
The Role of Data in Crisis Management Models in the Health Care
Context
Hannele Väyrynen
a
, Annamaija Paunu and Nina Helander
b
Information and Knowledge Management, Tampere University, Tampere, Finland
Keywords: Data, Crisis Management, Crisis Management Model, Information Technology, Health Care.
Abstract: Successful crisis management is consisted of different factors, varying actors and operation environments.
Health care system is one of the most critical sectors in societies to operate also in a crisis situation. In the
middle of a crisis, digitalization and access to data can have an important role as an enabler. In this paper, the
role of data in crisis management models in health care context is studied. The theoretical frame is derived
from the crisis management literature review. The study is able to identify the role of data in seven critical
elements in crisis management models that need consideration during crisis, namely data has supporting,
enabling as well as critical role in technology, strategy, government, adaptation mechanisms, scenarios,
security of supply chain and co-operation in crisis management. As a result of the study, different aspects of
data in promoting successful crisis management are proposed.
1 INTRODUCTION
There are different kind of crises such as economic,
war, natural disaster, health, technological and
human-made crisis to mention just a few. Crises can
be described through three elements: depth, duration
and resilience (Maritsa and Kalemis, 2020). We live
in a constant cycle of various crises and we need to
prepare, adjust, manage and learn from crises. Thus,
crisis management (CM) is very much needed
throughout different sectors of society. However,
different CM strategies and models are needed for
different crises (Khodarahmi, 2009).
In a crisis, it needs also to be considered that
different stakeholders (Shallmo and Williams, 2020)
have to explore several environments around them in
order to build a situational picture: political,
economic and social environments, technology,
health and science and international relationships (Li
et al., 2021). This kind of building of a situational
picture requires access to relevant data.
Health care systems are one of the most critical
sectors in societies being a solid foundation for daily
life (Keskimäki et al., 2019). In a crisis, situations are
resolved with ad hoc solutions causing complex
networks of a complex of human-technology mixture
a
https://orcid.org/0000-0002-3636-280X
b
https://orcid.org/0000-0003-2201-6444
(Bakos 2020). There may be signals for sudden crisis
and the preparedness and resilience to shocks of
health systems vary (European Observatory on
Health Systems and Policies, 2020).
Previous research has acknowledged the crucial
role of information technology in successful CM in
the health care context. Difficulties during the
management of emergencies and crisis are most often
related to proper information management, as
relevant and adequate data is needed promptly for the
decision makers. Information technology (IT) can
provide useful tools to ensure access to data, but we
also need to gain a proper understanding of the real
needs for information in the middle of a crisis,
existing information exchange practices, and ways of
communication in the stakeholders’ society (Wybo
and Lonka, 2003Telemedicine has enabled virtual
care and emergency consultation (Hollander and
Carr, 2020) although the role of telecare may still be
unclear (Singh et al., 2021).
Digitalization offers opportunities in CM
(Reeves et al., 2020; Gkeredakis et al., 2021);
however benefits are not actualized in the crisis
situations in health care context in an optimal way,
e.g. too few platforms or too little data utilization is
(Schofield et al., 2019) or challenges in IT integration
Väyrynen, H., Paunu, A. and Helander, N.
The Role of Data in Crisis Management Models in the Health Care Context.
DOI: 10.5220/0011589500003335
In Proceedings of the 14th International Joint Conference on Knowledge Discovery, Knowledge Engineering and Knowledge Management (IC3K 2022) - Volume 1: KDIR, pages 337-344
ISBN: 978-989-758-614-9; ISSN: 2184-3228
Copyright
c
2022 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
337

or data quality and cooperation of professionals
regarding the data face challenges (Hong et al., 2020).
During the 2020-2021 CORONA-19 crisis, different
strategies in health care were incentivized. However,
there is a need for strategy as long-term planning has
been identified as promoting health care digital
transformation and crisis anticipation (Pérez Sust et
al., 2020) and continuous anticipation to manage
complexity and investments in human resources
(ESPAS 2015).
IT and the available data can support health care
personnel in their daily work, enable supply chain
management, ensure health care financing with
effeciency processes, and produce transparent
processes for the governance and service delivery
(Otto et al. 2015). Concerning the practical
infrastructure level, transportation, power and water
network, internal and external organization
communication systems, and crucial supplies like
oxygen, blood, medical equipments, and medication
are subject to technological reliability (Zhao et al.,
2019). All these functions produce fragmented data
and technology platforms are one way to unify
scattered data and information (Cimellaro et al,
2018).
