
Social Determinant of Health for Smoke-Free Homes to Protecting
Children Become Smoker (Passive or Active)
Nur Rohmah
Department of Health Promotion, Faculty of Public Health, Mulawarman University, Samarinda, Indonesia
Keywords: Social Determinant, Smoke-Free Homes.
Abstract: This article is a literature review to design how smoking behavior prevention programs in children who will
become passive smokers or active smokers in the future with a compressive approach from the individual
level, organizational level, and community level. The social, physical, and economic situations in which
people are born, live, work, and age are social determinants of health. Infectious and non-communicable
diseases are affected by social determinants. This article aims to explain why we need to establish a smoke-
free home, as seen from the social determinants of health for smoking, to protect children from becoming
active or passive smokers. The meaning of social determinants and health inequity, based on own knowledge
of smoke-free homes, determines social determinants of health not only from social and health factors but
also from other factors including biology, psychology, economy, and politics. Therefore, social determinants
of health can be determined comprehensively from the environment in which people are born, live, work, and
age.
1
INTRODUCTION
Social determinant of health: a condition in the social,
physical, and economic environment in which people
are born, live, work, and age. Social determinants are
relevant to communicable and non-communicable
diseases. As smoking is an acknowledged risk factor
for a range of chronic diseases, developing
approaches to reduce tobacco use is critical.
Identification of factors associated both with smoking
initiation and cessation may help to underpin
strategies for smoke-free homes.
Various efforts have been made to reduce
smoking behavior, such as the failure to implement
indoor smoking bans (Abramova, Sami, & Huh,
2017), media campaigns (Been et al., 2014), smoking
restriction legislation, and tobacco taxation is among
policies implemented to reduce cigarette smoking
rates. Various factors include the influence of media,
parents, family, friends, and stress (Rohmah, 2013;
Rohman & Psi, 2010; WHO, 2010). Cigarette
initiation is associated with parental smoking and low
levels of maternal education (Conwell et al., 2003).
Why do we care about passive smokers? Because
there is still high smoking at home, the impacts of
cigarette smoke are not only for smokers but also
those around them as passive smokers. The First
effect to physic as second-hand smoke such as lung
cancer (Eng et al., 2014), leukemia (Lee et al., 2009),
malnutrition (Best et al., 2008), asthma, and ear
infection (Hawkins & Berkman, 2011; Wakefield et
al., 2000), increased risk of infant and under-5 child
mortality (Semba et al., 2008), low birth weight (Been
et al., 2014) and allergic (Thacher et al., 2014). The
second effect is psychological, such as depression or
stress (WHO, 2010). The third effect, social norms,
was more important than perceived parental
involvement in explaining cigarette consumption
(Olds & Thombs, 2001). Fathers' warmth and
hostility were the best predictors of heavy smoking
by sons (White, Johnson, & Buyske, 2000). Social
pressure from peers or older siblings has been
considered a prime factor for initial experimentation
(Leventhal & Cleary, 1980).
The meaning of the social determinants and health
inequity is based on knowledge of smoke-free homes
and the determination of social determinants of health
not only from social and health factors but also from
other factors like biology, psychology, economy, and
politics. There comprehensively social determinants
of health can be determined from the environment in
which people are born, live, work, and age.
Rohmah, N.
Social Determinant of Health for Smoke-Free Homes to Protecting Children Become Smoker (Passive or Active).
DOI: 10.5220/0011642400003608
In Proceedings of the 4th International Conference on Social Determinants of Health (ICSDH 2022), pages 147-153
ISBN: 978-989-758-621-7; ISSN: 2975-8297
Copyright
c
2023 by SCITEPRESS – Science and Technology Publications, Lda. Under CC license (CC BY-NC-ND 4.0)
147

This article aims to explain why we need to
establish a home free from cigarette smoke as seen
from the social determinants of health for smoking, to
protect children from active or passive smokers.
2 LITERATURE STUDY
2.1 Theories Conceptual Framework
Social Determinants of Health
The three primary theoretical directions invoked by
current social epidemiologists, are not mutually
exclusive, can be designated as follows: (1)
psychosocial approaches; (2) social production of
disease/political economy of health; and (3) Eco-
social theory and related multi-level frameworks.
