for Intraocular pressure in the
pathogenesis of glaucoma. Therefore, it is generally
accepted that the pathogenesis of glaucoma is a
multifactorial and integrated process. ''Glaucoma is
an optic neuropathy with characteristic optic nerve
damage and corresponding impairment of visual
function". (Gupta, Neeru, Yücel. 2001)This suggests
that progressive damage to the optic nerve head is the
essential feature of glaucoma and can therefore be
divided into factors that cause damage to the optic
nerve head and factors that resist damage to the optic
nerve head according to the role of various factors in
the pathogenesis of glaucoma Normal people are able
to achieve a paradoxical balance between factors that
cause damage to the optic nerve head and factors that
resist damage to the optic nerve head making The
optic nerve head is protected from damage. In
patients with glaucoma, the balance is disturbed when
the optic nerve head damaging factor is enhanced or
the anti-optic nerve head damaging factor is
weakened for some reason unilaterally, resulting in
progressive damage to the optic nerve head.(Garaci,
Francesco, et al. 2009)
4 MEDICAL TREATMENT FOR
GLAUCOMA
4.1 Glaucoma Drops
The goal of treating glaucoma is to slow down the
disease's progression and preserve the quality of life.
Intraocular pressure reduction is the only proven
method to achieve this objective. Several multicenter
trials have shown that this procedure can prevent the
development and slow the disease's progression. The
initial target pressure should be decreased gradually
over time to a level that is considered ideal for
patients. It should also be adjusted depending on the
evolution of the condition. For instance, even though
the target pressure has been set, it may still need to be
lowered due to disease progression. Several classes of
pressure-lowering drugs are available. They can be
used with or without a schedule of events. The choice
of medication can be influenced by the cost, safety,
and efficacy of the drug.(Weinreb, Aung , Medeiros
2014) Glaucoma drops have the ability to lower the
IOP by changing the production or the out flow of
outflow of aqueous humour from the eye. Primary
treatments are usually Prostagladin analogues since
they possess the greatest ability to lower the IOP,
furthermore, profiles showcased that they also have
the smallest side effects. These side effects from
using the drops often causes blurring and transient
stinging, some may also cause discomfort in eyes,
redness or stimulating the growth of eyelashes.
Adherence to glaucoma drops is variable and difficult
to evaluate. (Kass, Gordon, Meltzer 1986) This
causes it to be hard to evaluate whether if the effects
of therapeutic is not enough or if the patients fail to
use the drops properly. If the IOP have not been
controlled, once the amount of drops a patient can
have exceeds, laser or surgical invention may be
needed.
4.2 Laser Treatment
Laser trabeculoplasty could be considered as as a
primary selection for the patients. It lowers the IOP
for open angle glaucoma by increasing the out flow.
This procedure of Laser trabeculoplasty is clinically
based.A recent systematic review of laser
trabeculoplasty highlighted the lack of data
comparing the effectiveness of this procedure with
modern medical and surgical options. (Rolim de
Moura, Paranhos, Wormald, 2007) The process of
which it opens the drainage tube, allowing more fluid
to drain from the eye, therefore reducing the pressure.
Another laser treatment could be cyclodiode laser
treatment, which it destruct some of the tissues with
in the eye that produces the liquid that is causing
pressure.
