
Experimental Security Analysis of Connected Pacemakers
Guillaume Bour
1 a
, Marie Elisabeth Gaup Moe
2 b
and Ravishankar Borgaonkar
1 c
1
SINTEF Digital, Strindvegen 4, Trondheim, Norway
2
Department of Information Security and Communication Technology,
NTNU - Norwegian University of Science and Technology, Trondheim, Norway
Keywords:
Pacemaker, Connected IMD, Medical Device, Cyber Security, Home Monitoring Device Security.
Abstract:
Medical devices and their connectivity capabilities are providing a variety of benefits to the healthcare domain,
including remote monitoring, automated alerts, and improved patient outcomes. However, these medical
devices introduce a range of new potential cyber security risks when connected to the Internet, affecting
the patient or the healthcare infrastructure. In this paper, we systematically analyze the security issues of
connected pacemakers. In particular, we use a black box testing methodology against a commercial pacemaker
device and the network infrastructure. Our main objective is to understand how the data is sent from a bedside
monitor in the patient’s home to the backend server hosted by the pacemaker manufacturer, and whether or
not this data is protected from a cyber security perspective. To do so, we leveraged several hardware related
vulnerabilities found in the bedside monitor to obtain the firmware of the device and then reverse engineered
the proprietary communication protocol. We demonstrate how vulnerabilities in this protocol can be leveraged
to allow an attacker to perform a man-in-the-middle attack on the pacemaker.
1 INTRODUCTION
Implantable Medical Devices (IMD) in the form of
modern pacemakers are not a new medical innova-
tion but the evolution of technology from the fifties
and sixties. In the seventies “on-demand” pacemak-
ers were developed that would sense the patient’s
cardiac activity and adjust the pacing to it. These
pacemakers could be remotely programmed through a
radio-frequency telemetry link. The first pacemakers
driven by microprocessors appeared in the nineties.
These devices were able to detect cardiac events and
could adapt their internal pacing based on the pa-
tient’s needs. The first connected pacemakers ap-
peared in the early 2000s, with the addition of an
external device that would connect wirelessly to the
pacemaker and upload its data to a remote server via
the Internet, thus reducing the need for patients to go
to the clinic for a check-up. Today, this remote con-
nectivity is getting more and more popular in use. An
external device, sometimes called a “bedside moni-
tor”, which we in this paper will refer to as the Home
Monitoring Unit (HMU), is used to gather the pace-
a
https://orcid.org/0000-0003-4456-6279
b
https://orcid.org/0000-0003-1786-1133
c
https://orcid.org/0000-0003-2874-3650
maker’s data and upload it to a remote server accessi-
ble to the clinician through a web interface.
Patients’ safety has always been a key priority
in medical devices. Pacemakers are built with “fail-
safe” modes which they will switch to in case some-
thing goes wrong with its programming, to keep the
pacemaker generating a constant pulse until the pa-
tient gets seen by a pacemaker technician that can re-
program the device.
Cyber security of medical devices, on the other
hand, has not been paid much attention by researchers
or publicly debated until the last decade. The health-
care domain is however not spared by cyber crimi-
nals, and attacks like the WannaCry ransomware that
struck the world in May 2017 has shown that hospitals
and medical devices are at risk for being infected via
collateral damage even if the attack was not specifi-
cally targeted towards them, and that a cyber attack
can have a real impact on human lives.
Connected devices in the form of wearables like
the Apple Watch or the Fitbit have become increas-
ingly popular, and by extension, we are getting used
to having access to close to live data on our health.
This trend highlights the need for data protection
for all the devices that monitor our health, including
IMDs. Medical data is indeed an interesting target for
Bour, G., Moe, M. and Borgaonkar, R.
Experimental Security Analysis of Connected Pacemakers.
DOI: 10.5220/0010816900003123
In Proceedings of the 15th International Joint Conference on Biomedical Engineering Systems and Technologies (BIOSTEC 2022) - Volume 1: BIODEVICES, pages 35-45
ISBN: 978-989-758-552-4; ISSN: 2184-4305
Copyright
c
2022 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
35

criminals, who can monetize it by selling it to other
criminals on underground forums. As detailed in an
article by Robbie Richards Richards (2015), “Crim-
inal attacks are now the number one cause of secu-
rity breaches in healthcare, increasing 125% since
2010.” With medical devices being more and more
connected, the attack surface is growing, and it is thus
important to design the devices with security in mind
and not to rely on “security by obscurity” or “bolt-
on security”, which tends to be often the case when
security comes as an afterthought.
Over the past three years, we have been analyz-
ing the security of the pacemaker ecosystem of one of
the main vendors on the market today. We looked at
three different generations of HMU devices and com-
pared their security to document the state-of-the-art
and to see how security implementation in these de-
vices evolved over time.
Our results suggest that, even if the overall secu-
rity of the devices has improved, the medical device
manufacturers are still lagging behind and fail to im-
plement some common security practices.
The paper is organized as follows. Section 2 pro-
vides the background of our work, including a de-
scription of the principle of the pacemaker and its
ecosystem, along with the interactions between its
different components. Here we also review the rel-
evant related work and the threat model used in our
research. In Section 3 we outline the methodology
used along with the setup used to perform the secu-
rity analysis. Section 4 presents our main findings,
from a hardware, network, and devices management
perspective. Section 5 provides a discussion of the re-
sults along with mitigations. Section 6 concludes the
paper.
2 BACKGROUND
2.1 The Pacemaker Ecosystem
Pacemakers and Implantable Cardioverter Defibril-
lator (ICD) are active implantable medical devices,
which are defined in the Norwegian regulatory frame-
work Justis- og beredskapsdepartementet, Helse- og
omsorgsdepartementet (2005) as “Any active medi-
cal device which is intended to be totally or partially
introduced, surgically or medically, into the human
body or by medical intervention into a natural orifice,
and which is intended to remain after the procedure.”
