
Early Rehabilitation Training for Patients with Transfemoral
Amputation before Wearing Prosthesis
Lu Bai
School of Biomedical Engineering, Capital medical university, Beijing,100069, China
Keywords: Transfemoral Amputation, Rehabilitation, Deformity Prevention, Prosthetic Adaptation.
Abstract: Due to trauma and disease, the number of patients with transfemoral amputation is increasing year by year.
Exploring early rehabilitation methods for transfemoral amputation is becoming more and more important.
After finding the problems and consulting multiple documents, I found several methods for the problems.
Early rehabilitation training can not only meet the appearance needs of patients with transfemoral
amputations, but also provide preliminary preparations for patients before wearing prostheses. It can also
prevent or reduce the occurrence of deformities, and reduce training obstacles and training time for patients
when wearing prostheses.
1 INTRODUCTION
The number of amputations caused by trauma or
disease is increasing year by year. The amputation
will not only bring personal and physical trauma to
the individual, but it will also deal a heavy blow to a
family. Although early rehabilitation treatment and
prosthetic adaptation can help amputees return to
society early and resume activities of daily living as
soon as possible. However, due to the limited medical
level in some places, or the failure of family members
to contact the rehabilitation team in time, many
patients have deformities of the residual limbs due to
various reasons after amputation, and also due to the
need for physical mechanisms to compensate, which
cause the uninfected side disease (Xu 2018).
Therefore, in order to better fit the prosthesis and
meet the needs of patients for appearance, it is
necessary to prevent or reduce the deformity of the
residual limb. It is hoped that early functional
exercises can improve the convenience of patients to
adapt to prostheses and reduce the occurrence of
deformities. In this way, more amputees can get better
prosthetic fit and appearance satisfaction in the
future.
2 REHABILITATION AFTER
TRANSFEMORAL
AMPUTATION
The entire process of amputation should be
accompanied by the full participation of the
amputation rehabilitation team. The rehabilitation
team includes the amputee himself, doctors, nurses,
physiotherapists, occupational therapists, prosthetics,
social workers, family members, psychological
counselors, etc (Carroll 2006). In the entire process
of amputation, each worker performs their own job
function to help the amputee recover early, complete
the fitting of the prosthesis, and finally return to
society. In patients with a transfemoral amputation,
due to different amputation planes, unbalanced
muscle strength and poor posture, patients often
cause flexion and abduction deformities, and the
higher the amputation plane, the more obvious the
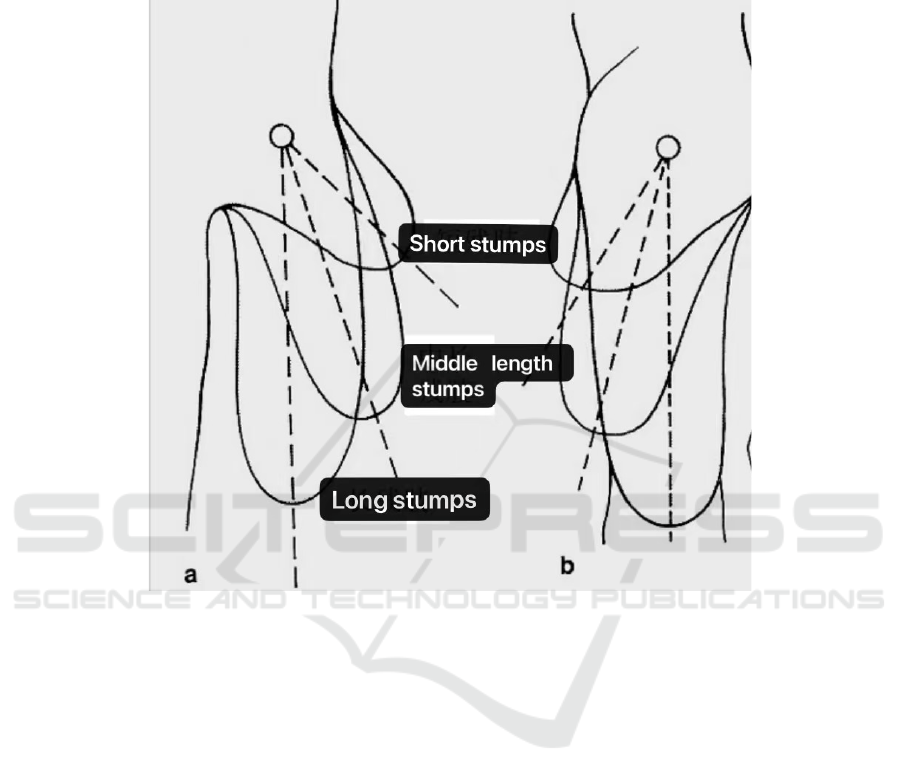
deformity is, as is shown in figure 1. When the thigh
stump has deformities, it will be difficult to make and
