
Change in Prostate Cancer Stage over Time
Fei Zhang
a
Biostatistics and Data Science, Weill Cornell Medicine College, Cornell University, New York, U.S.A.
Keywords: PSA, Prostate Cancer, Chi-Squared Test, Proportionality Test, Early Diagnosis.
Abstract: Prostate cancer is a form of cancer that occurs in the prostate gland cells among males and it is the second
most common type of cancer among males in the US. In early 1990, the American Urological Association
(AUA) and the American Cancer Society (ACS) started recommending annual prostate cancer screening with
Prostate-specific antigen test (PSA) which is a blood test. In October 2011, the US Preventive Service Task
Force (USPSTF) published a final guideline recommending against the use of PSA based screening for
prostate cancer. The influence of the use of PSA on the diagnosis rate of prostate cancer, especially in the
early stage, has become a hot research topic. The goal of this paper is to determine whether there has been a
change in proportion of men diagnosed with localized/regional prostate cancer over time due to the changes
in PSA screening recommendations, and whether this change of proportion is associated with other risk
factors. This paper uses Chi-Squared test, proportionality test and other methods to analysis data. There was
significant difference between the proportion of localized/regional prostate cancer in year 2004 and 2015 as
USPSTF recommended against the use of PSA based screening. Age, racial, region and marital status
significantly affect the distribution of the proportion of initial stage prostate cancer.
1 INTRODUCTION
Prostate cancer is a form of cancer that occurs in the
prostate gland cells among males and it is the second
most common type of cancer among males in the US.
As per a 2016 CDC annual report, for every 100,000
men in the US, 101 new prostate cancer cases were
reported in the year 2014 and of those cases, 19
died(Centers for Disease Control and Prevention). In
early 1990, the American Urological Association
(AUA) and the American Cancer Society (ACS)
started recommending annual prostate cancer
screening with Prostate-specific antigen test (PSA)
which is a blood test. PSA is made by the prostate
gland and high levels of PSA may be indicative of
prostate cancer or other non-cancerous conditions.
PSA screening was a cheaper and non-invasive
alternative to a digital rectal exam which is one main
reasons for PSA based screening being recommended
even though there was no supported clinical trial
evidence for PSA accurate indicator of prostate
cancer. There was an alarming increase in the
incidence rates as PSA based screening became more
common and by 1992 the incidence rate of prostate
a
https://orcid.org/0000-0003-3199-0521
cancer in the US nearly doubled. Mei Aobing et
al(Aobing et al. 2017, Mistry, Cable 2003, Zhao,
Huang, Cheng et al. 2014, Kramer, Brown, Prorok, et
al. 2013). questioned the sensitivity and specificity of
PSA, especially when PSA is between 4.00 ng/mL
and 10.00 ng/mL. There is an overlap between
SERUM PSA levels in PATIENTS with benign
prostatic hyperplasia (BPH)and prostaticcancer
(PCa), making it difficult to distinguish benign
prostatic hyperplasia from prostate cancer. K. Mistry
et al (Mistry, Cable 2003). 's study found that chronic
prostatitis, indplacement of urinary ducts, prostate
massage, and other conditions can lead to abnormal
PSA test results, that is, PSA is a prostate-specific
marker rather than a marker of prostate cancer. In
October 2011, the US Preventive Service Task Force
(USPSTF) published a final guideline recommending
against the use of PSA based screening for prostate
cancer (USPSTF).
The significant change in incidence rates and
diagnosis levels of prostate cancer cases over the last
few decades points towards a possibility of
overdiagnosis and overtreatment due to these policy
changes. There is scope to further study and evaluate
the impact of this change in the policy and scientific
308
Zhang, F.
Change in Prostate Cancer Stage over Time.
DOI: 10.5220/0011368700003438
In Proceedings of the 1st International Conference on Health Big Data and Intelligent Healthcare (ICHIH 2022), pages 308-313
ISBN: 978-989-758-596-8
Copyright
c
2022 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved

landscape over the years. Early diagnosis, timely
operation and effective endocrine therapy can greatly
reduce the mortality rate of prostate cancer.
