
Resident Safety Culture and Quality of Care in Nursing Homes
Retno Indarwati
a
, Ferry Efendi
b
, Rita Fauiningtyas
c
and Neisya Pratiwindya Sudarsiwi
d
Faculty of Nursing, Universitas Airlangga, Campus C Mulyorejo, Surabaya, East Java 60115, Indonesia
Keyword: Nursing Homes, Resident, Safety Culture, Quality of Care.
Abstract: Nursing home residents are a vulnerable population to treatment errors and incidents. To reduce errors and
incidents, a positive safety culture needs to be established. The study assessed the relationship between safety
culture and quality of care (QOC) in a nursing home of East Java, Indonesia. This cross-sectional study
involved 219 respondents recruited through multistage cluster samplings. This study included 13 nursing
homes: 8 government-owned and 5 private nursing homes. SAQ-INA was used to assess safety culture, and
questionnaires on perceived-based quality of care was used to assess QOC. The data were then analyzed using
table frequencies, descriptive statistics, and the spearman test to determine the relationship between safety
culture and quality of care. Safety culture was found to be significantly related to the quality of care (r =
0.000; p < 0.05). The highest and lowest mean (±SD) scores of safety culture were and quality of care were
55.93±5.844 and 21.50±2.327, respectively. The nursing homes need to improve service quality by increasing
the resident safety through education or training in new staff orientation session.
1 INTRODUCTION
Issues around safety culture of nursing homes receive
little attention. However, several organizations, such
as The Joint Commission and the Institute of
Medicine (IOM), are dedicated to improving patient
safety, making patient safety a top care priority.
Safety culture is an organization’s commitment to
health and safety management based on principles,
behaviors, perceptions, and competencies. A positive
safety culture includes work patterns, effective team
communication, punitive response to mistakes, and
collaborative learning (Castle et al., 2010). Safety
culture plays a vital role in increasing staff awareness
of safety issues, evaluating patient safety
improvements and tracking changes in safety culture
over time (Castle, 2006).
Hospitals are considered having developed safety
culture when achieving better patient outcomes, such
as reduced hospital mortality and provision of
empirical support to implement safety culture.
However, the outcomes are not likely found in less
developed nursing homes. Setting up a safety culture
a
https://orcid.org/0000-0001-7153-9757
b
https://orcid.org/0000-0001-7988-9196
c
https://orcid.org/0000-0002-1948-3909
d
https://orcid.org/0000-0003-0109-2667
in nursing homes is a compliance with the
government regulatory standards and care planning
(Castle et al., 2010). The literature mentions that
nursing homes lack safety control causing some
problems such as drug use and adverse drug events,
high rates of pressure ulcers, inadequate fall risk
management, and ineffective infection control (Li et
al., 2019).
Nursing homes are prone to treatment errors and
adverse events. As the physical ability decreases, the
social roles of the elderly decreases as well, thereby
increasing elderly’s dependence on others (Stone &
Harahan, 2010). Elderly usually require multiple
medications because they have several health
problems including cognitive and sensory
impairments that can lead to an increased risk of
medical errors (Castle et al., 2010). Nursing homes
may not accommodate elderly’s needs as they
experience a high workload, staff turnover,
difficulties in recruiting competent new staff
(Landers et al., 2016), and suboptimal quality of care
(Castle & Ferguson, 2010; Social Welfare Services of
East Java, 2017). In addition, nursing home is
88
Indarwati, R., Efendi, F., Fauiningtyas, R. and Sudarsiwi, N.
Resident Safety Culture and Quality of Care in Nursing Homes.
DOI: 10.5220/0012016300003576
In Proceedings of the 2nd Bali Biennial International Conference on Health Sciences (Bali BICHS 2022), pages 88-91
ISBN: 978-989-758-625-5
Copyright
c
2023 by SCITEPRESS – Science and Technology Publications, Lda. Under CC license (CC BY-NC-ND 4.0)

generally provided by certified nursing assistants who
are not licensed (Arnetz et al., 2011). Most caregivers
in nursing homes are social workers, followed by
nurses and doctors (Edvardsson et al., 2019). Overall,
staffing and demands are very important to consider
for providing health safety in nursing homes.
