
The Relation Between Heart Failure and Severity COVID-19 Disease
Silmi Kafa Hanifa and Diana Laila Rahmatillah
Faculty of Pharmacy, Universitas 17 Agustus 1945 Jakarta, Indonesia
Keywords: COVID-19, Comorbid Impact, Heart Failure.
Abstract: This study aims to learn the relationship between heart failure and COVID-19 severity. This study aim to
find out is there any correlation between patient with heart failure and COVID-19. This study employed a
retrospective observational cohort research methodology. Analyzing a number of patient medical records
based on preset categories and examining the convenience sampling employed in this study approach
constituted the data collection technique. This research was conducted in one of this hospital in Bekasi. This
study applies several criteria including: A) Inclusion criteria: all patients with heart failure with Covid 19
infection who were treated in the ICU or were not treated in the ICU, and patients aged 18 years or older. B)
Exclusion criteria: pregnant individuals, autoimmune patients and cancer patients. The result of this study
from 150 patient, 80 female and 70 male most of the patients who have confirmed infection with COVID-19
patients with comorbid heart failure generally have a history of hypertension. Cardiovascular damage with
COVID-19 is associated patients with cardiovascular comorbidities are more susceptible to SARS-CoV-2
contamination and may have more extreme clinical symptoms, possibly because of the association with
patients with ACE2 articulation in this collection than patients without cardiovascular comorbidities.
1 INTRODUCTION
Covid-19 is a medical problem brought on by the
SARS-CoV-2 virus. Covid was first discovered in
December 2021 in Wuhan, Hubei Province, China.
SARS- CoV-2 is transmitted from bats (Rhinolophus
hipposideros) to humans via zoonotic transmission.
As of 1 June 2022, the global rate of confirmed
COVID-19 cases has reached over 532 million, with a
death rate of over 6.3 million. Covid-19 manifests
with fever, cough, shortness of breath, diarrhea,
headache, conjunctivitis, sneezing, and loss of smell
and taste (Clekrin, 2020)
Heart disease is prevalent among Covid-19
patients (Ahsan, 2017). Several studies on heart
disease in Covid infection found that the prevalence
of patients with heart disease complications had a
high morbidity rate, and according to some
researchers, heart disease was caused by a variety of
factors, including age, heredity, stress, excessive
alcohol consumption, smoking, and an unhealthy
lifestyle (Iwashima, 2019).
1.1 Covid-19
Covid disease 2019 is an additional intolerable
infection brought on by Severe Acute Respiratory
Syndrome Corona Infection 2 (SARS-CoV-2)
(Jayanama, 2021). Originally, the disease was
known as the 2019 Covid Novel (2019-nCoV).
Coronavirus was identified for the first time in 2019
in Wuhan, Hubei, China (L, 2020). The World
Health Organization declared Covid-19 a pandemic
on March 11, 2022. (Al-Awwal, N, 2020).
Coronaviruses are members of the family
Coronaviradae (Shi, S, 2020). In China, the virus
began to spread between mid-January and late
January (T., Chen, 2020). Covid-19 is a crown-
shaped RNA virus with a diameter between 60 and
140 nanometers. It is transmitted via inhalation,
specifically through coughing and sneezing. By
inhalation, the Covid-19 virus enters the human
nasal system and begins to replicate. Covid-19's
primary receptor is ACE2 Coronavirus, which is
classified as a zoonotic virus, meaning it can be
transmitted from animals to humans (L, 2020)
1.2 Heart Failure
In addition to complications associated with Covid-
19 infection, such as pneumonia, Covid-19 can cause
damage to numerous organs, including the heart
Hanifa, S. and Rahmatillah, D.
The Relation Between Heart Failure and Severity COVID-19 Disease.