Therefore, to study the causes and influencing factors
of prostate cancer and determine the susceptible
population will provide an important basis for
effective prevention, early diagnosis and improved
survival rate. The goal of this project is to determine
whether there has been a change in proportion of men
diagnosed with localized/regional prostate cancer
(out of the total number of diagnosed prostate cancer)
over time due to the changes in PSA screening
recommendations, and whether this change of
proportion is associated with age group, the race
groups, region groups and marital status. Chang et al
(
Chang 1996). 's study found that PSA increased with
age, and different age groups had different effects on
PSA. The older you are, the greater the impact. In
addition, the mean prostate volume of all ages also
increased with age, and the prostate volume increased
with age. There has been a change in proportion of
men diagnosed with localized/regional prostate
cancer (out of the total number of diagnosed prostate
cancer) over time due to the changes in PSA
screening recommendations. And this change of
proportion is associated with age group, the race
groups, region groups and marital status.
2 METHOD
2.1 Data
The Surveillance, Epidemiology, and End Results
(SEER: https://seer.cancer.gov/) database which is
maintained by the National Cancer Institute (NCI),
was used for this study. The database extract contains
28% of all cancer cases in the US, diagnosed between
2004 and 2015. The data was collected from 18
different population-based registries and contains
incidence as well as survival records of patients by
patient ID. The dataset is deidentified and is
compliant with HIPAA regulations regarding
protection of patient privacy and intended use of the
data for research purposes. There is a total of about
1.94 million patient records out of which 230,326
records are associated with prostate cancer. Each
record contains a patient ID, registry ID, year and
month of diagnosis, age at diagnosis, histology
(stage) and other demographic information such as
race, birth year, sex. A check for duplicates yielded
31 patients with 2 diagnoses at different points of
time, only initial records were as the evaluation is
primarily based on the initial prostate cancer
diagnosis.
2.2 Statistical Analysis
Since the raw data contained 133 columns, it was
essential to select the relevant variables, filter the
essential categories, and create categorical variables
for age groups as well as diagnosis dates (before or
after PSA final guidelines). In the cleaning process,
male patients diagnosed with prostate cancer in
interested stages were selected from the original
SEER dataset. Duplicate records, patients with age
under 50 years old, and unrelated variables and stages
were removed. Then The clean data was then
grouped cases by race, region, marital status, and age
group to yield number of cases as a function of time
(month-year). In order to test the difference in
proportion of localized relative to the overall cases in
different categories (race, age group, geographical
region, marital status), we used proportionality test
for two groups and Chi-squared test of independence
in case of multiple groups. These non-parametric tests
were used after making sure that the following
requirements were met. Variables are categorical
(binary) in nature: Prostate Cancer
Stage(Localized/Regional and Distant). All cases
belonged to a single population. Data management
and statistical analyses were performed using R,
version 4.1.1.
3 RESULTS
In general, the widespread adoption of PSA-based
prostate cancer screening caused a stage migration
toward earlier stage of prostate cancer at diagnosis
(95% CI 0.0347 - 0.0451) during the early 2000s.
Thus, there was significant difference between the
proportion of localized/regional prostate cancer in
year 2004 and 2015 as USPSTF recommended
against the use of PSA based screening. The dotted
line marks the time when USPSTF released their final
guidelines (October 2011) and after which, there is a
sharp linear decrease in the proportion of
localized/regional cases detected in the following
years (Figure 1).