However, data as such is not valuable but has to
be transformed into understandable information that
brings some value to the recipient. It has been said
that “healthcare is undergoing a data revolution”
(Panesar 2019). Inreasingly, real-time data analysis to
create predictive modeling during the crisis has
supported the mitigation of risks (Mensah et al., 2015;
Lo Sardo et al., 2019). The challenges of data
utilization culminate in unintegrated information
management systems or non-syncretized data
formulating barriers for data and information
exchange between institutions (Liapiz et al. 2015).
The challenges of health-care informatics were
identified nearly twenty years ago (Guah, 2004) and
the same stumbling blocks still exist. Beside
technology solutions, the management of information
is needed as well (Bose, 2003).
In this paper the aim is to study the role of data in
CM. The paper describes key elements of CM models
and the role of data in them in health care context and
seeks answers to the following research question:
What is the role of data in successful CM in health
care?
The article proceeds as follows: after this
introductory section the theoretical bases of data and
crisis management are presented after which the
methodology part of the literature review is
described. The fourth section presents the main
results followed by the conclusions in the last section
with suggested avenues for future research.
2 THEORETICAL BASES OF
DATA AND CM
Crisis management is composed of different factors,
and has been called a “multi-faceted crisis response
mechanism” (Liapis et al., 2015), thus it requires
multidisciplinary examination (Pearson and Clair,
1998). Crisis management models are designed and
planned to prepare for a crisis and act as
prespecifications or guidance of how to operate.
There are examples of models that focus, e.g.
information exchange (Shooley et al., 2014), effects
on the economy (Estrada and Arturo, 2020), strategy
(Radonjic-Simic et al. 2021), infrastructure (Mihai,
2020), technical efficiency (Ortega-Díaz et al., 2020),
education (Estrada and Arturo, 2020) or signal
detection, prevention and preparedness, damage
limitation, recovery and learning (Pearson and
Mitroff, 1993).
In general, several challenges have been identified
in the literature related to the use of data and
information technology. There are challenges related
to poor quality of data leading to potential
misinterpretations, problems with information
systems, rigid processes, strict legislation and
resource challenges (Vuori et al., 2019). Typically
difficulties can also exist in accessing relevant
information (finding the right documents or
databases) due to the lack of sufficient employee
training, as people do not have the skills to search for
the right information (Corallo et al., 2012).
All of these challenges are also typical for health
data, but there are some special characteristics that
potentially hinder the usage of health data. First,
health data is characterized by highly confidential
personal health data leading to the challenge of
securing the privacy of health data. Second, other
challenges related to the use of health data are related
to the heterogeneity of the data sources,
interoperability between different IT systems and the
fragmentation and strictness of regulatory
frameworks. (OECD, 2015)
3 RESEARCH SETTING
The applied research methodology was a scoping
literature review. The review was selected to provide
valuable information about the topic for both
KDIR 2022 - 14th International Conference on Knowledge Discovery and Information Retrieval
338
academia and business (Tranfield et al. 2003). The
databases used for the literature search were Web of
Science, Scopus and Ebsco. The time horizon was
2009-2021 because health care technology as well as
data science developed rapidly during this decade. To
get a more general picture of the literature, crisis
management was considered with the concepts of
health AND data; and crisis AND management AND
model.