fit the prosthesis in the later stage. Early rehabilitation
training can avoid or reduce the formation of
deformities, which can not only bring the greatest
beautification of the appearance to the patient, but
also reduce the pain of the patient in the later
prosthetic fitting training.
Amputation is not only a destructive but also a
reconstruction and repair operation, which creates a
good residual value condition for the installation of a
104
Bai, L.
Early Rehabilitation Training for Patients with Transfemoral Amputation before Wearing Prosthesis.
DOI: 10.5220/0011187600003444
In Proceedings of the 2nd Conference on Artificial Intelligence and Healthcare (CAIH 2021), pages 104-108
ISBN: 978-989-758-594-4
Copyright
c
2022 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
prosthesis. Lower limb amputation requirements: the
residual limb has good weight-bearing capacity, can
walk after wearing a prosthesis, and the residual limb
after the amputation must have power, which is a
functional residual limb. A prosthesis is an orthopedic
device used outside the body that compensates for the
loss of the function and appearance of the limb.
Figure 1: Above knee amputation deformity.
2.1 Stump Stereotype
The ideal residual limb plays a very important role in
the late prosthetic fitting. The ideal residual limb
should achieve: (1) Proper length; (2) The residual
limb has normal joint movement, good muscle
strength, and no contracture deformities; (3) The
residual limb is covered with moderate soft tissue,
without tenderness, bone spurs, or neuroma, (4) and
the disabled no swelling of the limbs, good skin
condition, moderate skin tension, no adhesions, no
ulcers, no sinuses. After amputation or repair of the
residual limb, the soft tissue of the residual limb
undergoes greater trauma, and causes such as
capillary rupture can lead to edema. With time
passed, the edema can be slowly absorbed without
complications such as infection. Wrap the elastic
bandage in time after the operation to help reduce the
swelling and shape of the residual limb. As is shown
in Figure 2, use the eight-character winding method
when winding, follow the principle of tightening
down and loosening up, 30-40 minutes each time,
relax 2-4 times a day, and continue bandaging at
night. After amputation, the patient's affected limb
stump is wrapped and shaped with a medical elastic
bandage, which can not only reduce the pain of the
phantom limb, but also facilitate the shaping of the
limb stump, shorten the time to install the prosthesis,
and it is of great significance to improve the patient's
quality of life (Deng 2012).
2.2 Functional Training before
Assembly
Before the prosthesis is assembled, in order to
achieve the ideal rehabilitation effect, the patient
needs to undergo systematic rehabilitation training.
Through training, patients can restore physical
fitness, improve cardiopulmonary function,
strengthen muscle strength, maintain or improve joint
mobility, and make adequate preparations for wearing
prostheses.