Change in Prostate Cancer Stage over Time
309
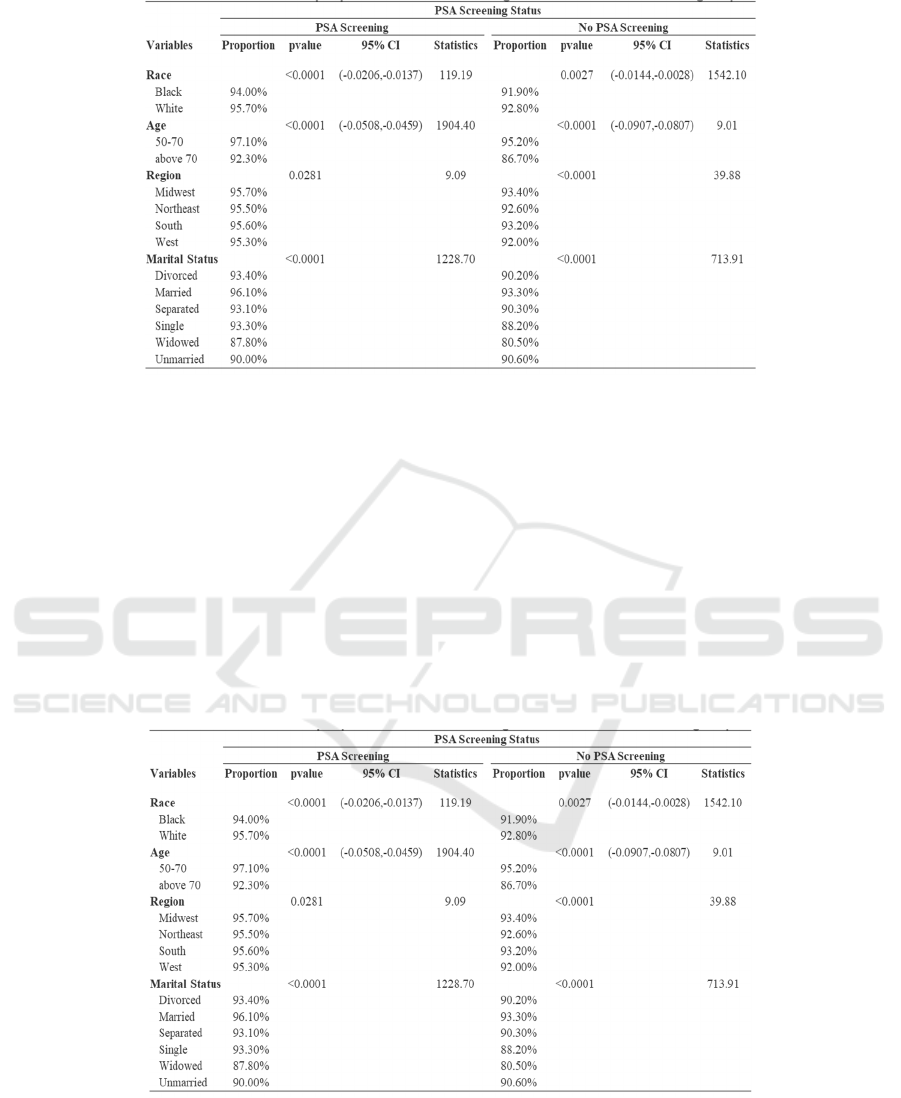
Figure 1: Proportion of US Males Diagnosed with Initial Stage Prostate Cancer Over Time.
3.1 Age Groups
From 2004 to 2015, the proportion of
localized/regional prostate cancer for age group
greater than 70 years was less than that of 50-70 years
age group. Moreover, the proportions of both the age
groups were stagnant during the time period between
2004 and October 2011, however there was
significant decrease in proportions of both age groups
since October 2011(Table1). The two-proportion z-
test showed that there were differences in proportion
of men diagnosed with localized/regional disease by
age groups: 50-70 and over 70 (χ2 statistic: 327.07,
95% CI: -0.06 - -0.056). The influence of PSA
screening guideline change on the proportion was
different for both age groups (with PSA screening:
95% CI -0.0508 - - 0.0459, without PSA screening:
95% CI -0.0907 - -0.0807). The plot shows that the
age group of individuals over 70 years experienced a
steeper decrease in proportions as compared to the
50-70 years age group.