4.3 Surgery
This option is often suggested when the formal
treatments cannot succeed in lowering the IOP. Yet,
it could be used earlier if the patient have difficulties
in using the drops or whose presenting with advanced
glaucoma. The standard operation of glaucoma
creates aguarded fistula into the wall of the eye
(sclera), which allows a slow egression of aqueous
humour from the anterior chamber into the
subconjunctival space. (Wong, Husain, Ang,
Gazzard, Foster, Htoon, et al 2013) Trabeculectomy
is the commonest surgical method of reducing eye
pressure. It involves debridement of a small portion
of the trabecular meshwork, or adjacent corneal and
scleral tissue, to provide a drainage pathway for water
ICBEB 2022 - The International Conference on Biomedical Engineering and Bioinformatics
582

to drain from the eye into the conjunctiva and be
absorbed under the conjunctiva. Anti-scarring drugs
are often used at the surgical site to reduce the fibrotic
response and improve the success of the procedure,
but may increase the incidence of complications such
as infection and very low intraocular pressure
damage. A recent meta-analysis comparing
trabeculectomy with non-penetrating procedures
(deep sclerectomy, mucosal ostomy and catheter
angioplasty) concluded that although trabeculectomy
was more effective in reducing blood pressure, the
risk of complications was higher. ( Weinreb, Aung,
Medeiros 2014)
5 CONCLUSIONS
Glaucoma is not limited to retinal ganglion cells, it
can affect the entire visual system. Damage reaches
the white matter areas involved in processing and
integration of visual information in the brain. we
integrated the studies of VBM and Dartel methods of
whole brain comparisons in patients. Which suggest
that glaucoma damage extends beyond the visual
cortex and also affects the wider central nervous
system. Glaucoma damage is complex and
widespread. What we need to do in the future is to
pay more attention to the effects of glaucoma on the
central nervous system, and to study and compare the
differences between patients In order to better
understand the central nervous system glaucoma in
different disease stages, more methods are needed to
treat eye diseases. Strategies to prevent the
progression of glaucoma disease should also take into
account the degeneration of the central nervous
system other than wisdom and optic nerve head.
REFERENCES
Classification of glaucoma in prevalence surveys. Br J
Ophthalmol 86:238–242
FFoster PJ, Buhrmann R, Quigley HA, Johnson GJ (2002)
The definition and classification of glaucoma in
prevalence surveys. Br J Ophthalmol 86:238–242
Foster PJ, Buhrmann R, Quigley HA, Johnson GJ (2002)
The definition and
Garaci, Francesco G., et al. "Optic nerve and optic radiation
neurodegeneration in patients with glaucoma: in vivo
analysis with 3-T diffusiontensor MR imaging."
Radiology 252.2 (2009): 496-501.
Garaci, Francesco G., et al. "Optic nerve and optic radiation
neurodegeneration in patients with glaucoma: in vivo
analysis with 3-T diffusiontensor MR imaging."
Radiology 252.2 (2009):496-501.
Goebel R, Muckli LARS, Kim DS (2004) Visual system.
In: Hum. Nerv. Syst. Elsevier, San Diego, pp 1280–
1305
Gupta, Neeru, and Y. H. Yücel. "Glaucoma and the brain."
Journal of glaucoma 10.5 (2001): S28-S29.
Gupta, Neeru, and Yeni H. Yücel. "What changes can we
expect in the brain of glaucoma patients?." Survey of
ophthalmology 52.6 (2007): S122-S126.
Iau, Ptc , et al. "Are Medullary Breast Cancers an Indication
for BRCA1 Mutation Screening? A Mutation Analysis
of 42 Cases of Medullary Breast Cancer." Breast
Cancer Research & Treatment 85.1(2004):81-8
Kass MA, Gordon M, Meltzer DW. Can ophthalmologists
correctly identify patients defaulting from pilocarpine
therapy? Am J Ophthalmol 1986;101:524-30.
[12]Rolim de Moura C, Paranhos A Jr, Wormald R.
Laser trabeculoplasty for open angle glaucoma.
Cochrane Database Syst Rev 2007;4:CD003919.
Li, Changying, et al. "Voxel-based morphometry of the
visual-related cortex in primary open angle glaucoma."
Current eye research 37.9 (2012): 794-802.
Review and MetaAnalysis. Ophthalmology 121:2081–
2090. doi:
Weinreb RN, Aung T, Medeiros FA. The Pathophysiology
and Treatment of Glaucoma: A
Review. JAMA.2014;311(18):1901–1911.
doi:10.1001/jama.2014.319210.1016/j.
ophtha.2014.05.013
Wong MH, Husain R, Ang BC, Gazzard G, Foster PJ,
Htoon HM, et al. The Singapore 5-Fluorouracil Trial:
intraocular pressure outcomes at 8 years.
Ophthalmology 2013; published online 1 Mar.
Glaucoma and Brain Nerve Relation
583