These structural determinants are what we include
when referring to the "social determinants of health
inequities." This concept corresponds to Graham's
notion of the "social processes shaping the
distribution" of downstream social determinants. A
comprehensive SDH framework should achieve the
following: (1) Identify the social determinants of
health and the social determinants of inequities in
health; (2) Show how major determinants relate to
each other; (3) Clarify the mechanisms by which
social determinants generate health inequities; (4)
Provide a framework for evaluating which SDH are
the most important to address and (5) Map specific
levels of intervention and policy entry points for
action on SDH. Health inequities flow from patterns
of social stratification—that is, from the
systematically unequal distribution of power,
prestige, and resources among groups in society
(WHO, 2010).
2.2 Application of the Framework to
Smoke-Free Homes in Indonesia
First Section
2.2.1 Socioeconomic and Political Context
(Macro Level)
Socioeconomic approach: smoking is the most
significant avoidable cause of inequalities in health.
Socio-economically disadvantaged people are more
likely to smoke and have started smoking younger
and smoke more heavily than their less disadvantaged
peers. Uptake may also be higher among those with
low socioeconomic status (SES), and quit attempts
are less likely to succeed. Raising the price of tobacco
products appears to be the tobacco control
intervention with the most potential to reduce health
inequalities from tobacco (Hiscock, Bauld, Amos,
Fidler, & Munafò, 2012). The policies of private and
public entities that limit the opportunities of
underprivileged groups are referred to as structural
discrimination. Restriction occurs as a result of
regulations' intentional or unforeseen repercussions,
with examples of structural discrimination emerging
in the context of the tobacco epidemic (Stuber, Galea,
& Link, 2008). The policies of private and public
entities that limit the opportunities of underprivileged
groups are referred to as structural discrimination.
Restriction occurs as a result of regulations'
intentional or unforeseen repercussions, with
examples of structural discrimination emerging in the
context of the tobacco epidemic (WHO, 2010).
Political approach: The regulator of tobacco in
Indonesia was passed in early 2003. The dates during
which it was debated and signed coincided with a
meeting in Geneva of the Intergovernmental
Negotiating Body (INB) of the Framework
Convention on Tobacco Control (FCTC). Thus,
senior Ministry of Health and Food and Drug
Administration representatives involved in tobacco
control issues were not present (Achadi, Soerojo, &
Barber, 2005). Indonesia is the only country in Asia
that refused and did not sign FCTC (Sarvika &
Aditama, 2016). Determination of Non-Smoking
Areas should be held in service facilities for health,
place of the learning process, place child play, place
of worship, public transport, workplace, public
places, and other places designated (Indonesia, 2009).
According to Government Regulation (PP) number
109 2012, The No Smoking Area (KTR) in areas
declared prohibited for activities smoking or
activities producing, selling advertising an promoting
products tobacco (RI, 20Indonesia’snesia tobacco
control regulation passed in 1999, succeeded by
amendments in 2000 and 2003. Today, few
restrictions exist on tobacco industry conduct,
advertising, and promotion in Indonesia (Achadi et
al., 2005).
Cultural and societal Values approach: Cultural
belief, tolerance in indoor smoking (Abramova et al.,
2017), socially unacceptable colludes with patriarchy
(Annandale & Clark, 2000), senior family men's
smoking (Mao, 2014), social acceptance, social
bonding, and tradition (Bush, White, Kai, Rankin, &
Bhopal, 2003) and parental value system (Emory,
Saquib, Gilpin, & Pierce, 2010). Widely cultivated
across Java Indonesia, tobacco was added to the long-
established social habit of chewing betel (Achadi et
al., 2005).
ICSDH 2022 - The International Conference on Social Determinants of Health
148

2.2.2 Socioeconomic Situation and
Structural Determinants (Meso
Level)
a. Increased smoking prevention efforts are
needed in low-SES areas, and limiting
adolescents' pocket money may be an effective
strategy for preventing smoking (Unger, Sun, &
Johnson, 2007). Indonesia's cigarette
expenditure spending in 2017 amounts to
Rp.65,586.00 per day (BPS, 2017). Meanwhile,
the cost of cigarette expenditure on low-income
families in the Samarinda City of Indonesia
amounts to 27.45% (Rp.15,759.00) of
household expenses (Rohmah Nur, 2016).
b. Education
In general, low education makes them lack the
correct health information and information
about the dangers of smoking. Adolescent
cigarette smoking was associated with low
school achievement (Conwell et al., 2003). The
proportion of the population in Indonesia at the
education level of 28,7 % active smoking for
senior high school, no educated 22.8% (RI,
2013).
c. Occupation
in smoker groups mainly from the informal
sector, although not denied from the formal and
professional sector many also become smokers.
