
Research on the Correlation between the Blood Lipid Metabolism
Level and Lung Cancer based on LIS Database
Yong Feng
a
, Juan Feng
b
and Yuxin Li
c
Qingdao West Coast New District People's Hospital, Qingdao, Shandong, China
Keywords: LIS Database, Health Data Analysis, Lung Cancer, Blood Lipid Metabolism.
Abstract: In recent years, the incidence of lung cancer has gradually increased, ranking second in malignant tumors,
and the mortality rate ranks first. Laboratory Information Management System (LIS) is a set of laboratory
information management system specially designed for hospital laboratory. LIS can network experimental
instruments and computers. LIS realizes intelligent, automated and standardized management of
complicated operation processes such as specimen scanning and registration, experimental data access,
report review, printing and distribution, and experimental data statistical analysis. The hospital will analyze
a large amount of test data every day, generate test reports, and store them in the LIS database through the
network. In this study, 1710 lung cancer patients were selected as the experimental group, and 1123 healthy
people who visited a doctor during the same period were selected as the control group. In this study, the LIS
database was used to analyze the correlation between the two groups of blood lipid metabolism levels. The
study found that the metabolic levels of serum total cholesterol (CHO), triglyceride (TG), high-density
lipoprotein (HDL-C) and apolipoprotein AI (ApoAI) in patients with lung cancer were significantly lower
than those in the physical examination population. There was no significant difference in low density
lipoprotein (LDL) and apolipoprotein B (ApoB) between the two groups. In this study, the LIS database was
used to retrieve medical and health data, and the LIS data was fully utilized to verify the correlation between
human blood lipids and lung cancer metabolic levels. This study has confirmed that the metabolic levels of
human serum total cholesterol (CHO), triglyceride (TG), high-density lipoprotein (HDL-C) and
apolipoprotein AI (ApoAI) can be used as important evaluation indicators for lung cancer.
1 INTRODUCTION
1
The incidence of lung cancer has risen to second
place in cancer, mortality ranks first, a serious
impact on people 's lives and health(Siegel 2019).
Studies have found that the metabolism of blood
lipids is related to the occurrence and prognosis of
tumors(
Lauby-Secretan 2016
). Abnormal lipid
metabolism can be used as a reference for the
diagnosis of tumor(
Xenoulis 2011, Kitahara 2011, Ahn
2009
). Excessive proliferation of cancer cells can
cause abnormal metabolism of blood lipids(
Pavlova
2016, Mancini 2018,
Sung 2019). Studies at home and
abroad have shown that abnormal lipid metabolism
was accompanied by changes in lipoprotein
metabolism in patients with malignant tumors.
Changes in lipid metabolism were associated with a
a
https://orcid.org/0000-0002-4515-560X
b
https://orcid.org/0000-0002-7321-7732
c
https://orcid.org/0000-0002-7793-6451
variety of malignant tumors(
Baenke 2013, Fiorenza
2000, Guan 2020
). In this study, the original health
data were collected by LIS database, and the data
were analyzed by SPSS statistical software package.
The indicators of dyslipidemia were expressed as ⎯x
± s. The analysis of variance was used to compare
the dyslipidemia between the lung cancer group and
the normal physical examination group. In this
study, the LIS database was used to extract medical
health data, which can effectively reduce the
statistical error and improve the accuracy of the
experimental results. This study shows that the
decrease of blood lipid metabolism can be used as an
important evaluation index for the deterioration of
lung cancer patients, and provides reference for
clinicians to observe the development of lung cancer
patients.
278
Feng, Y., Feng, J. and Li, Y.
Research on the Correlation between the Blood Lipid Metabolism Level and Lung Cancer based on LIS Database.
DOI: 10.5220/0011292500003438
In Proceedings of the 1st International Conference on Health Big Data and Intelligent Healthcare (ICHIH 2022), pages 278-283
ISBN: 978-989-758-596-8
Copyright
c
2022 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved

2 MATERIALS AND METHODS
2.1 Research Object
With the help of LIS database, 1710 patients with
pulmonary malignant tumors treated in the hospital
from January 2019 to June 2021 were selected as the
experimental group.