Table 1: Summarized Results of Statistical TestsConducted on All Groups.
3.2 Race Groups
During the period from 2004 to 2015, the proportion
of localized/regional cases decreased for both major
race groups (black and white) after October 2010. The
proportion among white males was greater than black
males and two-proportion z-test showed that the
difference in the overall proportion by race was
statistically significant (χ2 statistic: 117.92, 95% CI
0.012 - 0.018). The influence of PSA screening
guideline change in the proportion among black and
white patients was different (with PSA screening:
ICHIH 2022 - International Conference on Health Big Data and Intelligent Healthcare
310

95% CI -0.0508 - -0.0459, without PSA screening:
95% CI -0.0907 - -0.0807).
3.3 Region Groups
All the regions (Midwest, Northeast, South, and
West) showed a decrease from 2010 with slight
variations in trends. Chi-squared test showed that
there is an association between the US regions and the
proportions (χ2 statistic: 35.384, df = 3, p-value <
0.0001). So, there is sufficient evidence to state that
the influence of PSA screening on proportion of
localized/regional stage varies between different US
geographical regions.
3.4 Marital Status
Marital status was divided as Divorced, Married,
Separated, Single, Unmarried or domestic partner and
Widowed. In the period between 2004 and 2015,
there were slightly variance and experience decrease
since 2010 in marital status. The unmarried group has
some outliers on the lower end of the proportion range
in the time trend analysis, however smoothing shows
similar trend lines among all marital status. The
married group has the highest proportion of regional
stage prostate cancer cases from 2004 and 2015,
while widowed group had the least. Chi-squared test
of independence shows that there is an association in
the proportion of men diagnosed with
localized/regional disease with marital status:
Divorced, Married, Separated, Single, Unmarried or
domestic partner and Widowed (χ2 statistic: 1928.10,
df = 5, p-value < 0.0001). Additionally, the influence
of PSA screening on proportion of localized/regional
stage depends on marital status (with PSA screening:
χ2 = 9.088, df = 3, p-value = 0.02814, without PSA
screening: χ2 = 39.878, df = 3, p-value < 0.0001).
4 DISCUSSION
Many articles have confirmed that age, residence,
race, and marital status have a significant impact on
the diagnosis of prostate cancer. The incidence of
various tumors is very different in different countries
in the world. Even the incidence of different regions
in the same country is also very different. For
example, the country with the highest incidence of
gastric cancer is Japan, the incidence of colorectal
cancer is the highest in the United States, and Sweden
has the highest incidence of prostate cancer. For
different regions, the probability of occurrence of
each type of cancer is different in each region, which
may be affected by local eating habits, weather, air
quality, water quality and other external
environmental factors.
From the analysis of internal reasons, the
incidence of cancer may be related to mental state,
mental quality, happiness index, personal physical
fitness and so on. Many researchers have proven
through genetics that people of different regions and
races have different genes for prostate cancer
susceptibility, and the order of these genes is also
inconsistent, which will fundamentally affect the
prevalence and incidence of cancer. Nan Di et al (
nan,
Yun 2019, Li 2003) found that the differences in the
genotype and allele frequency distribution of
susceptibility genes between different races in
prostate cancer caused the abnormal incidence of
prostate cancer, which can directly participate in the
development of prostate cancer. Occurrence and
development. There are obvious differences in the
incidence of prostate cancer among people of
different races and regions, and the incidence varies
dozens of times. Studies by foreign scholars have
shown that there are obvious differences in the
incidence of prostate cancer among different ethnic
groups in the United States, such as Indians, African
Americans, Mexican Americans and Asian
Americans. Studies by domestic scholars have shown
that there are obvious differences in the distribution
of your genotypes under the front ranks of different
ethnic groups, which may affect the hormone levels
and biological effects of different individuals. VDR
genes and androgen-related gene polymorphisms
have obvious racial types, and they are different from
each other. The incidence of prostate cancer is the
same in different races.