Both pacemakers and ICDs are battery-powered de-
vices surgically implanted in a patient to treat a heart
related condition. They differ in the conditions they
are treating, as ICDs are not only capable of continu-
ous monitoring the heart rhythm and pacing the heart
with electrical pulses, but also to deliver an electrical
shock to the heart if required. In this paper, because
both ICDs and pacemakers are similar devices from
the cyber security point of view, they will both be re-
ferred to as pacemakers.
Pacemakers are constructed to last for around 10
years varying on their usage, before having to be re-
placed due to the battery running out. The devices
are able to deliver pacing when required and in a
way that is adapted to each patient. This means that
the clinician needs a way to program the device in a
non-invasive way for the patient. As previously men-
tioned, a RF-telemetry link was introduced to the de-
vices in the 70s to program some parameters in the
pacemaker. Since then, pacemakers have evolved into
complex embedded devices, driven by a microcon-
troller. Once implanted, they are not standalone de-
vices which are left there for ten years waiting to be
replaced, but take place in an ecosystem that allows
for monitoring the devices and also the patients’ con-
dition.
The Home Monitoring Unit is an example of a
communication device that enables this remote reg-
ular monitoring by connecting wirelessly to the pace-
maker, reading and transmitting data from it. Figure 1
presents the pacemaker ecosystem.
Vendor’s servers
Doctor
Programmer
HMU
Pacemaker
Patient
Figure 1: Diagram of the vendor’s pacemaker ecosys-
tem Bour (2019).
The Pacemaker. Implanted in the patient’s body,
this is the main device of the ecosystem. As already
explained, it generates an electric impulse that helps
regulate the heart rhythm.
The Programmer. The programmer is an external
computer used by a clinician to program the pace-
maker. Programming the pacemaker is achieved wire-
lessly by placing the programming head of the pro-
grammer in close proximity of the pacemaker. While
old pacemakers used to communicate with the pro-
grammer over the 175 kHz band, newer ones tend to
use 402-405 MHz Medical Implant Communications
BIODEVICES 2022 - 15th International Conference on Biomedical Electronics and Devices
36

(MICS) band Savci et al. (2005). The communica-
tion of the pacemaker with the programmer is trig-
gered by applying a magnetic field on the implant,
causing a magnetic switch inside it to close Halperin
et al. (2008). This magnetic field is emitted by the
programming head. It is to be noted that pacemakers
from different vendors require different programmers
due to differences in communication protocols, and
that a programmer of a specific vendor usually sup-
ports several pacemakers/ICD devices from the same
vendor.
The Home Monitoring Unit. The HMU is a router-
like device in charge of collecting telemetry data from
the implant and transmit it. The device is paired with a
pacemaker, placed in the patient’s home and receives
the data sent by the pacemaker at a pre-configured
time (for instance every night at 2:00). The HMU also
communicates with the pacemaker over the 402-405
MICS band, which allows for longer range communi-
cations than the 175 kHz band. This data is then sent
to a backend server, usually owned by the pacemaker
manufacturers. Similarly to the programmer, pace-
makers from different manufacturers requires differ-
ent HMUs. Some newer pacemakers communicate
over Bluetooth Low Energy with an app installed on
the patient’s smartphone, eliminating the need for an
external HMU device.
The Operator’s Network. In order to transmit the
data to the backend server, the HMU needs connectiv-
ity. To achieve that without having to rely on patients’
internet connection and also for ease of use, manufac-
turers usually have contracts with Telecom operators.
That way, the HMUs are shipped with a SIM card to
access the GSM or 3G networks, or with access to
the internet through telephone lines for older versions.
The HMU either connects directly to the server which
is exposed on the public Internet or connects to a Vir-
tual Private Mobile Network (VPMN) which gives it
access to the server. This implementation varies with
vendors.
Vendor’s Backend Infrastructure. This infrastruc-
ture is used to receive data sent by the HMU, process
it and make it accessible to the clinician through an
online platform. Alerts may also be triggered if some-
thing looks irregular, for instance, if no data has been
uploaded in a while for a given HMU, or if there is a
problem with the patient’s condition. This allows the
clinician to call in the patient for a follow-up checkup
if necessary.
2.2 Pacemaker Security Related
Research
While wireless communication technology has been
a feature of pacemakers since the seventies, security
researchers have only been taking an interest in this
topic for around 15 years. In 2008, Halperin et al.
published the first research paper describing a security
attack against a commercial pacemaker Halperin et al.
(2008). Their research targeted the communication
between the pacemaker and its programmer. Using
Software-Defined-Radio (SDR), they partially reverse
engineered the communication protocol in use and,
with that knowledge, were able not only to eavesdrop
and decode the communication, but also to perform
data replay attacks. They were able to interrogate the
pacemaker to reveal the patient’s data containing per-
sonal information such as patient’s name, diagnosis,
etc. They were also able to change parameters of the
pacemaker, such as the patient’s name, implantation
date, or even therapies (that includes turning off all
therapies). Finally, and more frightening, they were
able to trigger a shock on the ICD, which could have
fatal consequences on a real patient if delivered at an
inappropriate time. They thus highlighted the sever-
ity of the lack of security mechanisms for implantable
medical devices.
In more recent research from 2016, Marin et al.
carried out similar research on the latest generation of
pacemakers Marin et al. (2016). Their research high-
lights several weaknesses in the communication pro-
tocol and shows that a weak adversary can perform
attacks even with low capabilities. Three kinds of
attacks were performed. First, the researchers man-
aged to access private patient information from the
telemetry information, even though some obfuscation
technique was done by the manufacturer. Secondly,
they performed Denial-of-Service attacks. By keep-
ing the device in “interrogation” mode, they were able
to send messages to the device over a long-range com-
munication channel and thus drastically reduce the
implant battery life. Finally, they found that there is
no mechanism against replay attacks and that an ad-
versary without any knowledge of the protocol could
simply replay captured messages and spoof the pro-
grammer.