2.2 Standard Constrain
There were 1168 males and 542 females in the
experimental group; they were 24–92 years old with
an average age of ( 63.79 ± 9.10 ) years old. (1)
Patients diagnosed as pulmonary malignant tumor
by pathological examination; (2) no history of
surgery, radiotherapy and chemotherapy; (3)
Patients had the results of fasting blood lipid
examination during the morning of hospitalization;
(4) Complete clinical data of patients.
2.3 Method
In the lung malignant tumor group, 3ml of fasting
peripheral venous blood was taken in the early
morning of hospitalization and delivered to the
laboratory Beckman AU5800 automatic biochemical
analyzer for unified testing. Reference standards for
each test item: total cholesterol: 0-5.17mmol/L,
triglycerides: 0-2.3mmol/L, high-density lipoprotein
cholesterol: 1.29-1.55mmol/L, low-density
lipoprotein cholesterol: 0-3.37 mmol/L,
Apolipoprotein AI: 1.0-1.6g/L, Apolipoprotein B:
0.6-1.1g/L.
2.4 Statistical Analysis
The SPSS statistical software package was used to
analyze the research data. The measurement data
was represented by ⎯x±s parallel analysis of
variance or t test, and the count data was represented
by n(%) parallel X
2
test. P<0.05 indicated that the
difference was statistically significant.
3 RESULT
3.1 Abnormal Distribution of Blood
Lipids
689 of CHO cases were abnormal in the
experimental group, accounting for 40.29%, and 685
cases in the control group were abnormal,
accounting for 61.00%. The difference between the
two groups was statistically significant (P<0.05).
141 of TG cases in the experimental group are
abnormal, accounting for 8.25%, and 201 cases in
the control group were abnormal, accounting for
17.90%. The difference between the two groups was
statistically significant (P<0.05).
845 of HDL-C cases were abnormal in the
experimental group, accounting for 46.69%, and 292
cases in the control group were abnormal,
accounting for 23.88%. The difference between the
two groups was statistically significant (P<0.05).
276 of ApoAI cases in the experimental group
were abnormally decreased, accounting for 16.14% ,
345 cases were abnormally elevated, accounting for
20.18%, 13 cases in the control group were
abnormally decreased, accounting for 1.16%, and
348 cases were abnormally elevated, accounting for
30.99%. The difference between abnormal increase
and abnormal decrease between the two groups was
statistically significant (P<0.05).
81 of ApoB cases in the experimental group were
abnormally decreased, accounting for 4.74% , 657
cases were abnormally elevated, accounting for
38.42%, 78 cases in the control group were
abnormally decreased, accounting for 6.95%, and
443 cases were abnormally elevated, accounting for
39.45%. The difference between abnormal increase
and abnormal decrease between the two groups was
statistically significant (P<0.05). See Table 1.
Table 1: Distribution of dyslipidemia.
Lung cancer Control
Chi-squ P value
Abnormality(n) Proportion(%) Abnormality(n) Proportion(%)
Cho 689 40.29 685 61.00 116.3 <0.0001
TG 141 8.25 201 17.90 59.50 <0.0001
HDL-C 845 46.69 292 23.88 162.0 <0.0001
LDL 448 26.20 273 24.31 1.28 0.259
ApoAI
(reduction)
276 16.14 13 1.16
182.3 <0.0001
ApoAI
(ascension)
345 20.18 348 30.99
ApoB
(reduction)
81 4.74 78 6.95
7.35 <0.05
ApoB
(ascension)
657 38.42 443 39.45
Research on the Correlation between the Blood Lipid Metabolism Level and Lung Cancer based on LIS Database
279

3.2 Comparison of Abnormal Blood
Lipid Metabolism in Different Age
Groups
In the experimental group, 206 cases (29.90%) were
under 60 years old, 271 cases (39.33%) were 60 to
69 years old, 212 cases (30.77%) were over 70 years
old, and the control group was 60. There were 343
cases (50.0 7%) under the age of, 209 cases
(30.51%) between 60 and 69 years old, and 133
cases (19.42%) over 70 years old. The difference in
total cholesterol metabolism abnormalities between
the two groups of different age groups was
statistically significant (P<0.05).