Early Rehabilitation Training for Patients with Transfemoral Amputation before Wearing Prosthesis
105
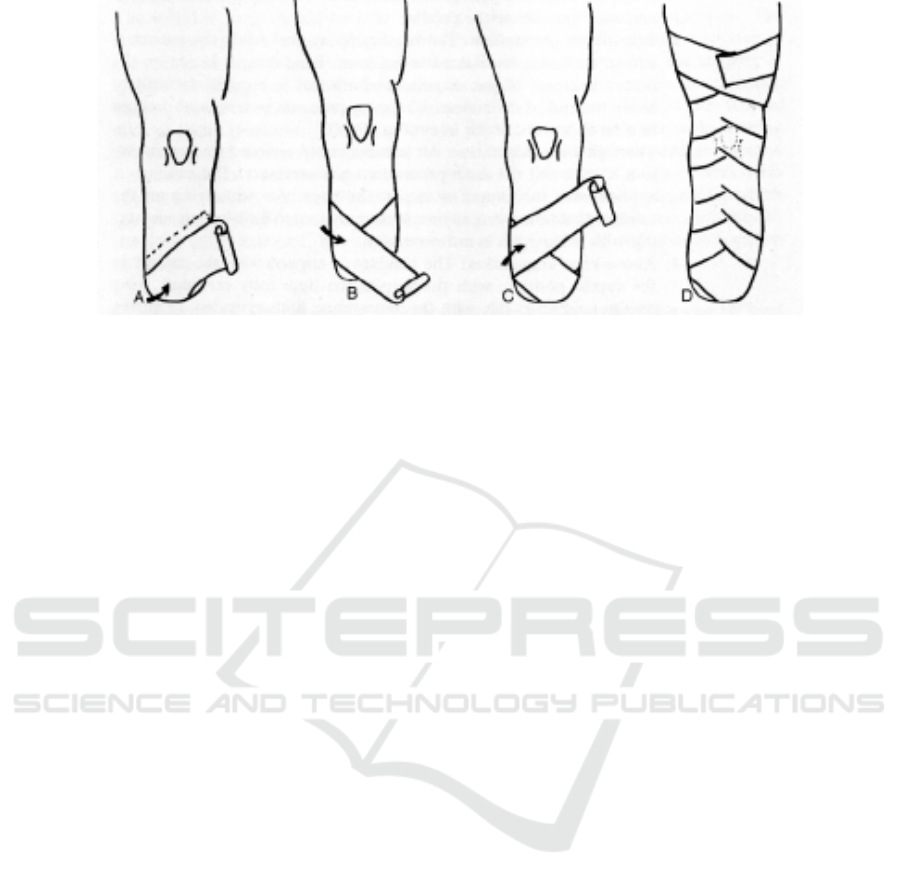
Figure 2: Horoscope bandage wrapping
2.2.1 Strength Training
In patients with thigh amputations, due to the
different amputation planes, the reduction in the
number of muscles that control a certain movement
will be different, resulting in unbalanced muscle
strength and deformity. The common deformity after
thigh amputation is flexion and abduction. Therefore,
in order to prevent the appearance of this deformity,
muscle strength training should be added early after
the amputation to strengthen the muscle strength on
the side with insufficient muscle strength. For
abduction deformities, the muscle strength of the
adductors of the thigh should be increased; for flexion
deformities, the muscle strength of the hip extensors
should be increased. Muscle training can help
patients improve muscle strength and better control
the position of the residual limb (Xiao 2016). Early
functional exercise can be combined with physical
factor therapy, which can effectively relieve the
patient's stump pain and enhance the patient's stump
muscle strength (Dilinuer 2020).
2.2.2 Range of Motion Training
For hip joint function disuse syndrome and long-term
immobilization, the joint deformity, contracture, etc.
caused by the limitation of joint range of motion, the
effective traction of the joints of the patient, and
encourage the patient to actively move, in order to
effectively improve joint function (Bao 2015).
2.2.3 Balance Training
Due to amputation, the body's center of gravity often
changes, causing the body to compensate and appear
unstable. Suspension training can strengthen the
body's core muscles, thereby improving the stability
of the patient's trunk and pelvis, strengthening the
core control ability, and enhancing the patient's
walking stability and balance ability (Sun 2019). It
can be prepared for the later adaptation of the
prosthesis.