DOI: 10.5220/0011978700003582
In Proceedings of the 3rd International Seminar and Call for Paper (ISCP) UTA â
˘
A
´
Z45 Jakarta (ISCP UTA’45 Jakarta 2022), pages 201-205
ISBN: 978-989-758-654-5; ISSN: 2828-853X
Copyright
c
2023 by SCITEPRESS – Science and Technology Publications, Lda. Under CC license (CC BY-NC-ND 4.0)
201
(Shi, S, 2020). In addition to the injuries caused by
Covid-19, many patients have a history of heart
disease prior to contracting the virus, so the
prognosis caused by Covid-19 will have a negative
impact (Wang, T, 2020).
Cardiovascular damage is a condition
characterized by irregularities. in the design or
capacity of the heart that prevents it from working
optimally in that state in all body tissues (Kikuchi, T,
2019). Coronary disease is a disease with a high
mortality and morbidity rate in Indonesia that is on
the rise. CHF (Chronic Heart Failure) causes
aspiration failure, which results in accumulation of
alveolar fluid, and pneumonia caused by Covid-19
disease can also cause accumulation of fluid in the
lungs, which can destroy the estimated Covid-19
contamination. The leading causes are pressure,
heredity, congenital coronary disease, and
cardiomyopathy (Jayanama, K, 2021).
1.3 Role of Heart Failure
Pathophysiology in Covid-19
The renin-angiotensin skeleton (RAS) leads to
cardiovascular disorders such as hypertension, heart
disease, and cardiovascular damage (Zheng, Y,
2020). The SRA comprises of angiotensinogen,
renin, angiotensin II, angiotensin II receptors (AT1
and AT2), and angiotensin- changing over compound
(ACE).
It has been determined that ACE is a compound
that catalyzes the conversion of angiotensin I to
angiotensin II, which is involved in vasoconstriction
and expansion of circulating pressure. Within the
past two decades, a second ACE homologue, ACE2,
has been identified (J. H., 2011). This material is a
counterregulatory chemical that can convert
angiotensin II into vasodilator angiotensin, thereby
reducing the effects of vasoconstriction, sodium
maintenance, and fibrosis.
2 RESEARCH METHODS
This study employed a retrospective observational
cohort research methodology. Analyzing a number
of patient medical records based on preset categories
and examining the convenience sampling employed
in this study approach constituted the data collection
technique.
This study was conducted at Sentra Medika
Cikarang Hospital. The study was conducted from
July through Agust of 2022. A) Inclusion criteria: all
patients with heart failure with Covid 19 infection
who were treated in the ICU or were not treated in
the ICU, and patients aged 18 years or older. B)
Exclusion criteria: pregnant individuals, autoimmune
patients and cancer patients.
2.1 Participant
The participants in this study were 150 patients who
had heart failure and were infected with covid 19,
which was in accordance with the inclusion that had
been set.
2.2 Data Analysis
The result of the research that was carried out at the
sentra medika cikarang hospital, sample taken was
150 patients patients who had heart failure and were
infected with covid 19.
The data was then analyzed in groups using excel
software and then the data was distributed using
SPSS statistical software version 25 to see a relation
between the severity of heart failure patients infected
with Covid-19 with the man withney, chis squared,
the kaplan mayer method
2.3 Instrument
This study uses medical record data patient who had
heart failure and were infected with covid 19 was
150 patients.