In the experimental group, 33 cases (23.40%)
were under 60 years old, 51 cases (36.17%) were 60
to 69 years old, 57 cases were over 70 years old
(40.43%); control group was 60 101 cases (50.25%)
were under the age of, 72 cases (35.82%) were 60 to
69 years old, and 28 cases (13.93%) were over 70
years old. There was a statistically significant
difference in triglyceride metabolism between the
two groups of different age groups (P<0.05).
In the experimental group, there were 133 cases
(29.69%) under 60 years old, 168 cases (37.50%)
between 60 and 69 years old, and 147 cases
(32.81%) over 70 years old in the experimental
group; There were 150 cases (54.95%) under 60
years old, 79 cases (28.94%) between 60 and 69
years old, and 44 cases (16.12%) over 70 years old.
There was a statistically significant difference in the
abnormality of low-density lipoprotein metabolism
between the two groups at different ages (P<0.05).
The experimental group was abnormally
elevated, 96 cases (27.83%) under 60 years old, 125
cases (36.23%) between 60 and 69 years old, 124
cases (35.94%) over 70 years old; 170 cases
(48.85%) under 60 years old in the control group, 60
101 cases (29.02%) were 69 years old and 77 cases
(22.13%) were over 70 years old. There was a
statistically significant difference in the abnormal
metabolism of apolipoprotein AI between the two
groups of different ages (P<0.05).
The experimental group was abnormally
elevated, with 197 cases (29.98%) under 60 years
old, 257 cases (39.12%) between 60 and 69 years
old, 203 cases (30.90%) over 70 years old; 233 cases
(52.60%) under 60 years old in the control group, 60
138 cases (31.15%) were 69 years old and 72 cases
(16.25%) were over 70 years old. The difference in
abnormal metabolism of apolipoprotein B between
the two groups of different ages was statistically
significant (P<0.05). See Table 2.
Table 2: Distribution of dyslipidemia.
≤60(Age,n,%) 61-69(Age,n,%) ≥70(Age,n,%)
Chi-squ
P-value
Lung cancer Control Lung cancer Control Lung cancer Control
Cho
206
(29.90%)
343
(50.07%)
271
(39.33%)
209
(30.51%)
212
(30.77%)
133
(19.42%)
60.27 <0.0001
TG
33(23.40%)
101
(50.25%)
51(36.17%) 72(35.82%) 57(40.43%) 28(13.93%)
38.25 <0.0001
HDL-C
300
(35.50%)
117
(40.07%)
356
(42.13%)
104
(35.62%)
189
(22.37%)
71(24.32%)
3.869 0.145
LDL
133
(29.69%)
150
(54.95%)
168
(37.50%)
79(28.94%)
147
(32.81%)
44(16.12%)
49.05 <0.0001
ApoAI
(reduction)
93(34.07%) 7(
53.85%)
124
(45.42%)
4(30.77%) 56(20.51%) 2(15.38%)
2.145 0.342
ApoAI
(ascension)
96(27.83%)
170
(48.85%)
125
(36.23%)
101
(29.02%)
124
(35.94%)
77(22.13%)
34.11 <0.0001
ApoB
(reduction)
22(27.16%) 27(34.62%) 39(48.15%) 25(32.05%) 20(24.69%) 26(33.33%)
4.300 0.117
ApoB
(ascension)
197
(29.98%)
233
(52.60%)
257
(39.12%)
138
(31.15%)
203
(30.90%)
72(16.25%)
61.98 <0.0001
3.3 Comparison of the Results of Blood
Lipid Determination between the
Two Groups
The metabolic levels of CHO (5.03±1.20) mmol/L,
TG (1.40±1.04) mmol/L, HDL-C (1.32±0.33)
mmol/L, ApoAI (1.32±0.29) g/L of the experimental
group and the control group CHO (5.52±1.14)
mmol/L, TG (1.75±1.26) mmol/L, HDL-C
(1.52±0.34) mmol/L, ApoAI (1.48±0.20) g/L have
statistically significant differences (all P<0.05 ) was
shown in Table 3 and Figure 1.