Achieving a safety culture requires leadership skills
from providers including staff to understand the
organization's values, beliefs, and norms about what
is important and what attitudes and behaviors are
expected (Castle et al., 2010).
Caregivers are human resources for health who,
on the one hand, are the primary supporting agents
focused on the quality of care (QOC). Elderly
satisfaction is the main indicator of service standards
to assess the quality of service provided (QOC). The
attitude of officers will also have an impact on elderly
satisfaction. The elderly needs will increase from
time to time with demands for the quality of care
(QOC). Thus, the elderly might pose subjective value
(perception) of the quality of care (QOC) (Sorra et al.,
2016). Elderly satisfaction with the healthcare service
has emerged as a central concept for orphanage
service management. The goal of a nursing home is
to improve the quality of physical, social, and mental
care with comfort and safety for elderly. Nursing
homes provide elderly with various services that have
been pre-planned and routine. This current study
aimed to assess the relationship between safety
culture and quality of care (QOC) in nursing homes
of East Java, Indonesia.
2 METHODS
This study used a cross-sectional survey design with
219 respondents recruited using multistage cluster
samplings. This study included 13 nursing homes in
East Java: 8 government-owned and 5 private nursing
homes. From July to October 2020, we conducted the
research using the SAQ distributed to caregivers (on
average, 15-20 caregivers per institution). A reminder
one week before the deadline was sent to caregivers
who participated in this study. The completed
questionnaires were returned anonymously in boxes
located in the nursing home ward to ensure
confidentiality. Respondents in this study included
nurses, social workers, security, cleaning services,
kitchen workers, and officers who worked directly
with the elderly.
2.1 Data Collection
The Indonesian version of the Safety Attitudes
Questionnaire (SAQ-INA) was used to assess patient
safety culture. The SAQ-INA was a 14-item
questionnaire which required respondents to rate their
level of agreement on a 5-point scale: 1 = strongly
disagree, 2 = slightly disagree, 3 = neutral, 4 = slightly
agree, and 5 = strongly agree. "Not applicable" was
included as a response category for all questions and
was combined with missing values in the data
analyses. Negative item scores were reversed to
obtain higher scores in the data set, indicating a more
positive evaluation of patient safety culture in nursing
homes. Besides, the Perceived Team-based Quality of
Care (QOC) version was utilized to assess care
quality. The instrument consisted of five items with a
five-point Likert scale from 1 (strongly disagree) to 5
(strongly agree).
2.2 Methods of Data Analysis
For statistical analysis, IBM SPSS Statistics for
Windows, Version 22.0, was used. The population
and patterns of the collected data were described
using descriptive statistics and frequency tables. The
Spearman test was used to examine the relationship
between safety culture and quality of care (QOC).
2.3 Ethical Considerations
This study was based on data on patient safety culture
obtained from nursing homes. It was done under the
National Health Research and Development Ethics
Commission's guidelines. All participants were given
written information about the research objective and
were assured about their data anonymity and
confidentiality. The ethical approval for this study
was obtained from the Commission for Health
Research Ethics, Faculty of Nursing, Universitas
Airlangga (Number of Ethical Approval: 2007-
KEPK).
3 RESULTS
This study included 219 respondents from 13 nursing
homes in East Java, Indonesia. Table 1 shows the
basic characteristics of the respondents. The majority
of respondents (56.2%) are female, and the average
age of nursing home staff workers (28.7%) is between
36 and 45 years old. Medical personnel make up the
majority of jobs (50.75%).