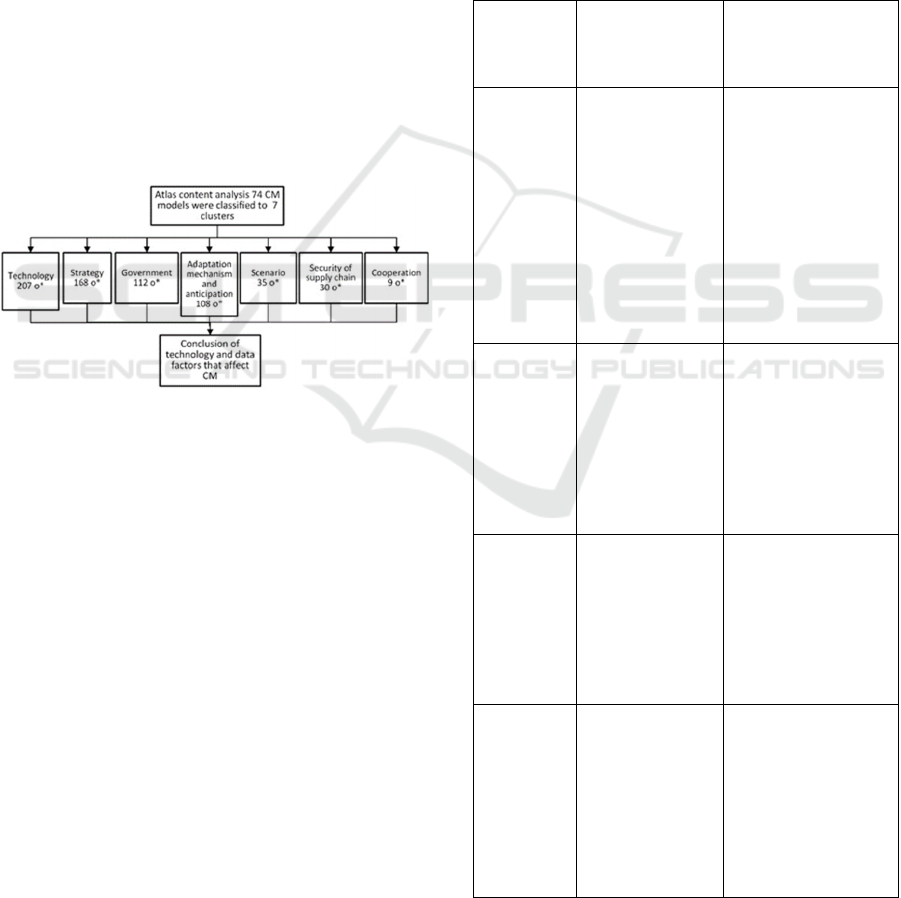
In the first phase of the literature review, a total of
633 articles were identified and furthermore,
altogether 74 CM models were identified from these
articles. Altogether these 74 identified CM model
papers were further analysed using the Atlas content
analysis program to code the content into clusters.
Atlas is the qualitative data analysis and research
software to analyse the content of the selected
literature and cluster the themes (Atlas 2022).
Altogether seven clusters were identified and the role
of data in these clusters were further identified. Figure
1 illustrates these phases of the literature review and
analysis.
Figure 1: Illustration of the research method process
(o* = occurrence of articles).
4 RESULTS
Different CM models can guide the stakeholders to
co-operate with other agents and institutions (Li, e.g.,
2021). A policy framework for technology and data
utilization is needed, and a crisis situation may push
policy development and reformulation of operational
strategies (Kuščer et al., 2022) as well as data
collection and communication planning (Barkbook-
Johnson et al., 2017). Open-source software for data
exchange and co-operation in a crisis is one way to
advance situational picture formulation and problem
solving (Falenski et al., 2013).
More advanced data utilization in crises enables
data-aided predictive modelling and scenario analysis
for environment change forecasting and pandemic
crisis, for example (Danesh-Yazdi and Aiei-Ashtiani,
2019). Big data analysis is used to support multi-
criteria decision-making processes in crisis
management with estimation and evaluation
techniques (Ersoy and Alberto, 2019; Alkahami et al.,
2020) and to study the effect of crises on business
management (Chen and Biswas, 2021). One critical
factor is security of supply chain and resource
management, and pandemic big data can navigate
optimal resourcing in a crisis (Bag et al., 2021; Das et
al., 2022).
Next, the key findings are listed in Table 1,
showing the role of data in CM that need to be
critically considered.
Table 1: Summary of the role of data in empirical findings.
Critical
element
Effect factors that
need to be ensured
in CM
Role of data in
promoting successful
CM
Technology
• Remote care
functionality and
efficiency
• Medical device
usage
• Sensor data,
network between
sensors and IT
• Dashboard with
real-time data
• Human-robotics
interaction
• Data policy
• Real time data and
information,
minimum level of
information
blackouts
• Big data analysis
• Facilitate decision
making
• Human-technology,
human-robotics in
o
p
eration
Strategy
• Systematic data
generation
• Communication
strategy
• Education
programs
• Information for
providers and policy
makers
• Analyses how the
system responds
• Simulation of
damage scenarios
and alternative
strate
gy
testin
g
Government
• Guidance means
for data and
technology
utilization in
services
• IT and data policy
• Produce data and
information for
decision makers to
prepare legislative
enablers
• Health and rescue
clinical governance
Adaptation
mechanisms
• Health IT
acceptance
• Platform for
health and
government
actors
• Virtual
interaction
• Education
• Transparent
information on
technology
implementation
processes
• Health care
professional
education provides
civic resilience
The Role of Data in Crisis Management Models in the Health Care Context
339
Table 1: Summary of the role of data in empirical findings
(cont.).