However, it is related to family expenditure in
the informal sector because almost 25% is spent
on cigarettes. By type of work,
farmers/fishermen/laborers are the most
significant proportion of active smokers each
day in Indonesia; around 44.5%, 9.9 % of
smokers in the group did not work (RI, 2013).
d. Social class
Widening social class inequalities in smoking
prevalence that members of lower social classes
are increasingly more likely to take up smoking
and less likely to quit (London, 1974). Smoking
behavior spreads through close and distant
social ties. The extent to which smoking
depends on how people are embedded in a social
network and how smoking behavior transcends
direct dyadic ties are not known (Christakis &
Fowler, 2008).
e. Gender and Age
The proportion of the population in Indonesia
aged ≥15 years of male smokers is 67.0% in
2011, to 64.9 % in 2013. More men than female
smokers (47.5% and 1.1%). Similarly,
according to GATS (Global Adult Tobacco
Surveys), female smokers are 2,7% in 2011 and
2.1 % (RI, 2013). The most significant
proportion of active smokers in Indonesia every
day is 30-34 years old, 33.4 %, age 35-39 years
32.2% (RI, 2013). Since starting to smoke at an
early age increases the number of cigarettes
smoked per day in adult life, it is likely to
enhance the risk of tobacco-related diseases. In
Samarinda city Indonesia, early ag start
smoking at four years (Rohmah, 2013).
2.2.3 An Intermediary Determinant
(Individual Level)
Social position determines health through
intermediate factors. Material circumstances,
behavioral and biological variables, and
psychological issues are all intermediate
determinants.
a. Material Circumstances
If a family member (like a father, or grandfather)
smokes at home will result in other family
members becoming passive smokers. This
condition is exacerbated if family members
risks, such as infants, toddlers, pregnant women,
and the elderly.
Data on smoking behavior at home in Indonesia
is 21.2% (RI, 2013), the average family member
stays at home 3.9 persons per household in 2015
(BPS, 2017), and smoking is a lifestyle in
Indonesia (Budiarsih & Ngah, 2017).
b. Behavior and biological factors
Behavior factors such as smoking is an essential
determinant of health. Smoking is generally
prevalent among the lower socioeconomic
group. Risk factors tend to cluster in socially
patterned ways. For example, those living in
adverse childhood social circumstances are
more likely to be low weight and be exposed to
poor diet, childhood infections, and passive
smoking (WHO, 2010).
In Indonesia, daily smokers in urban areas
outnumber those in rural areas by 30.4 percent
and 28.3 percent, respectively. Consuming
tobacco 12.8 pieces per day. Asthma 4.5%, lung
disease 3.7% and cancer 1.4% (RI, 2013).