A report exposing vulnerabilities in the pacemak-
ers and HMUs manufactured by St. Jude (now Ab-
bot) was published by Muddy Waters Capital LLC
in 2016 Block (2016). Amongst the vulnerabilities
that were presented was a way to perform a battery-
draining attack on the pacemakers or forcing them to
pace at a rhythm that would be potentially fatal for the
patient. These attacks were carried out by first com-
Experimental Security Analysis of Connected Pacemakers
37

promising the HMU, which was then used to attack
the pacemaker. Even if no attack has been publicly
reported exploiting these vulnerabilities, the disclo-
sure of this report had a potentially severe impact on
the 260 000 HMUs deployed in patients’ homes at the
time. As a result, the vendor issued a firmware update
at the beginning of 2017 to mitigate the vulnerabili-
ties.
In 2017, Rios and Butts evaluated the security
of the pacemaker ecosystems of the four major ven-
dors Rios and Butts (2017). They presented several
weaknesses, in the programmers, the pacemaker im-
plants, and the HMUs. Weaknesses include vulner-
able third-party software, lack of authentication be-
tween devices, unencrypted filesystems and firmware,
removable hard-drives, and unsigned firmware. The
conclusion is that the whole industry is quite imma-
ture in terms of cyber security. They highlight that
this is not only the case for one unique vendor but
that all vendors are impacted.
2.3 Threat Model
In this paper, we aim at understanding the evolution
of the security measures in the pacemaker ecosystem
and to evaluate its current maturity. In our research,
we have considered two classes of adversaries:
With Physical Access to an HMU. It is possible to
buy these devices online, sometimes at the low price
range of $20 - $50. Since these are much easier to
obtain (compared to a programmer), one can afford to
experiment with them without the fear of breaking an
expensive device.
Capable of Setting up a Fake Base Station (FBS).
Such an attacker has access to Software Defined Ra-
dio equipment, which is also affordable. The HackRF
One
1
manufactured by Great Scott Gadgets costs
around $350.
The two main assets that we want to look at in
this research are the patient’s safety and privacy. As a
consequence, we study the impact of different attacks
on the patient’s treatment and how it could be inter-
fered with, directly or indirectly. Regarding the pa-
tient’s privacy, we look at what attacks would enable
an attacker to access any kind of private data about
the patient.
As mentioned in the introduction of this paper,
motivations to attack the pacemaker ecosystem vary.
Attacks against the patients’ privacy are mostly driven
by financial motives, in order to monetize the medical
data on the black market. These attacks can have a
big impact if they can be leveraged at a large scale.
1
See https://greatscottgadgets.com/hackrf/
Safety related attacks could also be motivated by fi-
nancial profit, for example we can imagine that an
adversary could leverage a vulnerability in an extor-
tion attempt by threatening a patient or maybe even
a medical device manufacturer asking for a ransom.
Targeted attacks against a single individual in order
to harm or kill are less likely, except if it is a person
of high interest. In both cases, one can imagine that
we are facing organized crime or a nation-state threat
actor. However, we cannot exclude single opportunis-
tic attackers.
3 METHODOLOGY AND
EXPERIMENTAL
ENVIRONMENT
3.1 Black Box Testing Methodology and
Target
Our research focused on the Home Monitoring Unit,
more specifically, two main attack vectors were stud-
ied: physical and network. In both cases, a black box
testing methodology was followed, as the tested com-
ponents were proprietary hardware and software of
which we had very little knowledge. In order to be
as close to a real-world scenario as possible, we used
commercial off-the-shelf (COTS) equipment when-
ever possible, and tried to keep the cost of an attack
as low as possible.
The targeted devices from our lab were acquired
second hand and are all BIOTRONIK’s devices. This
manufacturer was chosen because no prior security
research had been published for this particular pace-
maker brand, and no known vulnerabilities had previ-
ously been disclosed for its devices. Devices in our
research project include three different generations of
the HMU:
V1: From the early 2000, one of the first HMUs on
the market, using the GSM network for connec-
tivity. This version is not used anymore.
V2: From the 2010s, in two models: one using the
plain old telephone service for its connectivity, the
other one using the GSM network. This version is
not commercially available anymore, but is still in
use.
V3: From 2016, using the 3G network. This is the
current commercially available version.
BIODEVICES 2022 - 15th International Conference on Biomedical Electronics and Devices
38
3.2 Testing Setups
To perform hardware testing, as previously men-
tioned, we used a combination of several COTS
equipment: The shikra to interface with low-level
data interfaces via USB, a logic analyzer (useful to
detect non standard baud rate), the JTAGulator to
identify the pinout of the JTAG interface (it does so
by trying all possible permutations). Once the pins
were known, we used a Raspberry Pi zero as our
UART/JTAG/SPI connector.
From a network perspective, we used two different
setups:
• We developed a modem emulator to interact with
the Telephone Line version of the HMU (V2).