Critical
element
Effect factors that
need to be ensured
in CM
Role of data in
promoting successful
CM
Scenarios
• Prevention and
recovery
• Simulation (live,
agent based
computer, virtual
reality)
• Systematic
databased
evaluation for the
situational
picture
• Machine learning
in scenario
develo
p
ment
• Tools for data
analysis and KM
tools for evaluation
• Data mining
techniques
• CM information
literacy
• Situational picture
formation
Supply
chain
• Integration of
different
technologies
(e.g.,
transportation
• Goods and
service delivery
• Resource and
inventory
management
• Multimodal
communication
technology that
enables risk
management and
decision making
• Health and clinical
management
• Absorbing best
solutions and
practices
from other industries
• Identification new
problems
• Network
mana
g
ement
Co-operation
• Collaboration
processes among
health care
industry
stakeholders
• Strategy,
operation, and
innovations for
prevention of
crisis effects
• Shared knowledge
and other resources
• National and global
knowledge sharing
between
professionals
• Complexity control
• E-learning.
Nutley et al.’s (2014) decision making model for
health data context addresses “behavioral, technical,
and organizational constraints to data use” to support
decision making. These data related factors proposed
by Nutley et al. (2014) were also present in the CM
models analysed in this paper. For example, the data
infrastructure factor revealed that technology is
already smart, but technology utilization may be
challenging. There are many technological systems,
solutions and applications with several measuring and
controlling means (e.g., sensors, internet of things
IoT, wireless technology) in health care. However,
connecting the different IT systems e.g. between
different hospitals, rescue services or transportation is
not an easy task. Integration of the IT systems
internally in a hospital is challenging e.g. because the
challenge of data interoperability. Even a simple
digital application utilization requires a health care
ecosystem around it: the manufacturer of the
platform, the equipment service or device provider,
and furthermore, an ecosystem for the
communications, e.g., the telecommunications
infrastructure provider and the institution (Jeong and
Shin, 2016). However, when integration is successful,
the literature results show that communication can be
strengthened and real time data made possible, e.g.,
by sensors and IoT (ibid.); but successful
communication either via technology or humans
requires strong cooperation (Sentell et al., 2019).
Technology utilization and the benefits obtained from
the technology solution need to be “sold” to the actors
to be implemented. It is important to identify how the
benefits occur in practice, at the different levels, e.g.,
at state level, corporation, profession or family and
individual level (Oborn et al., 2021).
Furthermore, the factor of data availability faces
similar challenge to infrastructure, i.e., how to obtain
integrated data. Different solutions produce data, but
it is another matter whether the actors have access to
the data or whether the data is usable (Lenert, 2012).
The literature covers information management in data
availability in more general terms than just in a crisis
context, often in the knowledge management (KM)
context (Alhuwail, 2021; Thye et al., 2020.) Although
the data sources can provide valuable information for
the actors in the crisis (Shooley et al., 2014) what kind
of means and possibilities there are for data exchange
between institutions. Access to a certain data source
(e.g. geographic information) is possible in one
industry while surprisingly, in another industry
(health care sector) access is rejected.
From this we reach data policy factor; data
availability and data policy should go hand in hand to
secure appropriate data and information usage as well
as enabling data. Platforms, data and information
usage need policy and protection methods and clear
guidelines on how to utilize and document them
(Tang et al., 2011; Shi, 2020). Moreover, the data
quality factor raises discussion of the challenges of
data or integration of other data sources. Therefore
again, in a wider national and operation context,
guidelines and data sharing programs and
standardization for data management are needed.
Data is an ever-changing resource and data
development and suitable technology solutions are
KDIR 2022 - 14th International Conference on Knowledge Discovery and Information Retrieval
340

essential to optimize data utilization as well as a
necessary part of CM. (Alhuwail, 2021) However,
data and information are useless until they are
utilized. CM models can advise the actors to adopt
technology solutions under pressure due to a crisis (Li
et al., 2021).
5 CONCLUSIONS
The previous literature has stated that the benefits of
information technology are not being actualized in
health care in optimal manner even though advances
e.g., in IT integration and AI and machine learning in
data analysis have a lot of potential (Hong et al.,
2020). The aim of this paper was to study the role of
data in the CM in health care context through a
literature review.
Altogether 74 different CM models were
identified from the literature and clustering seven key
elements: technology, strategy, government,
adaptation mechanisms, scenarios, security of supply
chain and co-operation. Data has an important role in
every other element as an enabler in crisis operation.