2.4 Ethical Approval
Ethical approval was obtained prior to conducting
the study. The ethical approval was sourced from the
health research ethics committee of the Universitas
17 Agustus 1945, Jakarta, with the approval letter
No.39/KEPK- UTA45JKT/EC/EXP/07/2022
3 RESULT
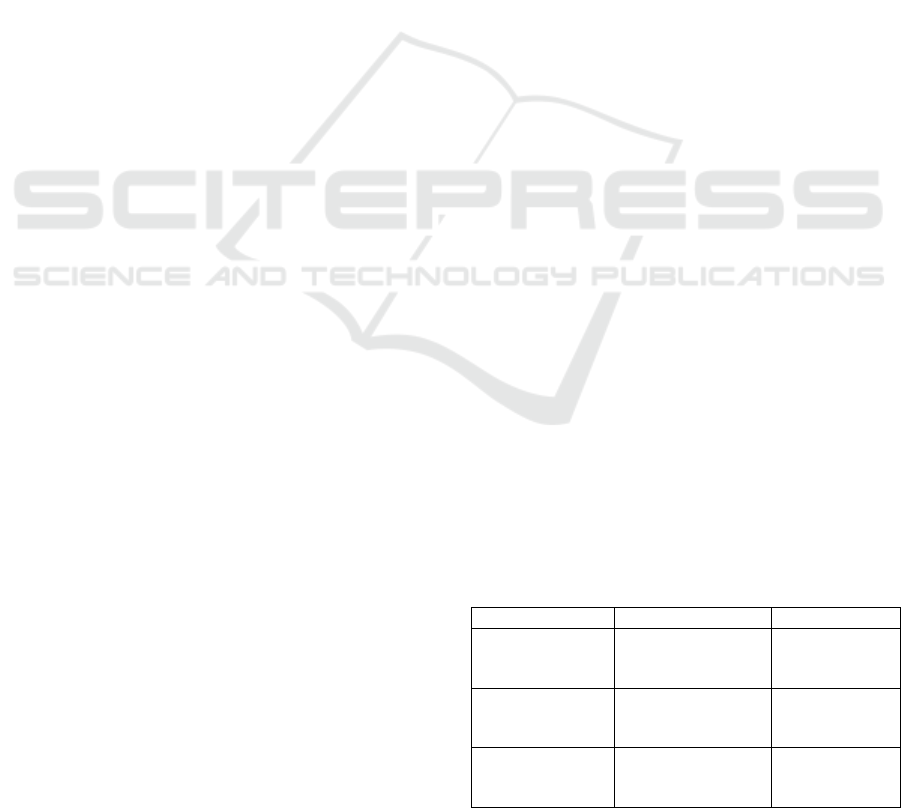
Table 1: Correlation Age and Blood Pressure with Clinical
Outcome.
Facto
r
Mean
p
-value
Age
Survive = 34
(50.67) Dead =
114 (57)
0.0001*
Blood Pressure
Before ICU
Survive = 34
(150.50) Dead
= 114 (149.81)
0.905*
Blood Pressure
After ICU
Survive = 34
(137) Dead = 114
(135.53)
0.951*
* Mann Whitney
ISCP UTA’45 Jakarta 2022 - International Seminar and Call for Paper Universitas 17 Agustus 1945 Jakarta
202
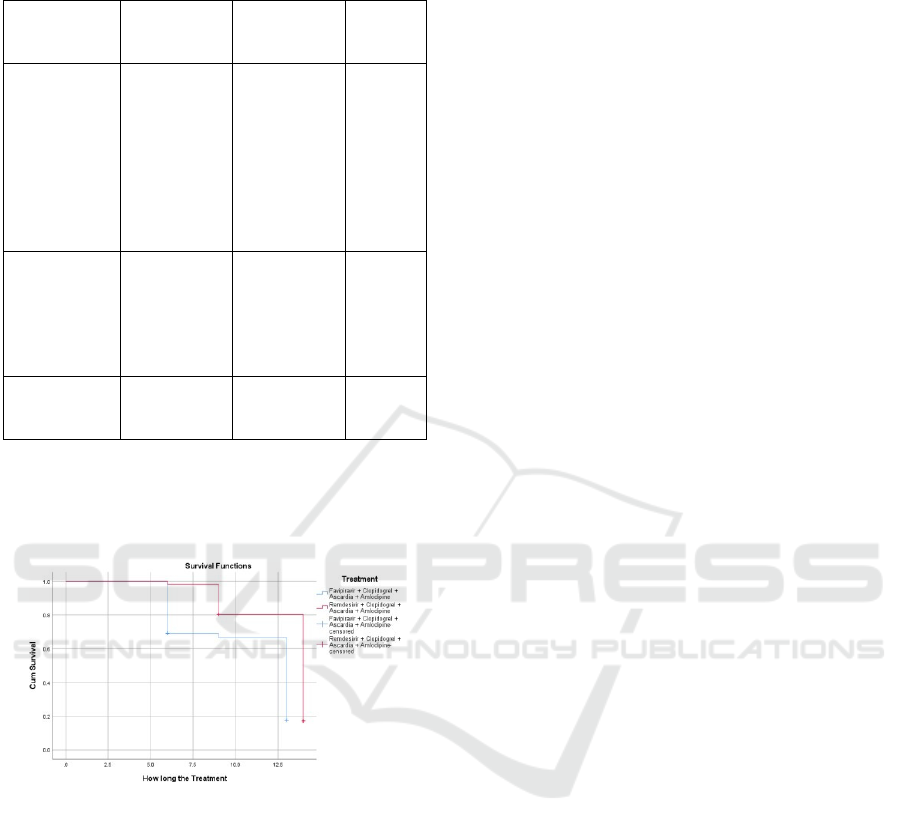
Table 2: Correlation between Diagnosis with Clinical
Outcome.
Factor
Survive (n =
36)
Dead (n =
114)
p-
Value
Comorbidit y
Diabetes = 6
Hypertens
ion = 11
Without
Comorbidit
y = 19
Diabetes = 1
Hypertens
ion = 42
Without
Comorbidit
y = 71
0.002 #
Grade
Moderate =
14 Severe =
10 Critical
illness = 12
Moderate = 8
Severe =
13 Critical
Illness = 93
0.0001 #
CT-Scan
Pile up = 15
Spread = 21
Pile up = 52
Spread = 62
0.705
# Chi-squared
Whitney method to determine the relationship
between age and blood pressure and clinical
outcomes (Pitidhammabhorn, D, 2021).
Figure 1: The Kaplan Meier Survival Analysis.
Frequently, abnormal blood pressure is
connected with the occurrence of heart failure,
which can be deadly, and heart failure is still a
disease with a high mortality rate, heart failure being
comorbid with old age (Micheal, & Ramatillah,
2022). Heart failure is a prime example of a life-
threatening condition that requires rapid medical
assistance and special treatment (Ramatillah, D.L,
2021). Heart failure is the inability of the heart to
properly and adequately pump blood throughout the
body (Ramatillah, D.L, 2021). Significant
