
Experience in the Application of GUSS Swallowing Function
Assessment Scale and Self-Rating Masticatory Ability Assessment
Scale for the Elderly People Health Care
Minchuan Huang
1,*
, I Ping Chen
2,*
and Shuying Chung
2
1
School of Computer Science, Guangdong University of Petrochemical Technology, Maoming 525000, China
2
Institute of Nursing College, Central Taiwan University of Science and Technology, Taichung, 406053, Taiwan, China
Keywords:
Gugging Swallowing Screen (GUSS), Swallowing Function, Masticatory Ability, Geriatric Medicine,
Empirical Nursing Care.
Abstract: Elderly people have progressive problems with swallowing function degradation as they get older. The
degradation of swallowing function has a great impact on many living diets in the elderly, which easily causes
body dehydration, nutrition imbalance, with and without susceptibility to aspiration pneumonia, problems
with physiological function, and psychological problems. Common problems, elderly people fear of eating
and drinking due to choking, self-social isolation, pulmonary trachea phlegm and other problems. The elderly
will also have a decreased swallowing function, a reduced oral intake capacity, and a significantly lower
ability to perform activities of daily living. To cite GUSS (gugging swallowing screen) swallowing function
assessment scale and self-rated masticatory ability assessment scale, five elderly people with different age
intervals were selected to implement clinical real-life observation and interview record, according to the
research subjects' self-conscious health and no swallowing function present status, the suggestions and
precautions for planning self-improvement methods.
1 INTRODUCTION
According to Article 2 of the legal database of
Taiwan's elderly welfare law, the age standard of the
elderly is that those over 65 are called old persons
(Balou, 2019; Krishnan, 2020). Many medical studies
have shown that effective and safe swallowing ability
is an important factor in maintaining health and
quality of life. Swallowing function involves a
complex coordination process of psychology, feeling
and motor behavior (Nuchit, 2020; Carnaby, 2020;
Shimizu, 2021; Sasegbon, 2017).
Dysphagia definition: there are problems involving
the mouth, pharynx, esophagus or gastroesophageal
junction in the process of food entering the stomach
from the mouth through chewing. Dysphagia is the
inability to chew food effectively. One or more foods
cannot be safely Swallow into the esophagus.
Uncoordinated breathing and swallowing.
Swallowing activities are divided into oral
preparation stage, oral stage, pharyngeal stage and
esophageal stage according to the location of food. If
there is a problem in any stage that affects eating, it
is also an abnormal phenomenon of swallowing
(Kuramoto, 2020).
Dysphagia in the elderly is the most common and
life-threatening serious problem, such as aspiration
pneumonia, malnutrition, dehydration and so on. In
view of the increasing popularity of chewing and
swallowing difficulties, especially in the elderly of
different ages (e.g. 65, 70, 80 and 90 years old),
chewing and swallowing problems have varying
degrees (Jardine, 2021).
To explore the incidence of dysphagia in the elderly,
research in Taiwan shows that dysphagia affects the
elderly in the community: 15% at the age of 65, 23%
at the age of 70, 16.6% at the age of 70 to 79 and 33%
over the age of 80. Foreign studies have shown that
dysphagia affects elderly patients: 56% to 78% of
hospitalized elderly patients, 47.5% of hospitalized
elderly patients in acute geriatric ward, 30% of stroke
patients, 52% to 82% of patients with Parkinson's
disease, 60% of patients with lateral amyotrophic
sclerosis, 40% of patients with multiple sclerosis and
84% of patients with Alzheimer's disease (Wirth,
2016). The prevalence of pharyngeal disorders in the
Huang, M., Chen, I. and Chung, S.
Experience in the Application of GUSS Swallowing Function Assessment Scale and Self-Rating Masticatory Ability Assessment Scale for the Elderly People Health Care.
DOI: 10.5220/0012018100003633
In Proceedings of the 4th International Conference on Biotechnology and Biomedicine (ICBB 2022), pages 187-191
ISBN: 978-989-758-637-8
Copyright
c
2023 by SCITEPRESS – Science and Technology Publications, Lda. Under CC license (CC BY-NC-ND 4.0)
187
elderly population is high, but it is underestimated
and underdiagnosed. It may increase related
complications, affecting morbidity, length of hospital
stay and medical costs (Khan, 2014).
2 SYMPTOMS AND
EVALUATION OF DYSPHAGIA
Dysphagia symptoms are common in the elderly
(Kahrilas, 1994; Vose, 2018; Ashiga, 2019).