ICHIH 2022 - International Conference on Health Big Data and Intelligent Healthcare
280
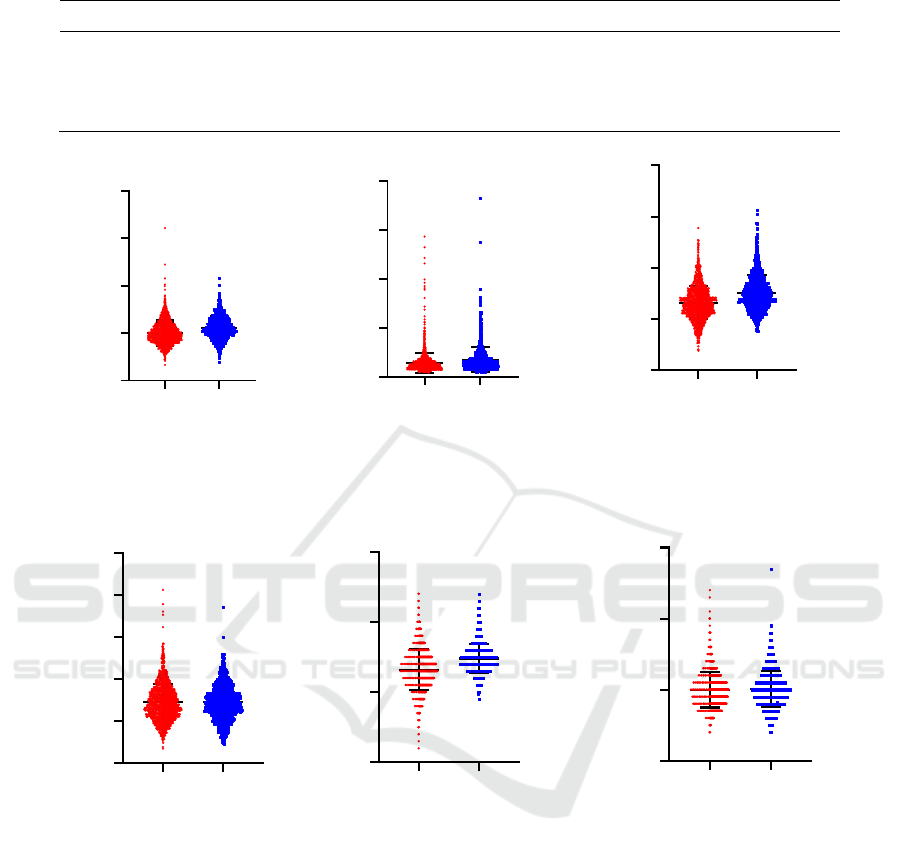
Table 3: Comparison of blood lipid determination results between the two groups (mmol/L, g/L).
Group n Cho TG HDL-C LDL ApoAI ApoB
Lung cancer 1710 5.03±1.20 1.40±1.04 1.32±0.33 2.88±0.86 1.32±0.29 0.99±0.25
Control 1123 5.52±1.14 1.75±1.26 1.52±0.34 2.87±0.80 1.48±0.20 1.00±0.26
t value 10.77 7.88 15.72 0.10 15.60 0.92
P value <0.0001 <0.0001 <0.0001 0.92 <0.0001 0.36
Figure 1: Comparison of the classification of blood lipid results between the two groups.
4 DISCUSSION
Lung malignant tumor was the cancer with the
highest mortality rate among malignant tumors. In
recent years, research on the metabolism of lung
malignant tumors has always been the focus of
everyone's attention. On the basis that the baseline
data was not statistically significant, this study used
the LIS database to retrieve medical data of 1,710
patients with lung malignant tumors, and compared
them with 1,123 health examiners in the same
period.