In successful CM in health care, real-time
information sharing between multiple actors and
organizations is essential to formulate the situational
picture (e.g., Ross Ashley, 2003). Furthermore, data
was identified as playing a supporting role; with new
or innovative technological solutions for the crisis
operation and data utilization, guiding strategy
modification of what needs to be done in a changing
situation and how technology could be utilized. Data
has also a critical role in formulating governmental
actions (data policy or data production for decision
makers), enabling information transparency, and
providing tools for education and leadership. Most
importantly, IT and modern digital solutions are
needed to gather, process, and share data to enable the
scenario and situational picture formulation in a
crisis. One critical area to ensure is the supply chain
and IT offers means of communication and network
management tools to enable essential national and
international co-operation in a crisis with knowledge
sharing.
Governmental actions are needed (legislation,
public-private data or platform sharing) to support the
health care transformation to survive in crisis
situations and to gain the benefits of innovative
technologies, such as AI and machine learning for
data analytics (Mahmood et al., 2020). Human-
technology interaction is an emerging trend in crisis
operations; however, it clearly needs a social
approach besides technology, such as change of
attitudes and education to promote competence for
technology utilization (Sentell et al., 2021) as well as
equality in access e.g. to virtual care services
(Schofield et al., 2019). New management models
and strategy development are also needed to turn a
crisis into an asset (Pérez Sust et al., 2020).
Although this paper managed to give a review, it
has some limitations. First, the data set was gathered
from a limited search engine and does not capture the
scholarly literature comprehensively. Secondly, there
are many excellent examples of data utilization and
technology innovations produced in a crisis
operational environment that merit additional reviews
in the future.
Further study of the role of data and information
exchange (Vujadinovic, 2020) would be especially
interesting. Cyber security was excluded from this
study and, when considering digital platforms, data
and medical applications, and data exchange, security
issues are an important research topic. Third potential
research avenue for IT and CM are simulations in
crisis. Simulations offer a tool for evaluating different
emergency plans and communication technologies
during a crisis.
ACKNOWLEDGEMENTS
This work is a part of the RECPHEALS project,
funded by Academy of Finland, Special funding for
research into crisis preparedness and security of
supply.
REFERENCES
Alhuwail, D. (2021). Information management practices in
public tertiary health-care facilities: an empirical
investigation from the state of Kuwait. Records
Management Journal, 31(1), 60-73.
Alkahami, W., Baz, A., Alkahami, H., Pandey, A., & Khan,
R. (2020). Symmetrical model of smart healthcare data
management: A cybernetics perspective. Summetry,
12(2), 1-16.
Al-Wesabi, F., Alsolai, H., Hilal, A., Hamza, M.,
Duhayyim, M., & Negm, N. (2022). Machine learning
based depression, anxiety, and stress predictive model
during COVID-19 crisis. Computers, Materials and
Continua, 70(3), 5803-5820.
Atlas 2022. Accelerate your research with the best
systematic literature review tools. Available: Literature
Review Tools - ATLAS.ti. Retrieved 3.9.2022.
Bag, S., Dhamija, P., Luthra, S., & Huisingh, D. (2021).
How big data analytics can help manufacturing
companies strengthen supply chain resilience in the
The Role of Data in Crisis Management Models in the Health Care Context
341

context of the COVID-19 pandemic. International
Journal of Logistics Management, 24 p.
Bakos, L. (2020). Knowledge Management Issues During
Organizational Crisis: How Human-Machine
Communication Helps. In A. E. Wensley (Ed),
Proceedings of the 17th International Conference on
Intellectual Capital, Knowledge Management and
Organisational Learning, 37-44. ICICKM 2020.
Barkbook-Johnson, P., Badham, J., & Gilbert, N. (2017).
Uses of agent-based modeling for health
communications: The TELLME case study. Health
Communications, 32(8), 939-944.
Bose, R. (2003). Knowledge management-enabled health
care management systems: capabilities, infrastructure,
and desicion-support. Expert Systems with
Applications, 24(1), 59-71.
Chen, Y., & Biswas, M. (2021). Turning crisis into
opportunities: How a firm can enrich its business
operations using artificial intelligence and big data
during covid-19. Sustainability (Switzerland), 13(22),
17 p.
Cimellaro, G., Malavisi, M., & Mahin, S. (2018). Factor
Analysis to Evaluate Hospital Resilience. Asce-Asme
Journal of Risk and Uncertainty in Engineering
Systems Par a-Civil Engineering, 4(1), 04018002.
Corallo, A., Lazoi, M., & Secundo, G. (2012). Inter-
organizational knowledge integration in Collaborative
NPD projects: evidence from the aerospace industry.