Assessment tools include GUSS (pigging swallowing
screen), SSA (standardized swallowig assessment),
EAT-10 (eating assessment tool), SWAL-QOL
(swallowing quality of life), SPDQ (self-competent
dysphagia questionnaire), self-assessed screening
test for masticatory ability.
2.1
Symptoms of Dysphagia
Symptom observation of clinical nursing: excessive
oral action is required for chewing or swallowing.
Coughing or choking often occurs during or after
eating. Each bite needs to be swallowed two or three
times. There is still a lot of food left on the tongue
after dinner. The food is piled on one side of the
mouth but not consciously. Food falls out during
chewing. Easy to drool, especially during meals.
There is often a large amount of secretion (saliva)
around the mouth. When entering, there will be a
grunt (similar to phlegm sound).
2.2 Key Factors Affecting Swallowing
Function in the Elderly
The physiological changes of aging include muscle
atrophy, decreased tissue elasticity, structural
changes of the cervical spine, decreased saliva and
decreased brain response. The insufficient strength of
the tongue leads to the obstacle of chewing and the
inability to trigger the swallowing reflex in time
(Khan, 2014). Aging causes the decline of oral
sensory function, the decrease of the number of taste
buds and the atrophy of oral mucosa, which affects
the passivation of tongue and lip to spatial touch, the
decrease of oral sense to viscous substances, the
deterioration of body feeling and the dullness of taste
(Youmans, 2006). The slow process of reflection
leads to obvious delay in the transmission and
pushing of food mass, which is easy to cause the
inhalation of foreign bodies and lead to aspiration
pneumonia. The lack of hyoid bone displacement and
the reduction of hyoid bone, epiglottis ligament,
muscle fibres will affect the protective mechanism of
the respiratory tract: aging will affect the as chewing
difficulty or swallowing.
3 CLINICAL SWALLOWING
EVALUATION AND TEST
RESULTS
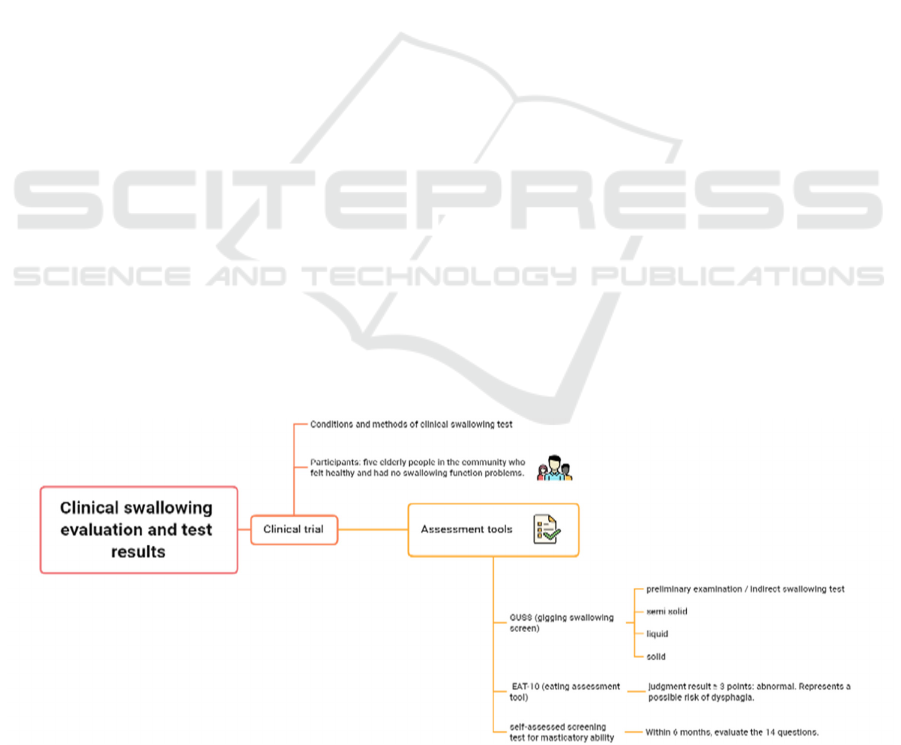
Using GUSS, EAT-10 and Self-assessed screening
test for masticatory ability, five elderly people in the
community were healthy and had no swallowing
problems (Vose, 2018; Molfenter, 2018). Chart of
clinical evaluation and testing is shown in Figure 1.
Figure 1: Chart of clinical evaluation and testing.