• A Fake Base Station (based on OpenBTS) to in-
teract with the GSM (V2) and 3G (V3) versions
of the HMUs. In addition, a network jammer was
used to prevent the HMU from connecting via the
3G network, forcing a so-called downgrade at-
tack. A virtual machine was set up to emulate the
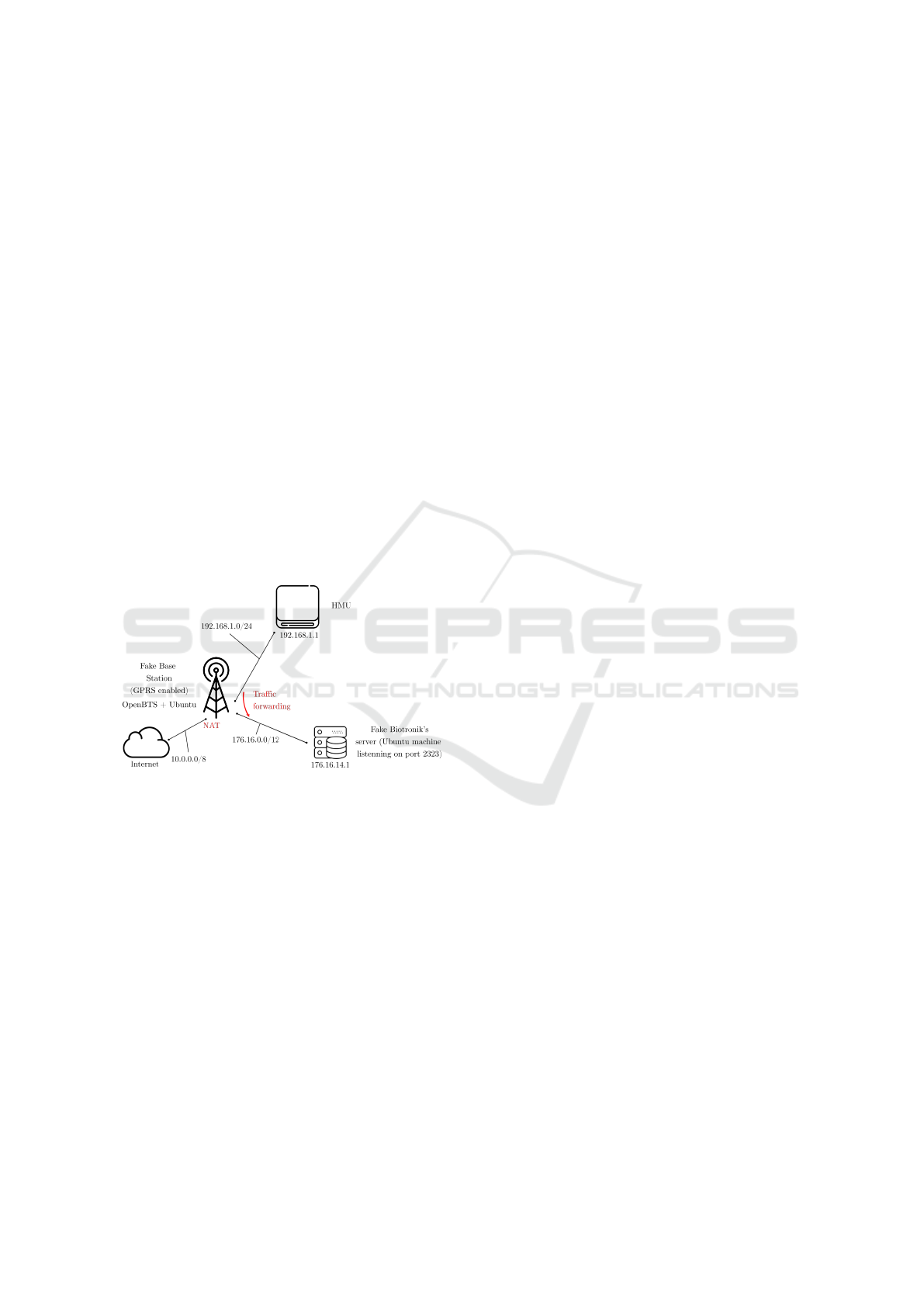
backend server of the manufacturer (as shown in
Figure 2).
Figure 2: Network diagram of the emulated network.
3.3 Ethical Considerations
Given that the devices available in our lab have been
acquired on the second-hand market, and that some
of them were not new, they could have contained po-
tentially sensitive data. This data has been systemati-
cally redacted from this paper and from previous pub-
lications. The Norwegian Centre for Research Data
(NSD) was notified at the beginning of our project,
and approved our patient data protection plan.
As the vulnerabilities discovered in the pacemaker
ecosystem during our research could have had a po-
tential impact on patients’ safety and security, our
findings were kept under embargo for one year. Dur-
ing this time the research findings were shared with
the vendor (BIOTRONIK) in the form of a vulnera-
bility report. The vendor cooperated according to a
coordinated vulnerability disclosure process and ap-
propriately analyzed and validated our report. They
then shared their responses to each reported vulner-
ability, and we discussed each point in detail. Dur-
ing these discussions, they also provided sufficient in-
formation to confirm that patient harm arising from
the vulnerabilities is very unlikely. BIOTRONIK rec-
ommends that healthcare providers and patients con-
tinue to use the investigated devices as intended and
follow device labelling. The coordinated vulnerabil-
ity disclosure process also involved the German Fed-
eral Office for Information Security (BSI), the Ger-
man Federal Institute for Drugs and Medical Devices
(BfArM), the US Cyber Security and Infrastructure
Security Agency (CISA) and the US Food and Drug
Administration (FDA). As a result of this process,
CISA issued an advisory CISA (2020).
4 SECURITY ANALYSIS OF THE
HMU
Our main objective with this project was to better
understand how the data is sent from the HMU to
the vendor’s backend servers, what kind of vulnera-
bilities exist on this part of the ecosystem and how
they could be exploited to potentially impact patient’s
safety and/or privacy. In the following sections, we
explore two classes of attack: the first focuses on
exploiting hardware vulnerabilities to compromise a
Home Monitoring Unit, and the second on how an
attacker can exploit vulnerabilities on the home mon-
itoring unit to gain access to the backend infrastruc-
ture.
4.1 Hardware Security Analysis
During the hardware analysis, we found several vul-
nerabilities:
Debug Interfaces Available. On all HMU versions
analyzed, we were able to discover the UART and
JTAG interfaces. On versions 1 and 2 the pins were
not labelled, making it harder to determine the JTAG
interface. On the latest version, however, pins were
labelled. On all versions, the UART interface seemed
disabled, and it was not possible to interact with it.
The JTAG interface on the other hand was enabled
and it is possible to fully control the microcontroller
using it. That includes dumping the contents of the
Random Access Memory (RAM) as well as the Flash
Memory, which gave access to the firmware of the de-
vice.
Experimental Security Analysis of Connected Pacemakers
39

Credentials Are Sent in Clear Text to the Modem.