Knowledge Management Research & Practice, 10(4),
354-367.
Danesh-Yazdi, M., & Aaie-Ashtiani, B. (2019). Lake urmia
crisis and restoration plan: Planning without
appropriate data and model is gambling. Journal of
Hydrology, (576), 639-651.
Das, D., Nag, S., Naskar, H., Acharya, S., Bakchi, S., Ali,
S., Tudu, B. (2022). Personal protective equipment for
COVID-19: A comprehensive review. EAI/Springer
Innovations in Communication and Computing, 141-
154.
Deutsch, E., Dong, Y., Halamek, L., Rosen, M., Taekman,
J., & Rise, J. (2016). Leveraging Health Care
Simulation Technology for Human Factors Research:
Closing the Gap Between Lab and Bedside. Human
Factors, 58(7), 1082-1095.
El-jardali, F., Bou-Karroum, L., & Fadlallah, R. (2020).
Amplifying the role of knowledge translation platforms
in the COVID-19 pandemic response. Health Res
Policy Sys, 18(58), 7p.
Ersoy, A., & Alberto, K. (2019). Understanding urban
infrastructure via big data: The case of belo horizonte.
Regional Studies, Regional Science, 6(1), 374-379.
ESPAS. (2015). Global Trends to 2030: Can the EU meet
the challenges ahead? Luxemburg: EU.
Estrada, R., & Anturo, M. (2020). A Post-COVID-19
Economic Ecovery Model: The National Domestic
Economic Auto-Sustainability Model (NDEAS-
Model). AEI Insights, 7(1), 37-46.
European Observatory on Health Systems and Policies,
Thomas, S., Sagan, A., Larkin J., & CulysJ. (2020).
Strengthening health systems resilience: key concepts
and strategies. World Health Organization. Regional
Office for Europe 2020.
Falenski, A., Filter, M., Thöns, C., Weiser, A., Wigger, J.,
Davis, M., Käsbohrer, A. (2013). A generic opensource
software framework supporting scenario simulaitons in
bioterrorist crisis. Biosecurity and Bioterrorism, 11(1),
S134-S145.
Gkeredakis, M., Lifshitz-Assaf, H., & Barrett, M. (2021).
Crisis as opportunity, disruption and exposure:
Exploring emergent responses to crisis through digital
technology. Information and Organization, 31(1), 12 p.
Granlund, T., Vedenpää, J., Stirbu, V., & Mikkonen, T.
(2021). On Medical Device Cybersecurity Compliance
in EU. arXiv.
Guah, M. (2004). Today's health care demands knowledge
management strategy. 26th International Conference
on Information Technology Interfaces, . 461-467.
Hicks, C., & Petrosoniak, A. (2018). The Human Factor:
Optimizing Trauma Team Performance in Dynamic
Clinical Environments. Emerg Med Clin North Am.,
36(1), 1-17.
Hollander, J., & Carr, B. (2020). Virtually Perfect?
Telemedicine for Covid-19. New England Journal of
Medicine, 382(18), 1679-1681.
Hunsaker, B., & Knowles, J. (2021). Effective Innovation
Begins with Strategic Direction. MIT Sloan
Management Review. Assessed 28. 10 2021
https://sloanreview.mit.edu/article/effective-innovation
begins-with-strategic-direction/
Jeong, Y., & Shin, S. (ei pvm). An IoT health care service
model of a vehicle using implantable devices. Cluster
Computing, 21(1), 1059-1068.
Keskimäki, I., Tynkkynen, L., Reissel, E., Koivusalo, M.,
Syrjä, V., Vuorenkoski , L., Karanikolos, M. (2019).
Finland: Health system review. Health Systems in
Transition, 21(2), 1-166.
Khodarahmi, E. (2009). Crisis Management. Disaster
Prevention and Management, 18(5), 523-428.
Kuscer, K., Eichelberger, S., & Peters, M. (2022). Tourism
organizations’ responses to the COVID-19 pandemic:
An investigation of the lockdown period. Current
Issues in Tourism, 25(2), 247-260.
Lenert, L., & Sundwall, D. (2012). Public Health
Surveillance and Meaningful Use Regulations: A Crisis
of Opportunity. American Journal of Public Health, e1-
7.
Li, B., Zhang, T., Hua, N., & Wang, Y. (2021). A dynamic
model of crisis management from a stakeholders
perspective: The case of COVID-19 in China. Turism
Review, 76(4), 767-787.