c. Psychosocial Factors
Psychosocial factors are highlighted by the
psychosocial theory described above. Relevant
factors include stressors (e.g., adverse life
events), stressful living circumstances, and lack
of social support (WHO, 2010). Psychosocial
Social Determinant of Health for Smoke-Free Homes to Protecting Children Become Smoker (Passive or Active)
149
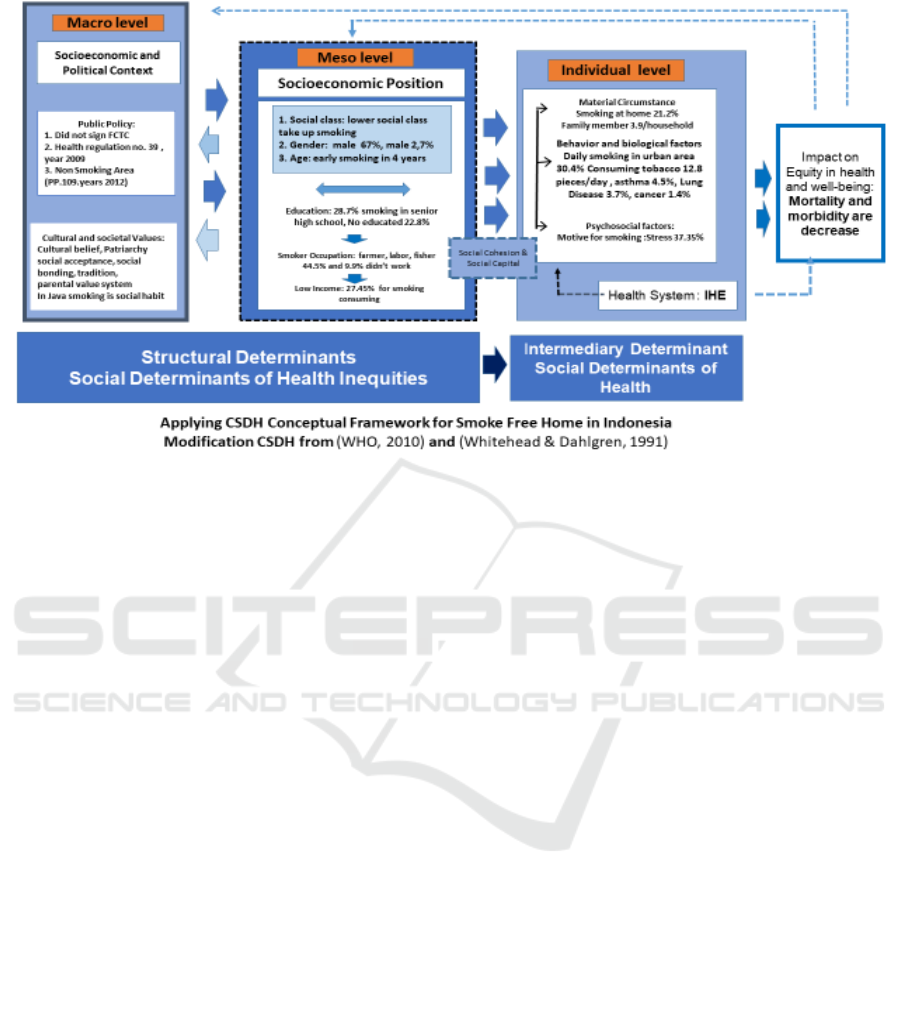
Figure 1: Applying CSDH Conceptual Framework for Smoke-Free Home in Indonesia Modification CSDH from (WHO,
2010) and (Whitehead & Dahlgren, 1991).
variables from adolescence and young
adulthood were significantly distinguished
among empirically identified four trajectory
groups (early stable smokers, late stable
smokers, experimenters, and quitters) (Chassin,
Presson, Pitts, & Sherman, 2000).
Data Smoking in Indonesian motives relieves
tension and stress occupy the highest order,
which is an average of 37,35 % (Rohman & Psi,
2010).
d. Health System
Indonesia's Ministry of Health has a program.
Individual health efforts are any activities
undertaken by the government, society, and the
private sector. To maintain and improve health
and prevent and cure disease and restore health,
individuals include health promotion efforts,
disease prevention, outpatient treatment,
treatment of hospitalization, restriction, and
recovery defects directed against individuals
(Adisasmito, 2007).
e. Impact on equity in health and well-being
Impact on equity in health and well-being, in
particular, moving away from a focus on
physical health status as measured by mortality
and morbidity to encompass, wherever possible,
many other dimensions of health and well-being
(Whitehead, 1991).
3 DISCUSSIONS
Suppose these children, mostly from minority groups
and impoverished families, had no hope for the future
and difference. Would it make if they smoked or used
drugs, missed school, or engaged in violent behavior?
Among smoking households, restriction types varied
according to the number and gender of parents who
smoke. In both smoking and non-smoking
households, children's SHS exposure was directly
related to the type of home smoking restriction, with
the lowest exposures among those reporting full
restrictions (Akhtar, Haw, Currie, Zachary, & Currie,
2009). Although the primary preventive goal should
be to achieve a smoke-free environment, the finding
of an association between early age at the start of
smoking and heavy subsequent cigarette
consumption suggests that additional efforts should
be made to postpone the beginning of smoking among
youngsters (Taioli & Wynder, 1991). By adopting
strong home smoking bans, parents can reduce some
of the influence friends' smoking can have on the
smoking behavior of their adolescents (Szabo, White,
& Hayman, 2006).