Resident Safety Culture and Quality of Care in Nursing Homes
89
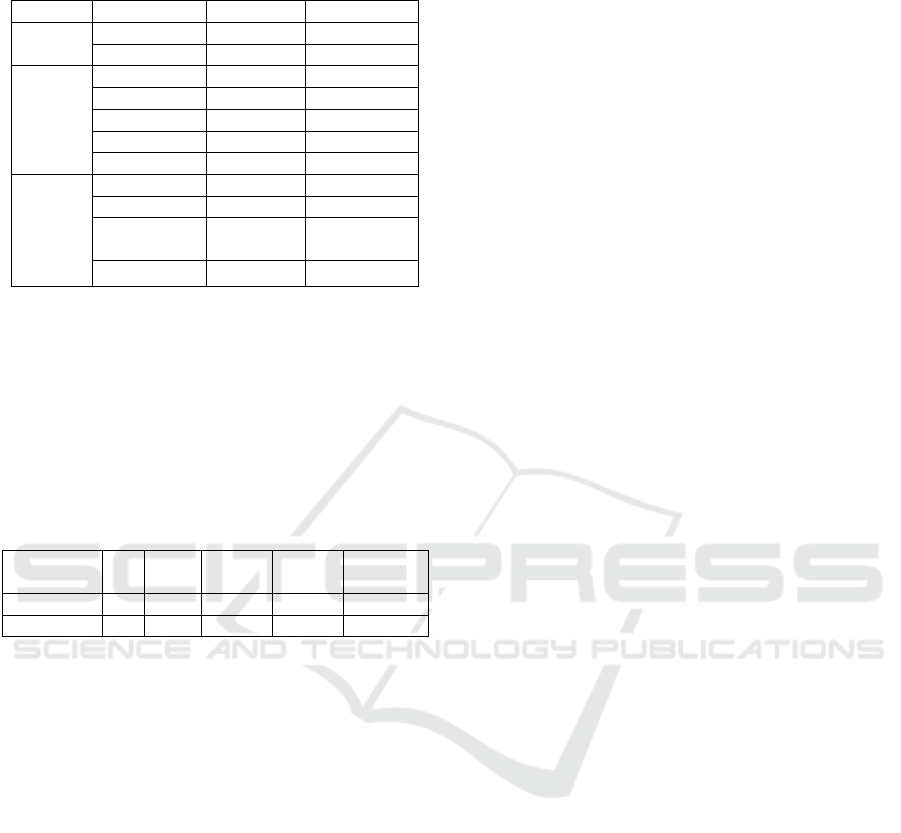
Table 1: Characteristics of 219 caregivers in 13 nursing
homes, East Java, Indonesia.
Numbe
r
Percent (%)
Gender Male 96 43.8
Female 123 56.2
Age
17
–
25 31 14.1
26
–
35 50 22.8
36
–
45 63 28.7
46
–
55 60 27.3
56
–
60 15 6.84
Type
of
work
Medical staff 111 50.7
Mana
g
erial 44 20.0
Supporting
staff
59 26.9
Therapists 5 2.28
Our study showed a significant relationship
between safety culture with quality of care (QOC) in
the nursing homes. Safety culture was significantly
associated with quality of care (r = 0.000; p < 0.05).
The highest and lowest mean (±SD) scores of safety
culture were 55.93±5.844. In addition, the quality of
care had the lowest and highest scores of 21.50±2.327
(Table 2).
Table 2: Descriptive statistics for QOC and SAQ.
N Min Max Mean
Std.
Deviation
PercQOC 219 11 25 21.50 2.327
SAQIna 219 33 70 55.93 5.844
4 DISCUSSION
This study found that patient safety culture had a
significant relationship with quality of care in nursing
homes. A patient safety culture is a commitment to
safety around the healthcare organization. This
includes being willing to discuss procedural errors,
process improvements, and system issues without
fear of repercussions (non-punitive to error) (Sorra et
al., 2016). Safety culture also involves open
communication to prevent recurring adverse events
and develop strategies (Handler et al., 2006). Staffing,
open communication, non-punitive response to
errors, feedback, and communication about errors,
hand-offs and transitions, management support for
patient safety, and organizational learning are all
identified as key measurement domains in patient
safety culture at hospitals.