The study found that the abnormal distribution of
blood lipids was compared. Among them, 689 cases
(40.29%) in the experimental group of serum total
cholesterol (CHO) were abnormal, 685 cases
(61.00%) in the control group were abnormal, and
141 cases in the experimental group were
triglycerides (TG) ( 8.25%) abnormality, control
group 201 cases (17.90%) abnormality;
Lu
n
g
c
ancer
g
ro
u
p
C
on
tr
ol
g
ro
u
p
0
5
10
15
20
Cho(mmoL/L)
t=10.77
P<0.0001
L
u
ng c
ancer
gr
o
u
p
C
ontrol grou
p
0
5
10
15
20
TG(mmoL/L
)
t=7.88
P<0.0001
L
u
ng cancer
g
ro
u
p
C
ontr
o
l
g
r
ou
p
0
1
2
3
4
HDL-C(mmoL/L)
t=15.72
P<0.0001
L
un
g
c
an
c
e
r
gro
u
p
C
o
nt
rol
gr
o
u
p
0
2
4
6
8
10
LDL(mmoL/L)
t=0.10
P=0.92
L
u
n
g c
a
n
c
e
r
grou
p
C
o
n
tr
o
l
gr
o
u
p
0
1
2
3
ApoA1(g/L)
t=15.60
P<0.0001
L
ung canc
er
gr
o
u
p
C
ontrol grou
p
0
1
2
3
ApoB(g/L)
t=0.92
P=0.36
Research on the Correlation between the Blood Lipid Metabolism Level and Lung Cancer based on LIS Database
281

experimental group HDL-C (HDL-C) 845 cases
(46.69%) abnormality, control group 292 cases
(23.88%) abnormality; experimental group
apolipoprotein AI (ApoAI) 276 cases (16.14%) were
abnormally decreased, 345 cases (20.18%) were
abnormally increased, 13 cases (1.16%) were
abnormally decreased in the control group, and 348
cases (30.99%) were abnormally increased; the
experimental group apolipoprotein B ( ApoB)
abnormally decreased in 81 cases (4.74%),
abnormally increased in 657 cases (38.42%),
abnormally decreased in 78 cases (6.95%) in the
control group, and abnormally increased in 443 cases
(39.45%). There were 448 cases (26.20%) abnormal
low-density lipoprotein (LDL) in the experimental
group and 273 cases (24.31%) in the control group.
The difference between the two groups was not
statistically significant (P>0.05).
In the determination results of the two groups of
blood lipids, the experimental group's CHO
(5.03±1.20) mmol/L, TG (1.40±1.04) mmol/L,
HDL-C (1.32±0.33) mmol/L, ApoAI (1.32±0.29) g
/L Metabolic level was different from the control
group CHO (5.52±1.14) mmol/L, TG (1.75±1.26)
mmol/L, HDL-C (1.52±0.34) mmol/L, ApoAI
(1.48±0.20) g/L Statistical significance (P<0.05).
Blood lipids participate in the formation of
human cell membranes, and play an important role
in the body's inflammatory response and signal
transduction. During the occurrence and
development of lung malignant tumors, the rapid
growth of cells causes abnormal metabolism of
blood lipids. The metabolic changes of blood lipids
will further affect the cellular metabolism of lung
malignant tumors. This study found that the
metabolic levels of CHO, TG, HDL-C, and ApoAI
in patients with lung malignant tumors were
significantly lower than those of normal healthy
people, and the metabolic levels of LDL and ApoB
were no different from those of normal healthy
people. The reason for this result was the abnormal
proliferation of cells in patients with lung malignant
tumors, which require a large amount of blood lipids
to synthesize cell membranes. As the degree of
malignancy increases, the consumption of blood
lipids increases, and the metabolic level of blood
lipids decreases.