Smokers were indistinguishable from non-
smokers in terms of integration in their social
networks. Nevertheless, three decades later,
reflecting significant shifts in societal views of
smoking, smokers were at the periphery of social
ICSDH 2022 - The International Conference on Social Determinants of Health
150
networks and aligned with other smokers
(Bainbridge, Smith, & Barker, 2008).
Based on these cases caused by smoke pollution
cigarettes at homes, need for guidance and
supervision of non-smoking areas in Indonesia. The
need for a set of rules that can support the creation of
a good environment, healthy and free from tobacco
smoke, and the need for guidance and supervision of
a limited region of cigarettes conducted by the City
Health Office Indonesia.
The government is expected to implement KTR
starting from government offices, including the DPR
by giving sanctions to employees who do not comply
with the rules. Smoking is their right, but they also
have to respect the rules for the crowd, that means in
a non-smoking area there is absolutely no smoke, no
cigarette advertisements and no one sells cigarettes, if
it is still fulfilled then sanctions must be imposed,
considering the sanctions this will deter violators. The
scope of the tobacco-free area is regulated in Law No.
36 of 2009 and Government Regulation No. 109 of
2012, among others, the government stipulates that
facilities that are not allowed to smoke are health
service facilities, places of study, places of worship,
public places and other places where smoking is not
permitted. set.
The Ministry of Health (2014) explained that
tobacco product advertisements are targeted at
teenagers, explained that 80% of Indonesian smokers
start smoking before the age of 19 years, the tobacco
industry aggressively targets young people, both
directly and indirectly. Tobacco advertising increases
consumption among children and youth by creating
an environment in which tobacco use is considered
good and regular.
Studies in 102 countries show that a limited ban
on cigarette advertising has little or no effect on
reducing tobacco consumption. Tobacco Control
Support Center Public Health Association of
Indonesia (TCSC-IAKMI) In collaboration with the
Southeast Asia Tobacco Control Alliance (SEATCA)
and the World Health Organization (WHO) Indonesia
reported the four best policy alternatives for tobacco
control, namely raising taxes (65% from retail prices),
prohibiting all forms of cigarette advertising,
implementing 100% non-smoking areas in public
places, workplaces, places of education, as well as
enlarging smoking warnings and adding images due
to smoking habits on cigarette packs.
For the suggested intervention, we will use the
structural intervention to tackle smoke-free homes in
Indonesia can be explained (see. Table 1).
4 CONCLUSION AND
SUGGESTIONS
A summary that the social determinant of health
should be comprehensively determined from various
levels of macro level, meso level, and individual level
so we can determine the determinants of health,
especially for smoking problems at home.
The biased advice presented in this article is that
there needs to be a holistic strategy for protecting
children from exposure to cigarette smoke in the
home environment, institutes, organizations, and
policymakers.
Table 1: Framework to Structural Intervention for smoke-free homes.
Intervention tar
g
e
t
Source of problem Individual-level Or
g
anization level Environment level
Availability Knowledge about smoking and
health, perceived risk of
smoking-related disease, self-
efficac
y
to refuse a ci
g
arette
Local ordinances
require smoke-free
homes.
Regulation selling cigarettes
by retail and not selling
cigarettes for child
Acceptability Picture by sticker do not smoke
at home
Tobacco product
advertising must
have a visual health
warning on the
p
acka
g
e.
Regulation on violence in the
media such as TV does not
show cigarette advertisements
on primetime and limits
b
illboards on the stree
t
Accessibility to smoke-free homes Zoning and timing
regulation to sell
cigarettes.
Prohibition of single
ci
g
arette sales
Community-based initiation by
health volunteers to reduce
smoking at home
Social Determinant of Health for Smoke-Free Homes to Protecting Children Become Smoker (Passive or Active)
151

REFERENCES
Abramova, Z., Sami, M., & Huh, J. (2017). Involuntary
Tobacco Smoking Exposure Among Korean American
Emerging Adults: A Qualitative Study. Journal of
immigrant and minority health, 19(3), 733-737.
Achadi, A., Soerojo, W., & Barber, S. (2005). The
relevance and prospects of advancing tobacco control
in Indonesia. Health policy, 72(3), 333-349.