correlation (p = 0.0001) Favirapir + Clopidogrel +
Ascardia + Amlodipine (Survive = 25.5%).
Remdesivir + Clopidogrel + Ascardia +
Amlodipine (Survive = 21.4%)
4 DISCUSSION
In examining the association between age and blood
pressure in COVID-19 (Laila, D,2021) patients with
comorbid heart disease, it was discovered that many
patients died due to advanced age and were
susceptible to abnormal blood pressure and
additional comorbidities due to precipitating factors
such as decreased organ function. Who do not
perform well when utilizing the Mann-
In the case of patients with a history of co-
morbid diseases being infected with Covid-19, there
is a strong correlation. Patients with a history of co-
morbid diseases are extremely susceptible to Covid-
19 infection due to a weakened immune system and
a decline in the quality of body organ functions
(King, M, 2012).
Several comorbid disorders, such as
hypertension and diabetes, are frequently observed
in COVID-19-infected patients. Diabetes is a set of
metabolic diseases characterized by hyperglycemia
that results from abnormalities in insulin secretion,
insulin action, or both (Vaduganathan, M, 2020)
Diabetes remains a risk factor for morbidity and
death in COVID-19 patients,yet many people with
diabetes who are infected with COVID-19 are
nonetheless able to survive (Micheal, & ramatillah,
2022), as are Covid-19 patients with a history of
hypertension.
hypertension is high blood pressure and is
indicated by systolic blood pressure > 140 mmHg or
diastolic blood pressure > 90 mmHg (Micheal, &
ramatillah, 2022). The risk of hypertension (Zheng,
Y, 2020) for determining the diagnosis of heart
failure patients infected with COVID-19 has
particular handlers including medical supporting
examinations including CT-scans, ECGs, Swab
tests, PCR, X-rays, blood pressure checks, and blood
sampling examinations (Micheal, & ramatillah,
2022).