Liapis, A., Kostaridis, A., Ramfos, A., Hall, I., DeGaetano,
A., Koutras, N., . . . Boustras, G. (2015). A Position
Paper on Improving Preparedness and Responce of
Health Services in Major Crises, 205-216. International
Conference on Information Systems for Crisis
Response and Management in Mediterranean
Countries.
Lo Sardo, D., Thurner, S., Songer, J., Dufschmid, G., Endel,
G., & Klimek, P. (ei pvm). Quatification of the
resilience of primary care networks by stress testing the
KDIR 2022 - 14th International Conference on Knowledge Discovery and Information Retrieval
342

health care system. Proceedings of the National
Academy of Sciences, 116(48), 23930-23935.
Loggins, R., Little, R., Mitchell, J., Sharkey, T., & Wallace,
W. (2019). CRISIS: Modeling the restoration of
interdependent civil and social infrastructure systems
following an extreme event. Hazards Review, 20(3).
Lopez, J., Setola, R., & Wolthusen, S. (Eds.) (2012).
Critical Infrastructure Protection. Advances in Critical
Infrastructure Protection: Information Infrastructure
Models, Analysis, and Defense. Heidelberg: Springer
Berlin.
Mahmood, S., Hasan, K., Carras, M., & Labrique, A.
(2020). Global Preparedness Against COVID-19: We
Must Leverage the Power of Digital Health. JMIR
Public Health Surveill , 6(2), e 18980.
Maritsa, E., & KalemisK. (2020). Leadership readiness in
crisis context: Health preservation through shared
knowledge. Leadership readiness in crisis context:
Health pre17th International Conference on
Intellectual Capital, Knowledge Management &
Organisational Learning, 11 p. ICICKM 2020.
Mensah, P., Merkuyev, Y., & Longo, F. (2015). Using ICT
in developing a resilient supply chain strategy.
Procedia Computer Science, 43, 101-108.
Mihai, F. (2020). Assessment of COVID-19 waste flows
during the emergency state in Romania and related
public health and environmental concerns.
International Journal of Environmental Research and
Public Health, 17(15), 1-18.
Nutley, T., Gnassou, L., Traore, M., Bosso, A., & Mullen,
S. (2014). Moving data off the shelf and into action: an
intervention to improve data-informed decision making
in Cote D'Ilvoire. Global Health Action, 7(1).
Oborn, E., Putievsky, N., Pilosof, N., Hinings, P., &
Zimlichman, E. (2021). Institutional logics and
innovation in times of crisis: Telemedicine as digital
‘PPE’. Information and Organization, 31(1), 8.
OECD. (2015). Health Data Governance: Privacy,
Monitoring and Recearch (OECD Health Policy
Studies). Paris: OECD Publishing.
Ortega-Diaz, M., Ocaña-Riola, R., Pérez-Romero, C., &
Martin-Martin, J. (2020). Multilevel analysis of the
relationship between ownership structure and technical
efficiency frontier in the spanish national health system
hospitals. International Journal of Environmental
Research and Public Health, 17(16), 1-19.
Otto, K., Shekar, M., Herbst, C., & Mohammed, R. (2015).
Information of Communication Technologies for
Health Systems Strengthening: Opportunities Criteria
for Successs, and Innovation for Africa and Beyond.
World Bank, Washington: World Bank.
Panesar, A. (2019). Machine Learning and AI in
Healthcare: Big Data for Improved Health Outcomes.
Berkeley, CA: Apress L. P.
Pearson, C., & Clair, J. (1998). Reframing Crisis
Management. The Academy of Management Review,
23(1), 59-76.
Pearson, C., & Mitroff, I. (1993). From Crisis Prone to
Crisis Prepared: A Framework for Crisis Management.
The Executive, 7
(1), 48-50.
Pérez Sust, P., Solans, O., Fajardo, J., Medina Peralta, M.,
Rodenas, P., Gebaldá, J., . . . Piera-Jimenez, J. (2020).
Turning the Crisis Into and Opportunity: digital Health
Startegies Deployed During the COVID-19 Outbreak.
JMIR Public Health and Surveillance, 6(2), e19106.
Ragin, C. C. (2006). Set Relations in Social Research:
Evaluation Their Consistency and Coverage. Politica
Analysis, 14(3), 291-310.
Reeves, J., Hollandsworth, H., Torriani, F., Taplizt, R.,
Abeles, S., Tai-Seale, M., Longhurst, C. (2020). Rapid
response to COVID-19: health informatics support for
outbreak management in an academic health system. J
Am Med Inform Assoc., 276, 853-859.