Adisasmito, W. (2007). Sistem Kesehatan Nasional.
Jakarta: Rajagrafindi Persada.
Akhtar, P. C., Haw, S. J., Currie, D. B., Zachary, R., &
Currie, C. E. (2009). Smoking restrictions in the home
and secondhand smoke exposure among primary
schoolchildren before and after the introduction of the
Scottish smoke-free legislation. Tobacco Control,
18(5), 409-415.
Annandale, E., & Clark, J. (2000). Gender, postmodernism,
and health. Health, medicine, and society: Key theories,
future agendas, 51-64.
Bainbridge, J., Smith, A., & Barker, S. (2008). Stranded in
the Periphery—The Increasing Marginalization of
Smokers. N Engl J Med, 358, 2231-2239.
Been, J. V., Nurmatov, U. B., Cox, B., Nawrot, T. S., van
Schayck, C. P., & Sheikh, A. (2014). Effect of smoke-
free legislation on perinatal and child health: a
systematic review and meta-analysis. The Lancet,
383(9928), 1549-1560.
Best, C., Sun, K., De Pee, S., Sari, M., Bloem, M., &
Semba, R. (2008). Paternal smoking and increased risk
of child malnutrition among families in rural Indonesia.
Tobacco Control, 17(1), 38-45.
Blankenship, K. M., Bray, S. J., & Merson, M. H. (2000).
Structural interventions in public health. Aids, 14, S11-
S21.
BPS. (2017). Laporan Sensus Penduduk 2017. Retrieved
from
Budiarsih, B., & Ngah, A. C. (2017). Role of Law
Influences on Modern Lifestyle Issues In Indonesia and
Malaysia. Scientific Journal of PPI-UKM, 4(1), 18-25.
Bush, J., White, M., Kai, J., Rankin, J., & Bhopal, R.
(2003). Understanding influences on smoking in
Bangladeshi and Pakistani adults: a community-based,
qualitative study. BMJ, 326(7396), 962.
Chassin, L., Presson, C. C., Pitts, S. C., & Sherman, S. J.
(2000). The natural history of cigarette smoking from
adolescence to adulthood in a midwestern community
sample: multiple trajectories and their psychosocial
correlates. Health Psychology, 19(3), 223.
Christakis, N. A., & Fowler, J. H. (2008). The collective
dynamics of smoking in a large social network. New
England journal of medicine, 358(21), 2249-2258.
Conwell, L., O'callaghan, M., Andersen, M., Bor, W.,
Najman, J., & Williams, G. (2003). Early adolescent
smoking and a web of personal and social disadvantage.
Journal of Paediatrics and Child Health, 39(8), 580-
585.
Emory, K., Saquib, N., Gilpin, E. A., & Pierce, J. P. (2010).
The association between home smoking restrictions and
youth smoking behavior: a review. Tobacco Control,
etc. 2010.035998.
Eng, L., Su, J., Qiu, X., Palepu, P. R., Hon, H., Fadhel, E.,
... & Liu, G. (2014). Second-hand smoke as a predictor
of smoking cessation among lung cancer
survivors. Journal of clinical oncology, 32(6), 564-570.
Hawkins, S. S., & Berkman, L. (2011). Increased tobacco
exposure in older children and its effect on asthma and
ear infections. Journal of Adolescent Health, 48(6),
647-650.
Hiscock, R., Bauld, L., Amos, A., Fidler, J. A., & Munafò,
M. (2012). Socioeconomic status and smoking: a
review. Annals of the New York Academy of Sciences,
1248(1), 107-123.
Pemerintah Indonesia. (2009). Undang-uandang No. 36
Tahun 2009 tentang kesehatan. Sekretariat Negara.
Jakarta
Lee, K.-M., Ward, M. H., Han, S., Ahn, H. S., Kang, H. J.,
Choi, H. S., . . . Choi, J.-E. (2009). Paternal smoking,
genetic polymorphisms in CYP1A1, and childhood
leukemia risk. Leukemia Research, 33(2), 250-258.
Leventhal, H., & Cleary, P. D. (1980). The smoking
problem: a review of the research and theory in
behavioral risk modification. Psychological Bulletin,
88(2), 370.