5 CONCLUSIONS
The use of LIS database to retrieve a large number of
patients' health data for correlation analysis of blood
lipids and lung malignancies was an important
research method. In this study, a large amount of
health data was collected, and with the help of SPSS
statistical software, the chi-square test was used to
analyze the correlation between the patient's blood
lipid metabolism and lung malignant tumors. The
metabolism of CHO, TG, LDL, HDL-C, ApoAI, and
ApoB in patients with lung malignant tumors and
healthy people in the same period was selected as
the evaluation criteria. Studies have found that the
metabolic levels of CHO, TG, HDL-C, and ApoAI
in patients with lung malignant tumors were
significantly lower than those of healthy people on
physical examination, confirming that the metabolic
levels of CHO, TG, HDL-C, and ApoAI play a role
in the occurrence and development of lung
malignant tumors. The metabolic levels of LDL and
ApoB are not statistically significant between
patients with lung malignant tumors and healthy
people.
Although this study has achieved some
preliminary results, it also has the shortcomings and
limitations of applying retrospective data and single-
institution analysis. In the next stage, this study will
further use LIS database to carry out prospective and
specific index research to further confirm the
research conclusions and provide a new diagnostic
basis for the occurrence and development of lung
malignant tumors
REFERENCES
Ahn J, Lim U, Weinstein SJ, Schatzkin A, Hayes RB,
Virtamo J, Albanes D. Prediagnostic total and high-
density lipoprotein cholesterol and risk of cancer.
Cancer Epidemiol Biomarkers Prev.
2009,18(11):2814-2821.
Baenke F, Peck B, Miess H, Schulze A. Hooked on fat:
the role of lipid synthesis in cancer metabolism and
tumour development. Dis Model Mech.
2013,6(6):1353-1363.
Fiorenza AM, Branchi A, Sommariva D. Serum
lipoprotein profile in patients with cancer. A
comparison with non-cancer subjects. Int J Clin Lab
Res. 2000,30(3):141-145.
Kitahara CM, Berrington de González A, Freedman ND,
Huxley R, Mok Y, Jee SH, Samet JM. Total
cholesterol and cancer risk in a large prospective study
in Korea. J Clin Oncol. 2011,29(12):1592-1598.
Lauby-Secretan B, Scoccianti C, Loomis D, Grosse Y,
Bianchini F, Straif K; International Agency for
Research on Cancer Handbook Working Group. Body
Fatness and Cancer--Viewpoint of the IARC Working
Group. N Engl J Med. 2016,375(8):794-798.
Mancini R, Noto A, Pisanu ME, De Vitis C, Maugeri-
Saccà M, Ciliberto G. Metabolic features of cancer
ICHIH 2022 - International Conference on Health Big Data and Intelligent Healthcare
282

stem cells: the emerging role of lipid metabolism.
Oncogene. 2018,37(18):2367-2378.
Pavlova NN, Thompson CB. The Emerging Hallmarks of
Cancer Metabolism. Cell Metab. 2016,23(1):27-47.
Siegel RL, Miller KD, Jemal A. Cancer statistics, 2019.
CA Cancer J Clin. 2019,69(1):7-34..
Sung H, Siegel RL, Torre LA, Pearson-Stuttard J, Islami
F, Fedewa SA, Goding Sauer A, Shuval K, Gapstur
SM, Jacobs EJ, Giovannucci EL, Jemal A. Global
patterns in excess body weight and the associated
cancer burden. CA Cancer J Clin. 2019,69(2):88-112.
Xenoulis PG, Levinski MD, Suchodolski JS, Steiner JM.
Serum triglyceride concentrations in Miniature
Schnauzers with and without a history of probable
pancreatitis. J Vet Intern Med. 2011,25(1):20-5.
YuG, KunH. The relationship between dyslipidemia and
the prognosis of non-small cell lung cancer [J]. China
Journal of Modern Medicine I Chin J Mod Med,
2020,0,30(8):33-39.
Research on the Correlation between the Blood Lipid Metabolism Level and Lung Cancer based on LIS Database
283