In a similar domain survey, nursing home staff
(Handler et al., 2006) and administrators (Bonner et
al., 2008) ranked hospital safety culture significantly
lower than the associated groups. Convenient work
environments and communication about patient
safety-related incidents may also contribute to be key
aspects of safety culture in hospital and nursing home
settings (Bonner et al., 2008). Additional aspects,
such as training and skills, teamwork, and adherence
to procedures are significant to identify safety culture
of either hospitals or nursing homes (Teigné et al.,
2019). Adherence to procedures is regarded as critical
for safe work practices (Famolaro et al., 2016).
Creating a patient safety culture could improve
patient safety and quality of care. Assessing key
aspects can be used in patient safety culture
assessment. The need to provide responsive quality
service might be imposed by elderly patients, and thus
speed and readiness of caregivers in dealing with
complaints are important to improve patient safety
culture. Bondevik et al. (2017) discovered that
increasing age and job position are related to patient
safety factors, teamwork climate, safety climate, job
satisfaction, and working conditions. The most
important factor of patient trust is the quality of care
which thus creates customer loyalty and satisfaction.
Patient safety culture is determined by the quality of
service. Hence, the improvement in quality of care
can be measured from to what extent nursing homes
apply patient safety culture (World Health
Organization Europe, 2003). Performance and
service quality will be successful if the customer’s
needs, desires, and expectations are met. This
indicates quality of services has a significant effect on
patient satisfaction (Erdfelder et al., 2009).
5 CONCLUSION
One of the determinants of service quality in nursing
homes is safety culture. This study can provide
nursing homes with the initial information to model
interventions for safety culture, such as improving
working conditions to increase job satisfaction,
lowering the risk of medication-related errors and fall
injuries, and improving quality of communication
among caregivers. A final note is that the nursing
homes need to improve service quality by increasing
their safety culture. More research is needed to study
the relationship between safety culture and other
quality-of-care indicators such as the incidence of
falls, pressure ulcers, malnutrition, injury, and others
.
Bali BICHS 2022 - The Bali Biennial International Conference on Health Sciences
90

ACKNOWLEDGMENTS
The authors would like to thank the Ministry of
Research and Technology for funding this study.
Extensive gratitude was given to Universitas
Airlangga for facilitating the research and all nursing
homes for giving access to data collection in this
study.
REFERENCES
Arnetz, J. E., Zhdanova, L. S., Elsouhag, D., Lichtenberg,
P., Luborsky, M. R., & Arnetz, B. B. (2011).
Organizational climate determinants of resident safety
culture in nursing homes. Gerontologist, 51(6), 739–
749. https://doi.org/10.1093/geront/gnr053
Bondevik, G. T., Hofoss, D., Husebø, B. S., & Deilkås, E.
C. T. (2017). Patient safety culture in Norwegian
nursing homes. BMC Health Services Research, 17(1),
1–10. https://doi.org/10.1186/S12913-017-2387-
9/TABLES/5
Bonner, A. F., Castle, N. G., Perera, S., & Handler, S. M.
(2008). Patient Safety Culture: A Review of the
Nursing Home Literature and Recommendations for
Practice. Ann Longterm Care, 16(3), 18–22.
https://doi.org/10.1109/DEVLRN.2002.1011723
Castle, N. G. (2006). Nurse Aides’ ratings of the resident
safety culture in nursing homes. International Journal
for Quality in Health Care, 18(5), 370–376.
https://doi.org/10.1093/intqhc/mzl038
Castle, N. G., & Ferguson, J. C. (2010). What is nursing
home quality and how is it measured? Gerontologist,
50(4), 426–442. https://doi.org/10.1093/geront/gnq052
Castle, N. G., Wagner, L. M., Perera, S., Ferguson, J. C., &
Handler, S. M. (2010). Assessing Resident Safety
Culture in Nursing Homes: Using the Nursing Home
Survey on Resident Safety. J Patient Saf, 6(2), 59–67.
https://doi.org/10.1016/j.physbeh.2017.03.040
Edvardsson, D., Baxter, R., Corneliusson, L., Anderson, R.