From the data obtained, it can be said, "In the
provision of pharmacological therapy in treating
heart failure patients infected with Covid19, the
administration of drug combinations is very
calculated to support the patient's recovery. in the
administration of antiviral,
antiplatelet, calcium channel blockers (CCBS) or
calcium antagonists. favipirafivir and remdasivir are
useful as antivirals for patients with Covid19,
favipirafir is a strong selective inhibitor derived from
favipirafir which is a strong selective inhibitor
derived from influenza virus RNA polymarse and
can enter the viral RNA chains(Shereen, M, 2020)
In patients with the group using favipirafir, it
The Relation Between Heart Failure and Severity COVID-19 Disease
203

showed a shorter treatment period while remdasivir
was useful as an antiviral which had benefits as
clinical manifestations of patients infected with
Covid19, therapy using remdesivir was generally
used in patients with severe categories and several
comorbid diseases (Shereen, M, 2020).
The administration of antiplatelet drugs in heart
failure patients functions as blood thinners based on
data obtained by antiplatelet drugs such as
clopidogrel and ascardia, clopidogrel and ascardia
itself are widely prescribed by doctors as
recommended drugs to function to reduce the risk of
heart attack by thinning the blood and preventing
clotting blood (N, 2020).
Most of the patients who have confirmed
infection with COVID-19 patients with comorbid
heart failure generally have a history of hypertension
(Vaduganathan, M, 2020). As a treatment therapy
patients are given pharmacological therapy with a
calcium channel brocker or calcium antagonist drug
class, the hypertension drug commonly used is
amlodiphine, amlodhipine itself has 2 types of doses,
namely amlodhipine 5 mg and amlodhipine 10 mg,
amlodhipine has a mechanism of action by
inhibiting calcium influxes into smooth muscle cells
in blood vessels and myocardium cells, amlodhipine
is also indicated for the treatment of hypertension
and angina, the effect of giving amlodhipine at the
right dose for patients Hypertension can cause a
decrease in supinated and orthostatic blood
pressure(Micheal, & ramatillah, 2022)
There is an relation between cardiovascular and
COVID-19 adverse events, an association between
patients with cardiovascular comorbidities who are
more immune to disease with SARS-CoV-2 and may
face more extreme clinical adverse events as a result
of association with ACE2 articulation in these
encounters contrasted with patients without
cardiovascular comorbidities
5 CONCLUSION
Due to the uncontrolled pandemic, which has
resulted in a large number of people being affected
by the outbreak, the increase of COVID-19 cases
remains of particular concern to all of us. The case of
the elderly who have been exposed to heart failure
and other comorbidities does not prevent the
possibility of COVID-19 infection.
The association between heart failure and
COVID-19 is dependent on age, therapy provided,
comorbidities, and the severity of COVID-19; age
and therapy are significant determinants in success
and recovery. Doctors prescribe the antiviral
medications favipirafir and remdasivir to patients
with a high risk of death. As well as ascardia and
clopidogrel, amlodhipine is used to control blood
pressure in COVID-19-infected heart failure patients
(N, 2020).
Cardiovascular damage with COVID-19 is
associated, in particular, patients with cardiovascular
comorbidities are more susceptible to SARS-CoV-2
contamination and may have more extreme clinical
symptoms, possibly because of the association with
patients with ACE2 articulation in this collection
than patients without cardiovascular comorbidities
(Jayanama, K, 2021).