2.2.4 the Placement of Residual Limbs and
the Prevention of Deformities
In addition to unbalanced muscle strength, patients
with thigh amputation can also cause deformity due
to abnormal posture. Therefore, after amputation, you
should pay attention to the placement of the residual
limb to avoid too high a residual limb for a long time,
which increases the possibility of flexion deformity;
or put something (such as a pillow, cushion, etc.)
between the legs to increase the possibility of
abduction deformity.
The correct posture of amputee patients which is
shown in Figure 3 include: (1) In the supine position,
lying on a hard board with the two legs tied together,
and the pelvis should be kept in a horizontal position;
(2) In the uninvolved side lying position, the affected
limb should be up and healthy. Side down, keep the
affected limb in a naturally straight posture; (3) In the
prone position, keep the hips flat on the bed with your
legs close together. It is best to sleep on your prone
for 1 to 2 hours a day; (4) When sitting, the body
Stands upright, with the center of gravity between the
legs, and the legs of the amputee patient are brought
together.
In the daily rest process, you can use
elasticbandages to tie the residual limb and the
healthy side together. Pay attention to controlling the
normal body posture, the size of the effective binding
area, the length of the effective arm, the binding time
and the amount of force applied. It can avoid other
problems caused by the occurrence of control
deformities.
CAIH 2021 - Conference on Artificial Intelligence and Healthcare
106
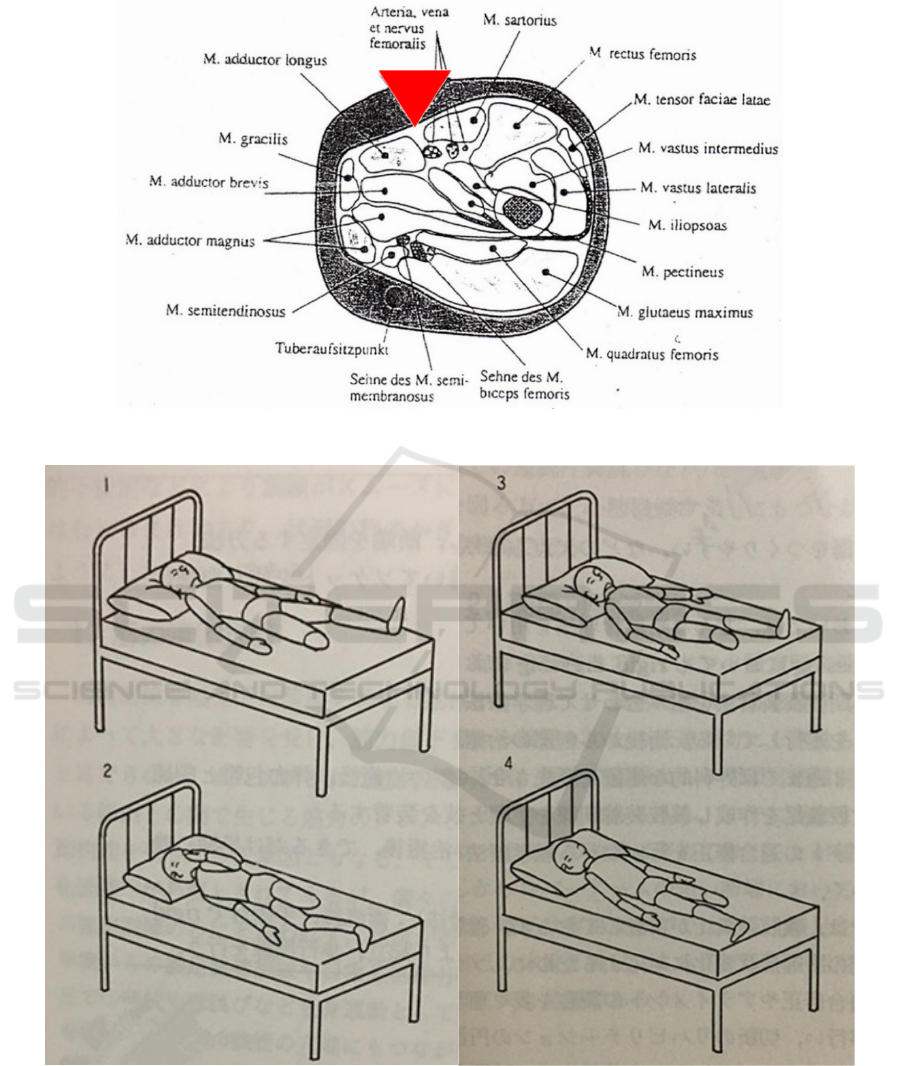
Figure 3: Schematic diagram of thigh muscles.