A., Beeber, A., Boas, P. V., Corazzini, K., Gordon, A.
L., Hanratty, B., Jacinto, A., Lepore, M., Leung, A. Y.
M., McGilton, K. S., Meyer, J., Schols, J. M. G. A.,
Schwartz, L., Shepherd, V., Skoldunger, A.,
Thompson, R., … Zúñiga, F. (2019). Advancing Long-
Term Care Science Through Using Common Data
Elements:Candidate Measures for Care Outcomes of
Personhood, Well-Being, and Quality ofLife.
Gerontology and Geriatric Medicine, 5,
233372141984267.
https://doi.org/10.1177/2333721419842672
Erdfelder, E., FAul, F., Buchner, A., & Lang, A. G. (2009).
Statistical power analyses using G*Power 3.1: Tests for
correlation and regression analyses. Behavior Research
Methods 2009 41:4, 41(4), 1149–1160.
https://doi.org/10.3758/BRM.41.4.1149
Famolaro, T., Yount, N. D., Greene, K., Ryan, H., Shakia,
T., & Sorra, J. (2016). AHRQ Nursing Home Survey on
Patient Safety Culture Part I: User Comparative
Database Report.
https://www.ahrq.gov/sites/default/files/wysiwyg/prof
essionals/quality-patient-
safety/patientsafetyculture/nursing-
home/2016/nhsurv16-pt1.pdf
Handler, S. M., Castle, N. G., Studenski, S. A., Perera, S.,
Fridsma, D. B., Nace, D. A., & Hanlon, J. T. (2006).
Patient safety culture assessment in the nursing home.
Quality and Safety in Health Care, 15(6), 400–404.
https://doi.org/10.1136/qshc.2006.018408
Landers, S., Madigan, E., Leff, B., Rosati, R. J., McCann,
B. A., Hornbake, R., MacMillan, R., Jones, K., Bowles,
K., Dowding, D., Lee, T., Moorhead, T., Rodriguez, S.,
& Breese, E. (2016). The Future of Home Health Care:
A Strategic Framework for Optimizing Value. Home
Health Care Management & Practice, 28(4), 262–278.
https://doi.org/10.1177/1084822316666368
Li, Y., Cen, X., Cai, X., & Temkin-Greener, H. (2019).
Perceived Patient Safety Culture in Nursing Homes
Associated with “nursing Home Compare”
Performance Indicators. Medical Care, 57(8), 641–647.
https://doi.org/10.1097/MLR.0000000000001142
Social Welfare Services of Jawa Timur. (2017). Penghuni
Panti Sosial Tresna Werdha (Lanjut Usia) Menurut
Jenis Kelamin, 2004-2016.
Sorra, J., Gray, L., Franklin, M., Streagle, S., Tesler, R., &
Vithidkul, A. (2016). Action Planning Tool for the
AHRQ Surveys on Patient Safety Culture. (Prepared by
Westat, Rockville, MD, under Contract No. HHSA
290201300003C). In Action Planning Tool for the
AHRQ Surveys on Patient Safety Culture. Agency for
Healthcare Research and Quality.
Stone, R., & Harahan, M. F. (2010). Improving the long-
term care workforce serving older adults. Health Aff,
29(1), 109–115.
https://doi.org/10.1377/hlthaff.2009.0554
Teigné, D., Mabileau, G., Anthoine, E., Lucas, M., Leclère,
B., Moret, L., & Terrien, N. (2019). Transcultural
adaptation and psychometric study of the French
version of the nursing home survey on patient safety
culture questionnaire. BMC Health Services Research,
19(1), 1–10. https://doi.org/10.1186/s12913-019-4333-
5
World Health Organization Europe. (2003). WHO Europe
Gerontological Nursing Curriculum. In Geriatric
Nursing.
Resident Safety Culture and Quality of Care in Nursing Homes
91