Ricciardelli, A., Manfredi, F., & Antonicelli, M. (2018).
Impacts for implementing SDGs: Sustainable
collaborative communities after disasters. the city of
macerata at the aftermath of the earthquake. Gorporate
Governance (Bingley), 18(4), 594-623.
Rodonjic-Simic, M., Mahrt, C., Niemand, S., Speck, A., &
Windrich, M. (2021). Decentralized open platform for
vaccination—a German example: Covid-19-vacc.
Journal of Open Innovation: Technology, Market, and
Complexity, 7(3), 26 p.
Ross Ashley III, W. (2003). Homeland security: sharing
and managing critical incident information. Teoksessa
C. E., Sensors, and Command, Control,
Communications, and Intelligence (C3I) Technologies
for Homeland Defence and Law Enforcement "ÍI, 6-11.
SPIE.
Sauer, B. A. (2011). Multimodal communication. System
health management: With aerospace applications, 29-
47.
Schofield, P., Shaw, T., & Pascoe, M. (2019). Toward
Comprehensive Patient-Centric Care by Integrating
Digital Health Technology with Direct Clinical Contact
in Australia. J Med Internet Res., 21(6), e12382.
Sentell, T., Foss-Durant, A., Patil, U., Taira, D., Paasche-
Orlow, M., & Trinacty, C. (2021). Organizational
Health Literacy: Opportunities for Patient-Centered
Care in the Wake of COVID-19. Quality Management
in Health Care, 30(1), 49-60.
Shallmo, D., & Williams, C. (2020). Crisis-Driven
Business Model Innovation – Decision-Making Under
Stress. The ISPIM Innovation Conference- Innovating
the Times of Crisis, 12. LUT Scientific and Expertise
Publications.
Shooley, B., Horan, T., & Marich , M. (2014). User
perspectives on the minnesota interorganizational
mayday information system. Information systems for
emergency management, 193-225.
Singh, J., Green, M., Lindblom, S., Reif, M., Thakkar, N.,
& Papali , A. (ei pvm). Telecritical Care Clinical and
Operational Strategies in Response to COVID-19.
Telemedicine and e-Health, 27(3), 261-268.
Smaradottir, B., Fagerlund , A., & Bellika, J. (2020).
Usercentred Design of a Mobile Application for
Chronic Pain Management. Studies in Health
Technology and Informatics, 272-275.
Tahan, H. (2020). Essential Case Management Practices
Amidst the Novel Coronavirus Disease 2019 (COVID-
The Role of Data in Crisis Management Models in the Health Care Context
343

19) Crisis: Part 2. Professional Case Management,
25(5), 267-284.
Tang, Y., Wang, T., Liu, L., Meng, S., & Palanisamy, B.
(2011). Privacy preserving indexing for eHealth
information networks. Proceedings of the 20th ACM
international conference of Information and knowledge
management (CKIM '11), 905-914. New York, NY:
Association for Computing Machinery.
Thye, J., Esdar, M., Liebe, J.-D., Jahn, F., Winter, A., &
Hubner, U. (2020). Professionalism of Information
Management in Health Care: Development and
Validation of the Construct and Its Measurement.
Methods Inf Med, 59(S 01).
Tranfield, D., Denyer, D., & Smart, P. (2003). Towards a
methodology for developing evidence‐informed
management knowledge by means of systematic
review. British Journal of Management, 14(3), 207-
222.
Vedenpää, J., Heikkinen, S., & Grandlund, T. (2020).
Foundations of medical device software cybersecurity
compliance. Whitepaper. Assessed 2. 3 2022
https://hub.solita.fi/foundations-of-medical-device-
software-cybersecurity-compliance.
Vujadinovic, N. (2020). Communication and Public
Relations in Healthcare. Studies in Health Technology
and Informatics: Empowering Public Health, 274, 42-
51.
Vuori V., Helander, N., & Mäenpää, S. (2018). Network
level knowledge sharing: leveraging Riege's model of
knowledge barriers. Knowledge Management Research
& Practice, 17(3), 253-263.
Wybo, J.-L., & Lonka, H. (2003). Emergency Management
and the information Society: How to improve the
synergy? International Journal of Emergency
Management, 12, 183-190.
Zhao, X., Miers, I., Green, M., & Mitrani-Reiser, J. (2019).
Modeling the cybersecurity of hospitals in natural and
manmande hazards. Sustainable and Resilient
Infrastructure, 4(1), 36–49.
KDIR 2022 - 14th International Conference on Knowledge Discovery and Information Retrieval
344