ICBB 2022 - International Conference on Biotechnology and Biomedicine
188

3.1 Clinical Trial
Conditions and methods of clinical swallowing test:
the subjects should be awake and can cooperate with
the instructions. Subject SaO2 > 90%, no obvious
respiratory urgency or insufficient vocal cord / throat
function, and no oxygen mask or respirator is
required. The subject had no suspected symptoms of
aspiration pneumonia in the past 3 days. Before the
test, clean the mouth, according to the standard
procedure to avoid choking food / secretions during
the test. First give the subject 3ml of water to drink,
observe whether there is any problem, and repeat the
same step 3 times. If there is no abnormal
swallowing, increase the amount of water tested to 10
ml, 30 ml and 50m in sequence. If the subject will
choke in any process, stop the test and record the
reaction during swallowing. Participants: five elderly
people in the community who felt healthy and had no
swallowing function problems.
3.2 Gugging Swallowing Screen
(GUSS)
Table 1: Indirect swallowing test and direct swallowing
test.
GUSS
(Guggi
ng
Swallo
wing
Screen)
♂96 ♀91 ♂74 ♀84 ♀71
Total
score
20 18 20 17 20
1. ※Sample: add thickeners with one third to half
spoon water (thick as pudding) Ask the patient has
3-5 spoon if without any symptoms, assess after 5
spoons.
2. ※Following 3,5,10,20ml water , continue
with50ml water if without any symptoms, assess
until presence of listed results.
3. ※Clinic: Fibrotic Nasopharyngoscope
swallowing function test: dry bread soaked in color
liquid.
4. ※Use functional examination, such as
swallowing X-ray television fluoroscopy, fiber
Nasopharyngoscope swallowing function
examination.
3.3 Eating Assessment Tool (EAT-10)
Early detection of patients at high risk of swallowing
disorders in order to receive further swallowing
evaluation and swallowing treatment as soon as
possible. A score of 3 or more is dysphagia. The
reliability and validity of eating assessment tool
EAT-10: The Cronbach alpha was 0.960. The
correlation coefficient within the test retest project
ranges from 0.72 to 0.91 (Belafsky, 2008).
Table 2: Assessment of swallowing ability (EAT-10):
within 3 months, 10 questions will be assessed (score
means: 0 is no problem, 4 is serious).
EAT-10
(Eating
Assessment
Tool
)
♂9
6
♀9
1
♂7
4
♀8
4
♀7
1
Total score 1 11 10 5 5
5. ※judgment result ≥ 3 points: abnormal.
Represents a possible risk of dysphagia.
3.4 Self-Assessed Screening Test for
Masticatory Ability
Table 3: self-assessed screening test for masticatory ability.
self-
assessed
screening
test for
masticatory
abilit
y
♂96 ♀91 ♂74 ♀84 ♀71
Total score 3 10 6 10 6
6. ※Within 6 months, evaluate the following 14
questions. Judgment result: some laborious and
unable to eat ≥ 4 kinds.
4 MEDICAL AND NURSING
PROGRAMS
The case receiving process of the empirical study on
oral care for the elderly is divided into seven steps, as
shown in Figure 2. The flow chart of evaluation
empirical research.
Experience in the Application of GUSS Swallowing Function Assessment Scale and Self-Rating Masticatory Ability Assessment Scale for
the Elderly People Health Care
189
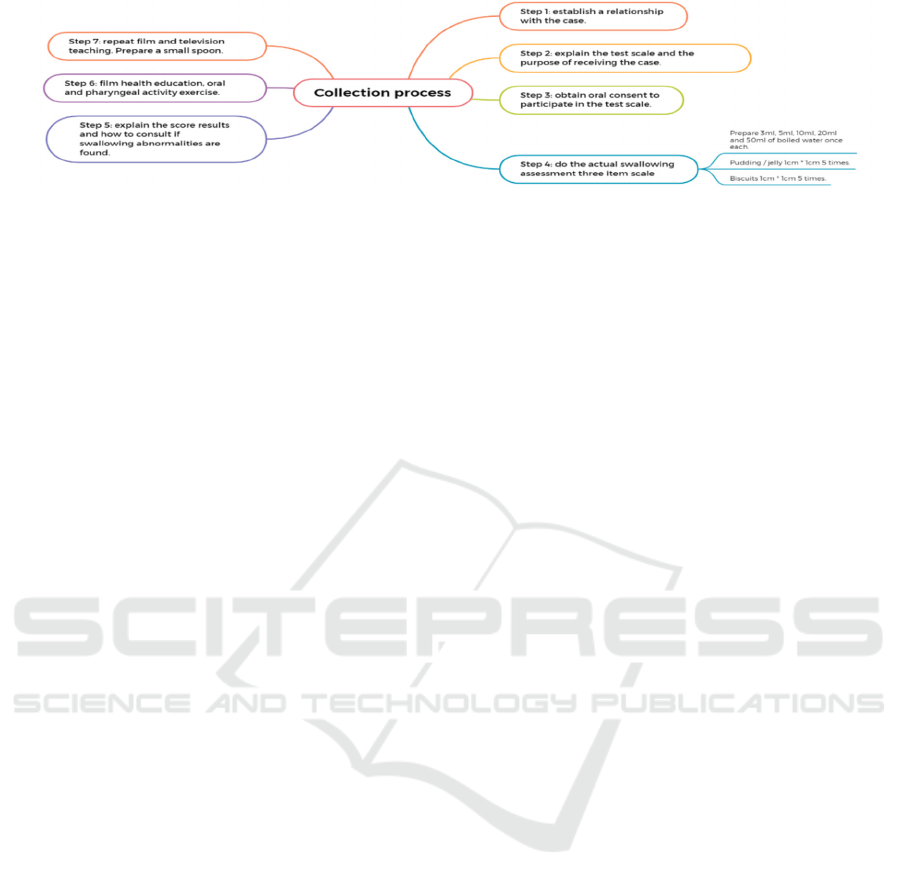
Figure 2: The flow chart of evaluation empirical research.