When analyzing the version 2 of the HMU, we were
able to eavesdrop the communication between the
microcontroller and the modem as the pins of the
modem were exposed on the PCB. This allowed us
to get access to the credentials used by the device to
connect to the manufacturer’s Virtual Private Mobile
Network (VPMN), since these were sent in clear text.
Firmware Is Not Encrypted, Nor Obfuscated.
Once the firmware was dumped via the JTAG in-
terface, reverse-engineering revealed that it was not
encrypted or protected in any way. There was no
trace of obfuscation of the code. On the contrary,
log strings used by the device were explicit enough
to ease the process of reverse engineering. This
made it possible to create a script to easily fetch the
credentials previously acquired via eavesdropping
on the communication channel directly from the
firmware, along with other credentials used by the
device to connect to the backend server hosted by the
manufacturer.
Memory Is Not Encrypted. The memory is not en-
crypted either, meaning that anyone with physical ac-
cess to the HMU can copy it via the JTAG interface
and access the data going through the HMU, includ-
ing the patient’s data.
Hard-coded Credentials and Cryptographic Keys.
The credentials used by the devices to connect to
the network and backend servers are hard-coded and
stays the same for each connection attempt, we ob-
served however that they are unique for every device
(two different HMUs will use different credentials).
On the latest version they are stored on the external
flash which is not encrypted and whose content can
be read via the Serial Peripheral Interface (SPI).
Cryptographic material such as DES and AES keys
used in the proprietary protocol is also stored in a
similar way.
Unencrypted Communication with the Pacemaker.
Even though we have not done exhaustive research
at this interface due to limited access to working
compatible pacemakers in our lab, we found that
there is no encryption of the data exchanged between
the pacemaker and the HMU. That means that
attackers who can intercept the radio signal from the
pacemaker (the radio band is already known) can also
access the patient’s data.
Leveraging the hardware vulnerabilities exposed
above and the raw network data obtained through
the modem and server spoofing, we were able to re-
verse engineer the proprietary communication proto-
col used by the HMU to send the pacemaker data to
Figure 3: Structure of the communication protocol’s packet.
the backend server. The detailed structure of a data
packet is presented in Figure 3.
4.2 Network Security Analysis
When analyzing the security of the communication
link between the HMU and the backend server, we
identified several weaknesses in the communication
protocol.
No Mutual Authentication. We were able to spoof
the backend server and trick the HMU into sending
its data to us, highlighting the lack of mutual authen-
tication between the backend server and the HMU on
the first two versions. We did so at two different lev-
els: first at the modem level on the Telephone line
version, where we spoofed both the modem and the
backend server, and at the network level, where we
used a virtual machine, connected to the same net-
work as our OpenBTS machine, with the proper IP
address requested by the HMU, to respond to the TCP
request of the HMU (see Figure 2). The data obtained
was encrypted for the most part. However, credentials
to connect to the service were sent in cleartext before
switching to the encrypted communication.
Usage of a Proprietary Protocol over an Insecure
Transport Protocol. The version 2 and 3 of the
HMU use both GPRS and SMS to send data. On
both channels, the data is sent using the proprietary
protocol presented in section 4.1 on top of TCP. This
BIODEVICES 2022 - 15th International Conference on Biomedical Electronics and Devices
40

protocol packs, compresses (when using GPRS) and
encrypts the data.
Broken or Risky Algorithm. In the case of patient
data, the proprietary protocol uses AES CBC as the
encryption algorithm, however single DES is used in
the case of log data going over SMS. DES is a broken
algorithm from a security perspective, and log data
can thus easily be obtained by an attacker that is able
to set up a Fake Base Station in the proximity of the
HMU. An attacker having had physical access once
to the HMU can also perform the same attack on pa-
tient data by getting hold of the AES key. The keys
(AES and DES) were however random and unique per
device.
Credentials Reuse. The credentials used to connect
the VPMN and the backend services are the same and
are sent unencrypted in both cases. They are thus very
easy to obtain.
By chaining several of the vulnerabilities, we were
able to weaponize the second version of the HMU.
With physical access to the device, an attacker can in-
stall a physical device with a wireless communication
interface inside of it (the inside of the HMU casing is
big enough to add a RaspberryPi zero), and that way
gain remote access to the device. This allows an at-
tacker to not only eavesdrop on all communications
between the HMU and the backend server, but also
to act as a Man-in-the-Middle, the proprietary pro-
tocol being known. Such an adversary can also get
access to all the data sent by the pacemaker to the
HMU. This would enable an attacker to modify the
pacemaker telemetry data in order to hide a possible
problem, or to create a problem by deleting or modi-
fying pacemaker alerts and warnings that were meant
to be sent to the backend server.
4.3 Credentials & SIM Cards Validity
The HMU has two sets of credentials: the first to
connect to the network and access the manufacturer
VPMN; the second to connect to the service on the
backend server. To verify the validity of the creden-
tials, we used them on a phone with the HMU SIM
card and manually entered the settings in order to con-
nect to the VPMN. However, when using the version
2 HMU’s SIM card, we were unable to connect be-
cause the SIM card was not valid anymore.
It turned out that using a SIM card from an old
first version HMU on a newer second version HMU
worked: we were able to connect to the VPMN and
obtain an IP address inside the VPMN. To ensure we
were in the right network, a successful ping request
was sent to the server hosting the telemetry collection
service. No other testing was performed as this was
outside of our research scope and could potentially
interfere with the manufacturer’s service.
The VPMN is an additional security measure,
even if this is not its main purpose. It prevents the
patient data telemetry servers from being publicly ex-
posed to the Internet, something that for instance pro-
tects against Denial-of-Service attacks. However, as
shown in our research this protection can be bypassed
by an attacker who acquires an old device with a valid
SIM card, highlighting the need for proper decommis-
sioning procedures for old devices.