Genetic factors are undoubtedly the main factors
affecting the incidence of prostate cancer, and the
differences in genetic gene sequences between
different races are the main factors contributing to the
huge differences in the incidence of prostate cancer
among different races. Those studies’ results are
consistent with this paper.
Besides, a study found a significant increase in the
incidence of prostate cancer among Asian
immigrants. It suggests that factors such as geography
and dietary habits may play a role in the development
of prostate cancer. Chuiguo Huang (
Huang 2018) used
multi-factor Cox regression analysis, survival
analysis and other methods to confirm that related
factors such as age, race, marital status, PSA
concentration, T stage in TNM staging, tumor tissue
grading, and the use of different interventions are
affecting the Gleason score of 8. Separate
Change in Prostate Cancer Stage over Time
311

independent risk factors for the prognosis of prostate
cancer patients.
In addition, prostate-specific antigen (PSA), as
the most valuable tumor marker for prostate cancer,
only has the specificity of prostate tissue but not the
specificity of prostate cancer. Various prostate tissues
(including normal tissues, benign hyperplasia tissues
and cancer tissues) are PSA can be secreted, leading
to its lack of specificity and sensitivity in the
diagnosis of early prostate cancer. For a long time,
clinicians have used total PSA = 4.0 ng/ml as the
threshold for screening prostate cancer (PCa) and
non-prostate cancer and has been widely used.
However, a large number of studies have shown that
in patients with tPSA≤4.0 ng/ml, the incidence of
prostate cancer is not low; and among patients with
tPSA>4.0 ng/ml, 75% of patients do not have prostate
cancer. Therefore, the use of a single PSA indicator
with fixed threshold value to diagnose prostate cancer
has a higher false positive rate and false negative rate.
Many new studies have shown that the original
threshold of the PSA method should be adjusted
according to the patient's actual physical condition
and past medical history. For example, big data
analysis and machine learning methods can be used
to obtain a new PSA threshold for early warning PCa
in the T2DM population (the original threshold 4.0
ng/ml), and calculate its sensitivity and specificity.
Probability function fitting is used to estimate the
distribution of PSA levels in the overall population,
support vector machines are used to calculate new
thresholds, and receiver operating characteristic
(ROC) curves are used to test its diagnostic efficacy.
This article only analyzed several risk factors.
However, change in proportion of men diagnosed
with localized/regional prostate cancer over time due
to the changes in PSA screening recommendations
may associated with other factors other than age
group, the race groups, region groups and marital
status. Besides, this article can use survival analysis,
multivariate statistical analysis and other models to
study more risk factors and influencing factors of
prostate cancer in the future. MIC can be used to carry
out factor correlation analysis on the large and
complex medical data of major hospitals, and then
obtain more accurate relationships and visual images
from the complex data. New models or other methods
can be used to further analyze the impact of the policy
of discontinuing the PSA screening
recommendations.
5 CONCLUSIONS
A statistical analysis of the SEER dataset helped us
understand the effects of healthcare policies on
prostate cancer diagnosis levels over the years. The
overall proportion of cases with localized/regional
prostate cancer show a slight increase between 2004
and mid of 2008 which is due to the prominence of
PSA-based prostate cancer screening. In 2008, the
overall proportion started declining due to rising
awareness of overdiagnosis of initial stage
(localized/regional) of prostate cancer from PSA
screenings. Additionally, during this time (2008) the
USPSTF began recommending men over the age of
75, against PSA screening tests which led to a steeper
decline in the proportion of initial stage cases in the
above 70 years age category. In October 2011, the
USPSTF issued a draft recommending against PSA
screening for other age groups as well and due to this
a steep linear decline in the proportion of initial stage
prostate cancer can be seen across all categories: race,
region, marital status, and age group. Statistical tests
were conducted to determine if the proportions
between the groups (within each category) were
significantly different. Table 1 shows that the p-value
for the proportionality tests was consistently less than
the level of significance (0.05), due to which we could
reject the null hypothesis (proportions are equal).