4.1
Consultation Program for Finding
Dysphagia
Visit a qualified medical institution: evaluation and
referral of rehabilitation department or
Otorhinolaryngology department. Speech therapist
assesses swallowing function. Provide swallowing
training. Swallowing related health education
courses. Radiation therapist if swallowing
photography is required, the radiologist shall assist in
it after being referred by the doctor. Nutritionist a
balanced and complete diet is recommended. Suitable
nutritious food or nutritious fortified food is
recommended.
4.2
Video-Fluoroscopic Swallowing
Study (VFSS)
The golden (best) standard for evaluating patients'
swallowing ability. To confirm the structural and
physiological abnormalities causing the patient's
symptoms. Identify and evaluate the ability and
treatment plans for patients to eat safely and / or
effectively. It needs to be evaluated by the dynamic
image the television fluorescence photography
(VFSS).
4.3
Oral and Pharyngeal Mobility
Exercise
Oral movement control exercise, tongue activity,
exercise, impedance movement, food, ball control
movement, improve the rough movement of getting
objects, the movement of holding close food ball, the
movement of promoting food ball, the activity of
pharyngeal structure, respiratory tract entrance, vocal
cord closure movement, tongue root movement,
laryngeal lifting movement (false voice exercise),
neuromuscular electric stimulation.
Head and neck relaxation exercise: Tilt your head
to the left and right, lower your head and raise your
head. Mouthwash saliva swallowing movement: hold
your left hand flat to rotate next to your left cheek,
and your left cheek is in the shape of mouthwash. Lip,
tongue and tooth movement: extend the tongue to
move left and right. Oral rotation: make a snapping
sound and a lip shape that makes a snapping sound.
5 CONCLUSION
With the deterioration of tongue muscle strength and
the aging of teeth, the diet of the elderly may indeed
bring many difficulties and inconvenience in
chewing and swallowing.
However, with proper maintenance and treatment
of teeth, effective training of tongue muscle strength,
adjustment of food types and selection of suitable
food materials, the elderly can still eat nutritionally
balanced and delicious.
ACKNOWLEDGMENTS
We would like to thank the School of Nursing,
Central Taiwan University of Science and
Technology, the Taichung Blood Donation Center of
the Taiwan Blood Foundation, and Guangdong
University of Petrochemical Technology (Project
Number: 2019rc076 (702-519186, 702-
72100003102)).
REFERENCES
Ashiga, H., Takei, E., Magara, J., Takeishi, R., Tsujimura,
T., Nagoya, K., Inoue, M. (2019). Effect of attention on
chewing and swallowing behaviors in healthy humans.
Scientific Reports, 9(1), 6013.
https://doi.org/10.1038/s41598-019-42422-4
Balou, M., Herzberg, E. G., Kamelhar, D., Molfenter, S. M.
(2019). An intensive swallowing exercise protocol for
improving swallowing physiology in older adults with
radiographically confirmed dysphagia. Clinical
Interventions in Aging, 14, 283–288.
https://doi.org/10.2147/CIA.S194723
ICBB 2022 - International Conference on Biotechnology and Biomedicine
190

Belafsky, P. C., Mouadeb, D. A., Rees, C. J., Pryor, J. C.,
Postma, G. N., Allen, J., Leonard, R. J. (2008). Validity
and Reliability of the Eating Assessment Tool (EAT-
10). Annals of Otology, Rhinology & Laryngology,
117(12), 919–924.
https://doi.org/10.1177/000348940811701210
Carnaby, G. D., LaGorio, L., Silliman, S., Crary, M.