Figure 4: Good stump placement.
3 CONCLUSIONS
Due to the frequent occurrence of accidents and the
impact of diseases, the number of patients with thigh
amputations is increasing year by year, but
postoperative muscle atrophy, stump deformity, and
stump pain are prone to occur, which affects the
patient's prosthetic fit and quality of life.
Early Rehabilitation Training for Patients with Transfemoral Amputation before Wearing Prosthesis
107

At the same time, it effectively prevents and
alleviates the occurrence of deformities, which not
only provides aesthetics for patients, but also
provides convenience for the production and wearing
training of prostheses that are adapted in the later
stage. Early rehabilitation training after amputation
plays a very important role in shaping the residual
limb, restoring function, and preventing deformity. It
is worthy of promotion by clinical and rehabilitation
teams.
ACKNOWLEDGEMENTS
Thanks to the teachers from the Department of
Prosthetics and Orthopedics of the China
Rehabilitation Research Center for their teaching and
guidance on the content of this article. Thanks to
Professor Dario Farina from Imperial College
London for explaining to me the related content of
bionic limbs online, which enriched my vision. Thank
you from the thesis teacher for your guidance on my
writing. Thank you from the thesis teacher for your
guidance on my writing.
REFERENCES
Bao Zhongying. Observation on the curative effect of
rehabilitation training for patients with lower limb
amputation after assembling prostheses[J]. Electronic
Journal of Clinical Medicine,2015,2(13):2565,2568.
Carroll K. Prosthetics and Patient Management[M].
SLACK Inc. 2006.
Deng Haizhang, Cui Xiumei, Chen Hefeng, et al.
Application and nursing of residual limb bandaging and
shaping technique after amputation[J]. Chinese Journal
of Modern Nursing,2012,18(10):1215-1216.
DOI:10.3760/cma. j.issn.1674-2907.2012.10.038.
Dilinuer Aishan, Shen Jing. Application of physical factors
in the rehabilitation of lower limb amputation stump[J].
Diet and Health Care,2020,7(28):12.
Sun Yingcai, Duan Suqian, Zheng Hong, et al. Effects of
suspension training on balance and walking stability of
amputees[J]. Chinese Trauma and Disability Medicine,
2019,27(24):79-80.
DOI:10.13214/j.cnki .cjotadm.2019.24.052.
Xiao Zhigang. Treatment and rehabilitation of lower limb
amputation patients before prosthesis installation[J].
Journal of Aerospace Medicine,2016,27(7):845-846.
DOI:10.3969/j.issn.2095-1434.2016.07.017.
Xu Zhi, Huang Weizhi, Zhang Ming, Jiang Wentao, et al.
Biomechanical study on muscle coordination of healthy
limbs in patients with thigh amputation[C]. //The 12th
National Conference on Biomechanics and the 14th
National Conference on Biorheology Proceedings.
2018:148-148.
CAIH 2021 - Conference on Artificial Intelligence and Healthcare
108