The results of this study can be used by further
researchers as research material and a research
reference, as well as a consideration for expanding
further exploration, and I hope that future scientists
will have the choice to make this research more
comprehensive.
REFERENCES
Ahsan, S., & Khan, F. (2017). Physicochemical Properties
and Pharmacology of Amlodipine Besylate: a Brief
Review. Baqai Journal of Health Sciences,
Al-Awwal, N., Dweik, F., Mahdi, S., El-Dweik, M., &
Anderson, SH (2022). A Review of SARS-CoV-2
Disease (COVID-19): Pandemic in Our Time.
Pathogens, 11(3)
Chemotherapy, 55(2), 782–787.
https://doi.org/10.1128/AAC.01219-10
Chen, L., & Hao, G. (2020). The role of angiotensin-
converting enzyme 2 in coronaviruses/influenza
viruses and cardiovascular disease. Cardiovascular
Research, 116(12), 1932–1936.
Clerkin, K. J., Fried, J. A., Raikhelkar, J., Sayer, G.,
Griffin, J. M., Masoumi, A., Jain, S. S., Burkhoff, D.,
Kumaraiah, D., Rabbani, L. R., Schwartz, A., & Uriel,
COVID-19 pneumonia: what has CT taught us? In The
Lancet Infectious Diseases (Vol. 20, Issue 4, pp. 384–
385). Lancet Publishing Group.
https://doi.org/10.1016/S1473- 3099(20)30134-1
Drożdżal, S., Rosik, J., Lechowicz, K., Machaj, F., Kotfis,
K., Ghavami, S., & Łos, M. J. (2020). FDA approved
drugs with pharmacotherapeutic potential for SARS-
CoV-2 (COVID-19) therapy. Drug Resistance
Updates, 53, 100719.
Gee, S., Gaughran, F., MacCabe, J., Shergill, S., Whiskey,
E., & Taylor, D. (2020). Management of clozapine
treatment during the COVID-19 pandemic.
Therapeutic Advances in Psychopharmacology, 10,
204512532092816.
https://doi.org/10.1177/2045125320928167
Geiger, J., Teichmann, L., Grossmann, R., Aktas, B.,
Steigerwald, U., Walter, U., & Schinzel, R. (2005).
ISCP UTA’45 Jakarta 2022 - International Seminar and Call for Paper Universitas 17 Agustus 1945 Jakarta
204

Monitoring of clopidogrel action: Comparison of
methods. Clinical Chemistry, 51(6), 957–965.
https://doi.org/10.1373/clinchem.2004.0470 50
Guan, W., Ni, Z., Hu, Y., Liang, W., Ou, C., He, J., Liu,
L., Shan, H., Lei, C., Hui, D. S. C., Du, B., Li, L.,
Zeng, G., Yuen, K.-Y., Chen, R., Tang, C., Wang, T.,
Chen, P., Xiang, J., ... Zhong, N. (2020). Clinical
Characteristics of Coronavirus Disease 2019 in China.
New England Journal of Medicine, 382(18), 1708–
1720.
Iwashima, Y., Kai, H., Kamide, K., Kanno, Y., Kashihara,
N., Kawano, Y., Kikuchi, T., ... Hirawa, N. (2019).
The Japanese Society of Hypertension Guidelines for
the Management of Hypertension (JSH 2019).
Hypertension Research, 42(9), 1235–1481.
https://doi.org/10.1038/s41440-019-0284-920(2), 27–
31.7. Lee, E. Y. P., Ng, M. Y., & Khong, P. L. (2020).
J. J. V., Pfeffer, M. A., & Solomon, S. D. (2020). Renin–
Angiotensin– Aldosterone System Inhibitors in
Patients with Covid-19. New England Journal of
Medicine, 382(17), 1653–1659.
https://doi.org/10.1056/NEJMsr2005760
Jayanama, K., Srichatrapimuk, S., Thammavaranucupt, K.,
Kirdlarp, S., Suppadungsuk, S., Wongsinin, T.,
Nanthatanti, N., Phusanti, S., Pitidhammabhorn, D., &
Sungkanuparph, S. (2021). The association between
body mass index and severity of Coronavirus Disease
2019 (COVID-19): A cohort study. PLoS ONE, 16(2
Febuary).
https://doi.org/10.1371/journal.pone.0247023
King, M., Kingery, J., & Casey, B. (2012). Diagnosis and
evaluation of heart failure. American Family
Physician, 85(12), 1161– 1168.