4.4 Attack Scenarios
In this subsection, we will describe two attack scenar-
ios against the HMU and more generally against the
whole pacemaker ecosystem. Figure 4 and 5 present
the attack trees for these scenarios. Arrows indicate a
requirement. An arc between several arrows indicates
an “AND” condition while single arrows indicate an
“OR” condition.
Figure 4: Attack tree for the “MitM” scenario.
The first scenario is the Man in the Middle pre-
sented in Figure 4. Given the vulnerabilities described
earlier, an attacker can spoof the identity of the HMU
for the backend server and vice-versa. This means
that an adversary can have full control over the in-
formation that is sent between these two entities. In
order to target a patient an attacker could for instance
constantly send good reports, suppressing any alerts
or warnings from the pacemaker. This could trick a
clinician into thinking that the patient is doing great
while in reality, the patient might be in urgent need of
a check-up, for example, due to the pacemaker battery
running out. Having an HMU would thus be more
dangerous than having no home monitoring enabled,
due to a false sense of security and potentially fewer
clinic visits.
Experimental Security Analysis of Connected Pacemakers
41

Figure 5: Attack tree for the “Unauthorized access to the
backend server” scenario.
The second scenario can be described as Unautho-
rized access to the backend server and is presented in
Figure 5. We believe that this is possible with both
versions of the HMU, given that the attacker can ac-
cess credentials that are still valid. The attack tree is
only showing the GSM attack tree, the attack tree for
the T-Line would be similar but easier since it only
requires a working telephone line and no valid PIN
or SIM. If an attacker can access the Virtual Private
Network (VPN) with their computer using the cre-
dentials of the HMU, they would have direct access
to the backend server (and all machines that reside in
the same private network unless proper network seg-
mentation with security monitoring is in place). If any
of these machines are compromised, the result could
be a significant data leak of personal data. Second-
hand HMUs can be bought for a very low price on the
internet, some come with their SIM cards still valid as
we have demonstrated in our research, thus enabling
an attacker to perform such an attack.
5 DISCUSSION
5.1 Results from the Security Analysis
Our research confirms what was highlighted by Rios
and Butts: the industry is overall still quite immature
when it comes to cybersecurity Rios and Butts (2017).
Indeed, from a hardware point of view, an attacker
with physical access to a device can easily get access
to patients’ data with no need for extensive knowledge
or expensive equipment. From our observations, best
security practices were not applied when it comes to
hardware security given our findings of vulnerabilities
that can all be described as commonly found in em-
bedded devices. From a network perspective, several
weaknesses have been identified in the protocol that
is used by the HMU to communicate with the back-
end server, such as the credentials sent in clear text
over TCP, the usage of a weak cipher to send data us-
ing SMS or the lack of mutual authentication in the
second version of the HMU.
On balance, it is also important to highlight
that there is a notable evolution in terms of secu-
rity between the versions. The latest version of the
HMU seems to implement mutual authentication and
stronger cryptographic ciphers than the previous ver-
sions. We can also point out that even though the
second version has been found to have several weak-
nesses and vulnerabilities, the telemetry data was al-
ready encrypted using AES CBC with the keys being
randomly generated and unique per device.
5.2 On the Trade-offs in the Medical
Industry
When designing IMDs, there are several security ob-
jectives to have in mind. These are the regular six
following properties: Confidentiality, Integrity, Avail-
ability, Non-repudiation, Authorization and Authen-
tication. One also needs to consider the two modes
under which these security properties have to be
respected: normal operation mode and emergency
mode. In the normal operation mode, the patient is in
a state where it is reasonable to assume strict control
of which devices can interact with the IMD, and it is
feasible to implement strong access control, through
the mean of cryptographic protocols for instance. Ca-
mara et al. explain that ideally, the device should not
be detectable by unauthorized parties in this mode,
and should “ignore data requests or device repro-
gramming commands” Camara et al. (2015). In emer-
gency mode, even though the previously mentioned
security objectives are important, it is vital that the
device be accessible, for example if the patient is to
undergo an emergency procedure for which the pace-
maker must be deactivated.
It is thus a challenge for manufacturers to develop
devices that fulfill all these characteristics. Zheng et
al. highlight the trade-offs that come with the pace-
maker ecosystem Zheng et al. (2017). The first one
is related to the emergency mode: security vs acces-
sibility. Indeed, the pacemaker purpose is to save
the patient’s life and should not be an obstacle dur-
ing an emergency surgery. The second trade-off is,
emergency access vs secure checkup access. Secur-
ing the regular access while having an emergency ac-
cess, which is almost like a security backdoor, is a
challenge, especially when one must also take into
account the battery life of the device. This leads to
BIODEVICES 2022 - 15th International Conference on Biomedical Electronics and Devices
42

the third trade-off which is limited resources vs strong
cryptography. Indeed, to secure the device, one need
to implement strong cryptography which require in-
tense processing power, this conflicts with the with
low power capabilities and the long battery life time
required by the implanted devices. This can even be
abused by an attacker that launches Denial of Service
(DoS) attacks in the form of constant wireless com-
munication requests to draw the device battery, lead-
ing to a premature pacemaker battery depletion which
requires surgery and thus setting the patient’s life at
higher risk from complications.
5.3 Mitigations & Defense Mechanisms
As mentioned in the previous section, building safe
and secure medical devices means facing several
trade-offs. Several solutions have been proposed to
solve the problem of having a secure access to the de-
vice while allowing access in emergency situations.
Zheng et al. wrote a review Zheng et al. (2016) of the
different mechanisms that could be used:
External Proxy-based Solutions. This idea was first
proposed by Denning et al., and consists, as the name
indicates, in having an external device called the
Communication Cloakers to protect the implant Den-
ning et al. (2008). This external device is caried by the
patient and protects the implant from attacks in the
everyday life. In an emergency situation, when the
clinician doesn’t have access to the distributed key,
they can simply remove the proxy. However, this also
means that if patients forget or lose their proxy device,
their implant becomes vulnerable to attacks again.