London, J. F. (1974). Smoking behavior and socioeconomic
status: a cohort analysis, 1974 to 1998. Age, 1984, 1998.
Mao, A. (2014). Getting over the patriarchal barriers:
women's management of men's smoking in Chinese
families. Health education research, 30(1), 13-23.
Olds, R. S., & Thombs, D. L. (2001). The relationship of
adolescent perceptions of peer norms and parent
involvement to cigarette and alcohol use. Journal of
School Health, 71(6), 223-228.
Departemen Kesehatan Republik Indonesia. (2013). Riset
kesehatan dasar. Jakarta: Badan Penelitian dan
pengembangan Kesehatan Kementrian Kesehatan RI.
TCSC-IAKMI. 2014. Bunga Rampai : Fakta Tembakau dan
Permasalahannya. Kemenkes RI. Jakarta
Rohmah, N. (2013). Social Learning Theory Application on
Smoking Behavior Junior High School in Samarinda.
Jornal of Sain Learning, 11, No. 4.
Rohmah Nur, R. N., Fitriyana, Exzmy. (2016). Studi
Pengeluaran Biaya Rokok Terhadap Status Gizi Balita
di Kecamatan Samarinda Ulu, Indonesia. Paper
presented at The 3rd Indonesian Conference on
Tobacco or Health 2016, Yogyakarta, Indonesia.
http://ictoh-tcscindonesia.com/the-3rd-ictoh-5/
Rohman, A., & Psi, S. (2010). Hubungan Antara Tingkat
Stres dan Status Sosial Ekonomi Orang Tua dengan
Perilaku Merokok Pada Remaja. Diambil Tanggal, 9.
Sarvika, M. A., & Aditama, Y. M. (2016). Indonesia Jadi
Satu-Satunya Negara di Asia yang Menolak FCTC.
tribunnews. Retrieved from http://bogor.
tribunnews.com/2016/10/02/indonesia-jadi-satu-
satunya-negara-di-asia-yang-menolak-fctc.
Semba, R. D., De Pee, S., Sun, K., Best, C. M., Sari, M., &
Bloem, M. W. (2008). Paternal smoking and increased
risk of infant and under-5 child mortality in Indonesia.
American journal of public health, 98(10), 1824-1826.
ICSDH 2022 - The International Conference on Social Determinants of Health
152

Stuber, J., Galea, S., & Link, B. G. (2008). Smoking and the
emergence of a stigmatized social status. Social science
& medicine, 67(3), 420-430.
Szabo, E., White, V., & Hayman, J. (2006). Can home
smoking restrictions influence adolescents' smoking
behaviors if their parents and friends smoke? Addictive
behaviors, 31(12), 2298-2303.
Taioli, E., & Wynder, E. L. (1991). Effect of the age at
which smoking begins on the frequency of smoking in
adulthood. N Engl J Med, 325(13), 968-969.
Thacher, J. D., Gruzieva, O., Pershagen, G., Neuman, Å.,
Wickman, M., Kull, I., . . . Bergström, A. (2014). Pre-
and postnatal exposure to parental smoking and allergic
disease through adolescence. Pediatrics, 134(3), 428-
434.
Unger, J. B., Sun, P., & Johnson, C. A. (2007).
Socioeconomic correlates of smoking among an
ethnically diverse sample of 8
th
-grade adolescents in
Southern California. Preventive Medicine, 44(4), 323-
327.
Wakefield, M., Banham, D., Martin, J., Ruffin, R., McCaul,
K., & Badcock, N. (2000). Restrictions on smoking at
home and urinary cotinine levels among children with
asthma. American journal of preventive medicine,
19(3), 188-192.
White, H. R., Johnson, V., & Buyske, S. (2000). Parental
modeling and parenting behavior effects on offspring
alcohol and cigarette use: A growth curve analysis.
Journal of substance abuse, 12(3), 287-310.
Whitehead, M. (1991). The concepts and principles of
equity and health. Health Promotion International,
6(3), 217-228.
Whitehead, M., & Dahlgren, G. (1991). What can be done
about inequalities in health? Lancet, 338(8774), 1059-
1063.
WHO. (2010). A conceptual framework for action on the
social determinants of health.
Social Determinant of Health for Smoke-Free Homes to Protecting Children Become Smoker (Passive or Active)
153