L. (2020). A pneumonia outbreak associated with a new
coronavirus of probable bat origin. Nature, 579(7798),
270–273. https://doi.org/10.1038/s41586-020-2012-7
Laila, D., Id, R., & Isnaini, S. (2021). Treatment profiles
and clinical outcomes of COVID-19 patients at private
hospital in Jakarta. 1–11.
https://doi.org/10.1371/journal.pone.0250147
Mendenhall, M., Russell, A., Juelich, T., Messina, E. L.,
Smee, D. F., Freiberg, A. N., Holbrook, M. R., Furuta,
Y., De La Torre, J. C., Nunberg, J. H., & Gowen, B.
B. (2011). T-705 (favipiravir) inhibition of arenavirus
replication in cell culture. Antimicrobial Agents and
Micheal, & ramatillah, D. L., (2022) Treatment profile and
survival analysis acute respiiratory distress syndrome
(ARDS) Covid19 patient International Journal of
Applied Pharmaceutics, 54–56.
https://doi.org/10.22159/ijap.2022.v14s2.447 50
N. (2020). COVID-19 and Cardiovascular Disease. In
Circulation (pp. 1648–1655). Lippincott Williams and
Ramatillah, D. L., & Isnaini, S. (2021). Treatment profiles
and clinical outcomes of COVID-19 patients at private
hospital in Jakarta. Plus one, 16(4), e0250147.
https://doi.org/10.1371/journal.pone.0250147
Shereen, M. A., Khan, S., Kazmi, A., Bashir, N., &
Siddique, R. (2020). COVID-19 infection: Origin,
transmission, and characteristics of human
coronaviruses. In Journal of Advanced Research (Vol.
24, pp. 91–98). Elsevier B.V.
Shi, S., Qin, M., Shen, B., Cai, Y., Liu, T., Yang, F.,
Gong, W., Liu, X., Liang, J., Zhao, Q., Huang, H.,
Yang, B., & Huang, C. (2020). Association of Cardiac
Injury With Mortality in Hospitalized Patients With
COVID-19 in Wuhan, China. JAMA Cardiology, 5(7),
802. https://doi.org/10.1001/jamacardio.2020.0950
Vaduganathan, M., Vardeny, O., Michel, T., McMurray,
Wang, T., Du, Z., Zhu, F., Cao, Z., An, Y., Gao, Y., &
Jiang, B. (2020). Comorbidities and multi-organ
injuries in the treatment of COVID-19. The Lancet,
395(10228), e52. https://doi.org/10.1016/S0140-
6736(20)30558-4Wilkins.
https://doi.org/10.1161/CIRCULATIONAH
Zheng, Y.-Y., Ma, Y.-T., Zhang, J.-Y., & Xie, X. (2020).
COVID-19 and the cardiovascular system. Nature
Reviews Cardiology, 17(5), 259–260.
https://doi.org/10.1038/s41569-020- 0360-5
Zhou, P., Yang, X. lou, Wang, X. G., Hu, B., Zhang, L.,
Zhang, W., Si, H. R., Zhu, Y., Li, B., Huang, C. L.,
Chen, H. D., Chen, J., Luo, Y., Guo, H., Jiang, R. di,
Liu, M. Q., Chen, Y., Shen, X. R., Wa
The Relation Between Heart Failure and Severity COVID-19 Disease
205