Biometric-based Access Control. This type of solu-
tions uses patients’ biometric features in order to pro-
vide access. For instance, the Heart-to-Heart (H2H)
scheme Rostami et al. (2013) makes sure that the
pacemaker can only be accessed by a programmer in
physical contact with the patient by using ECG sig-
nals to generate the crypto material to establish a se-
cure wireless communication. Other solutions might
use different biometric features, such as fingerprints,
iris or even voice Zheng et al. (2018).
Proximity-based Security Schemes. In these
schemes, the proximity of the device is used to
determine whether or not a functionality is available.
For instance, changing the device settings, which
is a critical operation, requires close proximity (a
few centimeters) while home monitoring is allowed
up to 10m. If some authentication scheme such as
Ultrasonic-AC Rasmussen et al. (2009) combine
proximity and security credentials, others can be
based on magnetic fields or short-range communica-
tion protocol. This is in fact what is currently used to
secure pacemakers. It has however been proven to be
vulnerable if the attacker uses strong magnetic fields
or simply use powerful and sensitive transceivers and
high gain antennas Marin et al. (2016).
Key Distribution Supporting Emergency Access.
These schemes rely on cryptography to achieve
secure access in normal situations while also keeping
an emergency access. This includes symmetric
cryptography, in which the key is distributed to
authorized devices. For emergency situations, it is
proposed that the key is carried by the patient, either
with a smart card, on a bracelet or simply tattooed
on the skin (with UV ink for instance) Schechter
(2010). Public key cryptography can also be used.
However, in the case of an emergency situation,
the programmer needs to contact a trusted party
to obtain the certificate that can be used to derive
a symmetric key, and this requires access to the
Internet. In addition, public key cryptography is not
compatible with the low energy requirements of the
pacemakers. Finally, it is possible to use biometric
features to generate keys, as already explained for
biometric-based solutions.
In their review, Zheng et al. also suggest possi-
ble solutions to address the resource constraints of
IMDs Zheng et al. (2016).
Lightweight Cryptography. In order to preserve
the implant energy, manufacturers need to use
lightweight cryptography protocols. Marin et al. pro-
pose a key agreement protocol that is an alternative to
the proposal of Halperin et al., that was to add a stan-
dard symmetric key authentication and encryption be-
tween the ICD and the programmer, thus requiring the
key to be safely stored on the programmer and open-
ing the door to it being leaked. Marin et al. propose
a semi-offline protocol: the IMD is in charge of com-
puting a new key for the new period. To do so, the
programmers need to contact the vendor to obtain the
key for the period. That way, if the programmer is
lost, or not in use anymore, it will not receive any
updated key, and thus the ecosystem goes back to a
secure state when the key is changed. Even though
the new key computation is expensive for the IMD,
this is a rare event and is thus not a problem.
Energy Harvesting. Another way to protect medical
devices is through energy harvesting. Halperin et al.
propose zero-power defenses for IMDs. These de-
fenses includes detection of attacks, prevention of at-
tacks and a key exchange mechanism. As a detection
mechanism, they propose to add a way to make the
patient aware that there is something out of the or-
dinary happening, by for instance playing a “beep”
Experimental Security Analysis of Connected Pacemakers
43

if the security is disabled on the implant. The zero-
power idea is to use a piezo-element driven by wire-
less communication (thus alerting a patient that wire-
less communication is happening).
Separate Security Unit. Last but not least, the usage
of a separate security unit that would be in charge of
the security can mitigate the impact on the battery of
the implant. This is for instance something that can be
pushed to the external proxy device proposed above.
Moving away from the communication channel,
another area that needs improvements is the software
security. Li et al. propose a way to improve the trust-
worthiness of medical device software with formal
verification methods Li et al. (2013). They applied
their approach to the firmware of a pacemaker and
“demonstrated its ability to detect a range of software
vulnerabilities that compromise security and safety.”
The idea behind formal verification is not only to
check for common vulnerabilities such as buffer over-
flows, use after free, etc. but also to go from the de-
vice specifications to verifiable properties. This can
be for example the voltage of the pacing for a pace-
maker in a given configuration. This approach allows
to verify real-world properties.
The healthcare domain has recently been plagued
with cyber attacks in the form of ransomware attacks,
where the intrusion often comes as a result of poor
practices related to software patching and software
inventory management. One mitigation that might
help IT staff in deciding which software security up-
dates that needs to be applied for securing medical
devices is the introduction of a Software Bill of Ma-
terials (SBOM), where the manufacturer declares all
software components in a device. In 2018 the FDA
published a Medical Device Safety Action Plan where
one of the proposed actions was to require medical
device manufacturers to include an SBOM as part of
their premarket submissions.
Securing devices to which an attacker might have
physical access is hard. As mentioned in the Mi-
crosoft’s Ten immutable Laws of Security, “If a bad
guy has unrestricted physical access to your com-
puter, it’s not your computer anymore.” This is even
more true for embedded medical devices, which usu-
ally do not come with as strong security defense
mechanisms as computers. Indeed, adding strong
hardware security to medical devices such as the
Home Monitoring Unit also has a cost, and manufac-
turers might have to make a choice between security
and costs, given that the money that is invested in the
security of an HMU is not used for developing treat-
ment functionality, which saves lives. In addition to
this, there is also the race to market and the strict cer-
tification process that does not allow to easily make
changes to an already approved design.
The industry is unfortunately not yet at the point
where we can expect very strong cyber security in
medical devices. As demonstrated by our research,
basic security practices remains to be applied. A
first step towards a more secure pacemaker ecosystem
is the implementation of well-known best practices
for hardware security, which, if they will not protect
against all attackers, can surely raise the cost of an at-
tack, and simply discourage many attackers. Guides
such the Secure Design Best Practice Guide by the
IoT Security Foundation IoT (2020) gives a checklist
of security measures to be adapted to a product, al-
ready during the design phase. When it comes to se-
curing the firmware, the OWASP foundations offers a
project for Embedded Application Security OWASP
(2020) that should be taken into account.