Thus, we can conclude that the proportions of initial
stage (localized/regional) prostate cancer cases were
significantly different between age groups (50-70 and
above 70) as well as racial groups (black and white).
It was also found that the proportions of men
diagnosed with initial stage of prostate cancer were
statistically different between 2004 and 2015, based
on the sample size. In order to obtain a detailed
analysis, it was important to look at the proportion
trends by other factors like marital status and regions
in the US. Histogram of proportionvalues for
different regions showed that the distributions had
different variances, and Chi-Squared test indicated
the total proportions for the regions are statistically
different. Finally, marital status also significantly
affected the distribution of the proportion of initial
stage prostate cancer. Due to the differences in
domestic and foreign policies, the current domestic
research in China focuses on other research based on
PSA screening recommendations. The main research
directions are as follows. Factors affecting prostate
cancer. Whether the threshold value of the detection
index needs to be adjusted according to the patient's
actual situation such as past medical history and how
to adjust. In addition to the current detection methods
and indicators taken into account, do you need to add
ICHIH 2022 - International Conference on Health Big Data and Intelligent Healthcare
312

other indicators to make the detection results more
reliable and effective, avoid biased results, and reduce
unnecessary testing for patients. At present, few
scholars or institutions have studied the influence of
the existence of PSA screening on the efficiency of
prostate cancer diagnosis. This article fills this
loophole very well, and hope that this article
encourages more scholars to study the detection
method itself. With the rapid development of
computers, statistical learning and artificial
intelligence deep learning algorithms are gradually
being integrated with medicine. Use artificial
intelligence, big data complex analysis and other
emerging computing methods to explore new
research methods based on medical observation data,
and then better diagnose. It is also possible to analyze
the influencing factors of prostate cancer from a new
perspective. In addition to the four factors mentioned
in the article, as well as many genes that are currently
being studied, there are actually many factors that can
be analyzed. Humans are social animals and are
affected by various factors, such as psychological
factors, diet, and water sources.
REFERENCES
Centers for Disease Control and Prevention. United States
cancer statistics: 1999–2014 cancer incidence and
mortality data. https://nccd.cdc.gov/uscs/
Chuiguo Huang. A nomogram for analyzing prognostic
features in patients with Gleason 8 prostate tumor[D].
The Second Clinical College of Zhengzhou University:
Department of Urology, 2018
Di nan, Zhizhong Yun. Research progress on ethnic
differences and susceptibility to prostate cancer
genome[J]. Journal of Clinical Medical,
2019,6(06):194-195.
Jiangping Chang. Effects of gland volume and age on
prostate specific antigen in benign prostate
hyperplasia[J]. Journal of Clinical Urology, 1996(4):
207-209.
KramerB S, Brown ML, Prorok PC, et al. Prostate cancer
screening: What we know and what we need to know
[J]. Annals of internal Medicine, 2013,119 (9) : 914-
923.
Mei Aobing, et al. The correlation study and clinical
guidance of serum EPCA-2 and PSA in the diagnosis of
early prostate cancer[J]. Guizhou Medical Journal,
2017(9): 917 - 920.
Mistry K, Cable G. Meta-analysis of prostate-specific
antigen and digital Rectal examination for prostate
carcinoma: A meta-analysis [J]. Journal of the
American Board of Family Practice, 2003,16 (2) : 95-
101.
Ming Li. The incidence of prostate cancer and associated
factors[J]. China Cancer, 2003(12): 4-7.
U.S. Preventive Services Task Force (USPSTF). Rockville,
MD: U.S. Dept. of Health & Human Services, Agency
for Healthcare Research and Quality
Zhao R, Huang Y, Cheng G, et al. Developing a follow-up
Strategy for Patients with PSA Ranging from 4 to
10ng/mL via a New Model to Reduce Unnecessary
Prostate Biopsies [J]. Plos One, 2014,9 (9): e106933-
e106933.
Change in Prostate Cancer Stage over Time
313