(2020). Exercise-based swallowing intervention
(McNeill Dysphagia Therapy) with adjunctive NMES
to treat dysphagia post-stroke: A double-blind placebo-
controlled trial. Journal of Oral Rehabilitation, 47(4),
501–510. https://doi.org/10.1111/joor.12928
Jardine, M., Miles, A., Allen, J. (2021). Self-reported
Swallowing and Nutrition Status in Community-Living
Older Adults. Dysphagia, 36(2), 198–206.
https://doi.org/10.1007/s00455-020-10125-y
Kahrilas, P. J. (1994). Current investigation of swallowing
disorders. Bailliere’s Clinical Gastroenterology, 8(4),
651–664. https://doi.org/10.1016/0950-
3528(94)90017-5
Khan, A., Carmona, R., Traube, M. (2014). Dysphagia in
the Elderly. Clinics in Geriatric Medicine, 30(1), 43–
53. https://doi.org/10.1016/j.cger.2013.10.009
Krishnan, G., Goswami, S. P., Rangarathnam, B. (2020). A
Systematic Review of the Influence of Bolus
Characteristics on Respiratory Measures in Healthy
Swallowing. Dysphagia, 35(6), 883–897.
https://doi.org/10.1007/s00455-020-10103-4
Kuramoto, N., Ichimura, K., Jayatilake, D.,
Shimokakimoto, T., Hidaka, K., Suzuki, K. (2020).
Deep Learning-Based Swallowing Monitor for
Realtime Detection of Swallow Duration. Annual
International Conference of the IEEE Engineering in
Medicine and Biology Society. IEEE Engineering in
Medicine and Biology Society. Annual International
Conference, 2020, 4365–4368.
https://doi.org/10.1109/EMBC44109.2020.9176721
Molfenter, S. M., Hsu, C.-Y., Lu, Y., Lazarus, C. L. (2018).
Alterations to Swallowing Physiology as the Result of
Effortful Swallowing in Healthy Seniors. Dysphagia,
33(3), 380–388. https://doi.org/10.1007/s00455-017-
9863-6
Nuchit, S., Lam-Ubol, A., Paemuang, W., Talungchit, S.,
Chokchaitam, O., Mungkung, O.-O., … Trachootham,
D. (2020). Alleviation of dry mouth by saliva
substitutes improved swallowing ability and clinical
nutritional status of post-radiotherapy head and neck
cancer patients: a randomized controlled trial.
Supportive Care in Cancer: Official Journal of the
Multinational Association of Supportive Care in
Cancer, 28(6), 2817–2828.
https://doi.org/10.1007/s00520-019-05132-1
Sasegbon, A., Hamdy, S. (2017). The anatomy and
physiology of normal and abnormal swallowing in
oropharyngeal dysphagia. Neurogastroenterology and
Motility: The Official Journal of the European
Gastrointestinal Motility Society, 29(11).
https://doi.org/10.1111/nmo.13100
Shimizu, A., Fujishima, I., Maeda, K., Wakabayashi, H.,
Nishioka, S., Ohno, T., … The Japanese Working
Group On Sarcopenic Dysphagia, null. (2021).
Nutritional Management Enhances the Recovery of
Swallowing Ability in Older Patients with Sarcopenic
Dysphagia. Nutrients, 13(2), 596.
https://doi.org/10.3390/nu13020596
Vose, A. K., Kesneck, S., Sunday, K., Plowman, E.,
Humbert, I. (2018). A Survey of Clinician Decision
Making When Identifying Swallowing Impairments
and Determining Treatment. Journal of speech,
language, and hearing research: JSLHR, 61(11), 2735–
2756. https://doi.org/10.1044/2018_JSLHR-S-17-0212
Wirth, R., Dziewas, R., Beck, A. M., Clave, P., Heppner,
H. J., Langmore, S., … Hamdy, S. (2016).
Oropharyngeal dysphagia in older persons –
from pathophysiology to adequate intervention: a
review and summary of an international expert
meeting. Clinical Interventions in Aging, 189.
https://doi.org/10.2147/CIA.S97481
Youmans, S. R., Stierwalt, J. A. G. (2006). Measures of
Tongue Function Related to Normal Swallowing.
Dysphagia, 21(2), 102–111.
https://doi.org/10.1007/s00455-006-9013-z
Experience in the Application of GUSS Swallowing Function Assessment Scale and Self-Rating Masticatory Ability Assessment Scale for
the Elderly People Health Care
191