6 CONCLUSION
In this paper, we presented the results of our research
regarding the security of the pacemaker ecosystem of
the medical device manufacturer BIOTRONIK, and
the evolution of the security between the different ver-
sions of their Home Monitoring Units. We analyzed
different versions of the devices and discovered vul-
nerabilities in all of them. While we confirm that the
medical device manufacturing industry is still imma-
ture when it comes to the implementation of hardware
security, we also point out that there is an evolution
towards a safer ecosystem. We noticed improvements
in the protocol used to communicate with the back-
end infrastructure between the older and newer gen-
erations of devices. Our findings were reported to the
vendor in a coordinated vulnerability disclosure pro-
cess, resulting in an official security advisory, and will
hopefully be used as input to improving the security
of future devices.
ACKNOWLEDGEMENTS
We would like to thank Anniken Wium Lie with whom
we collaborated on the network aspects of the project.
We very much appreciate the contributions of Éireann
Leverett that did some of the initial hardware testing
to discover the HMU debug interfaces. Finally, we
are grateful to Snorre Aunet and Ingulf Helland from
NTNU who took time to help us solder a connector
on the HMU.
This work was partially funded by Reinforcing
the Health Data Infrastructure in Mobility and As-
BIODEVICES 2022 - 15th International Conference on Biomedical Electronics and Devices
44

surance through Data Democratization, a five-year
project (grant number 28885) under the Norwegian
IKTPLUSS-IKT and Digital Innovation programme.
The authors gratefully acknowledge the financial sup-
port from the Research Council of Norway.
REFERENCES
Block, C. C. (2016). Muddy waters report - st. jude medical,
inc. Technical report, Muddy Waters Capital LLC.
Bour, G. N. (2019). Security analysis of the pacemaker
home monitoring unit: A blackbox approach. Mas-
ter’s thesis, NTNU.
Camara, C., Peris-Lopez, P., and Tapiador, J. E. (2015). Se-
curity and privacy issues in implantable medical de-
vices: A comprehensive survey. Journal of biomedi-
cal informatics, 55:272–289.
CISA (2020). ICS Medical Advisory (ICSMA-20-
170-05). https://us-cert.cisa.gov/ics/advisories/
icsma-20-170-05. [Online; accessed 30-Sep-2021].
Denning, T., Fu, K., and Kohno, T. (2008). Absence makes
the heart grow fonder: New directions for implantable
medical device security. In HotSec.
Halperin, D., Heydt-Benjamin, T. S., Ransford, B., Clark,
S. S., Defend, B., Morgan, W., Fu, K., Kohno, T., and
Maisel, W. H. (2008). Pacemakers and implantable
cardiac defibrillators: Software radio attacks and zero-
power defenses. In 2008 IEEE Symposium on Security
and Privacy (sp 2008), pages 129–142. IEEE.
IoT (2020). Secure design best practice guide. [Online].
Justis- og beredskapsdepartementet, Helse- og omsorgsde-
partementet (2005). Forskrift om medisinsk utstyr.
https://lovdata.no/dokument/SF/forskrift/
2005-12-15-1690/%2FT1%2Ftextsection1-5#/T1/
textsection1-5.
Li, C., Raghunathan, A., and Jha, N. K. (2013). Improving
the trustworthiness of medical device software with
formal verification methods. IEEE Embedded Systems
Letters, 5(3):50–53.
Marin, E., Singelée, D., Garcia, F. D., Chothia, T., Willems,
R., and Preneel, B. (2016). On the (in) security of
the latest generation implantable cardiac defibrillators
and how to secure them. In Proceedings of the 32nd
annual conference on computer security applications,
pages 226–236.
OWASP (2020). OWASP embedded application security.
[Online].
Rasmussen, K. B., Castelluccia, C., Heydt-Benjamin, T. S.,
and Capkun, S. (2009). Proximity-based access con-
trol for implantable medical devices. In Proceedings
of the 16th ACM conference on Computer and com-
munications security, pages 410–419.
Richards, R. (2015). Healthcare data breaches cost $6 bil-
lion a year (infographic)t. [Online; posted 16 Novem-
ber 2015].
Rios, B. and Butts, J. (2017). Security evaluation of the
implantable cardiac device ecosystem architecture and
implementation interdependencies.
Rostami, M., Juels, A., and Koushanfar, F. (2013). Heart-
to-heart (h2h) authentication for implanted medical
devices. In Proceedings of the 2013 ACM SIGSAC
conference on Computer & communications security,
pages 1099–1112.
Savci, H. S., Sula, A., Wang, Z., Dogan, N. S., and Ar-
vas, E. (2005). Mics transceivers: regulatory stan-
dards and applications [medical implant communica-
tions service]. In Proceedings. IEEE SoutheastCon,
2005., pages 179–182. IEEE.
Schechter, S. (2010). Security that is meant to be skin
deep using ultraviolet micropigmentation to store
emergency-access keys for implantable medical de-
vices.
Zheng, G., Shankaran, R., Orgun, M. A., Qiao, L., and
Saleem, K. (2016). Ideas and challenges for secur-
ing wireless implantable medical devices: A review.
IEEE Sensors Journal, 17(3):562–576.
Zheng, G., Yang, W., Valli, C., Qiao, L., Shankaran, R.,
Orgun, M. A., and Mukhopadhyay, S. C. (2018).
Finger-to-heart (f2h): Authentication for wireless im-
plantable medical devices. IEEE journal of biomedi-
cal and health informatics, 23(4):1546–1557.
Zheng, G., Zhang, G., Yang, W., Valli, C., Shankaran, R.,
and Orgun, M. A. (2017). From wannacry to wan-
nadie: Security trade-offs and design for implantable
medical devices. In 2017 17th International Sympo-
sium on Communications and Information Technolo-
gies (ISCIT), pages 1–5. IEEE.
Experimental Security Analysis of Connected Pacemakers
45
