
A Psychobiological Model for the Neurological Symptoms in Somatic
Symptom Disorder
Yutong Xu
Keystone Academy, Beijing 101318, China
Keywords:
Somatic Symptom Disorder, Cause of SSD.
Abstract: Current research lacks in synthesis of psychological and biological approaches when studying the mechanism
of somatic symptom disorder (SSD), which impedes the development of effective treatment intervention.
Primarily due to the conflicting perspectives of the two fields. This paper derived a model that combines both
psychological and biological factors by analyzing literature about factors causing development of SSD. Three
neurological symptoms of SSD were analyzed in this paper (headache, dizziness, and weakness) using 19
pieces of studies. The result shows that the development of SSD follows the path of external stimuli –
physiological change – cognitive processing – response – recurrence. Based on the result, a psychobiological
model of SSD development is established. It will help to find a more precise target for SSD treatment.
1 INTRODUCTION
Although modern medicine has made remarkable
progress in curing diseases over the past century,
there is still a range of symptoms that cannot be fully
resolved. Somatic symptom disorder (hereinafter
referred to as SSD) is a typical category. When
patients report discomfort, but a medical inspection
cannot determine its cause, the complaint may be
ascribed to the psychological status of patients and
diagnosed as SSD. Terms such as somatization,
somatization disorder, somatoform disorder, and
somatization syndrome, have all been used in early
studies to describe SSD. Currently, SSD is defined as
“distressing somatic symptoms plus abnormal
thoughts, feelings, and behaviors in response to these
symptoms” (American Psychiatric Association,
2013). A diagnosis of other medical conditions might
or might not be present for patients with SSD. It is
believed that SSD is caused by the interaction of
biological and psychological factors, but the specific
mechanism behind SSD still needs more
understandings due to the miscellaneous physical
expressions and interlaced causes of SSDs.
The diagnostic criteria of SSD in DSM-V are
shown in Table 1. It was improved from the criteria
in DSM-IV, which attributes SSD mainly to the
psychological factors and suggests that somatic
symptoms of patients are illusions caused by their
mental disorder since their somatic discomfort lacks
medical explanation. According to DSM-V, the
patient’s self-reported somatic distress is real,
regardless of the presence or absence of medical
explanation. Moreover, diagnosis of SSD does not
conflict with other medical diagnoses – in fact, SSD
is usually accompanied by other medical conditions
(American Psychiatric Association, 2013).
Table 1: Diagnostic Criteria of Somatic Symptom Disorder in DSM-V (American Psychiatric Association, 2013).
A. One or more somatic symptoms that are distressing or result in significant disruption of daily life.
B. Excessive thoughts, feelings, or behaviors related to the somatic symptoms or associated health concerns as
manifested by at least one of the following:
1. Disproportionate and persistent thoughts about the seriousness of one’s symptoms.
2. Persistently high level of anxiety about health or symptoms.
3. Excessive time and energy devoted to these symptoms or health concerns.
C. Although any one somatic symptom may not be continuously present, the state of being symptomatic is
persistent (typically more than 6 months).
270
Xu, Y.
A Psychobiological Model for the Neurological Symptoms in Somatic Symptom Disorder.
DOI: 10.5220/0012019500003633
In Proceedings of the 4th International Conference on Biotechnology and Biomedicine (ICBB 2022), pages 270-277
ISBN: 978-989-758-637-8
Copyright
c
2023 by SCITEPRESS – Science and Technology Publications, Lda. Under CC license (CC BY-NC-ND 4.0)

Common symptoms of SSD may be categorized
into 1) pain, 2) neurological symptoms, 3) digestive
symptoms, 4) sexual symptoms (Cleveland Clinic,
2018). Pain has been the most commonly reported
symptom, hence most thoroughly studied by previous
researchers. This paper would therefore discuss the
neurological symptoms of SSD. Neurological
symptoms of SSD include headaches, weakness,
dizziness, and abnormal movements (Cleveland
Clinic, 2018). Compared to localized pain, these
symptoms are non-specific, which means the causes
of these symptoms can be associated with a greater
variety of factors.
As mentioned before, SSD is undeterminable by
objective inspections, psychiatrists have to rely on
self-reported experiences of patients, which makes
diagnosis and treatment of SSD problematic. Due to
the complicated nature of SSD, we need to have a
comprehensive understanding of its causes, so that a
better treatment/prevention of SSD could be
developed. Since SSD is a combination of mental
disorders and medical conditions, it is of concern to
both psychiatrists and physicians. However, because
of the discrepancies between professions, previous
researchers have been using different approaches to
study the causes of SSD – psychological and
biological – which are sometimes disagreeing.
Researchers using psychological approaches
explain the cause of SSD mainly by patients’ mental
processing of information and stimuli. Eifert, Lejuez
and Bouman argued that SSD is caused by
individuals' belief about the threatening outcomes of
physiological changes, which is strongly related to
their past learning, including misinterpretation of
medical information, past experiences, perception of
illness, etc (Eifert, 1998). Witthoft and Hiller added
up to that opinion, suggesting that SSD is caused by
individuals' excessive focus on bodily sensations and
exaggerated illness outcomes and that excessive
focus is primarily due to their neuroticism and
suggestibility (Witthöft, 2010).
Researchers using biological approaches explain
the cause of SSD mainly by patient’s physiological
changes. Rief and Barsky proposed a filter system, in
which they argued that SSD is strongly influenced by
biological factors such as physiological arousal,
endocrine imbalance, neurotransmitter disorder, etc
(Rief, 2005). The individual’s selective attention and
pre-existing mental disorder either made them ignore
the primary physiological signal or over-amplify the
signal, thereby causing the symptoms in SSD.
Dimsdale and Dantzer argued more radically,
suggesting that SSD is probably a misdiagnosis due
to ignorance of patients' history, an unrecognized
disease, or misdiagnosis due to not using modern
diagnostic technology (Dimsdale, 2007).
The disagreement between psychological and
biological approaches is not beneficial for the study
of SSD because a single-factor model is not enough
to induce the developmental path of SSD, which may
have been allowed more precise and effective
treatment interventions. The modern behavioral
medicine approach considered both psychological
and biological factors in the mechanism of SSD by
indicating a mutually reinforcing relationship
between physiological disturbance and emotional
arousal, but the focus was on treatment intervention
(Looper, 2002). The model needs more details on the
mechanism of SSD, as well as more specific
connections to symptoms.
One integrated model was created by Flor,
Birbaumar, and Turk in 1990 for the development of
chronic pain. According to their model, the cause of
chronic pain can be divided into four stages (Flor,
1990):
1. Predisposing factor including genetic defect,
previous social learning, trauma, etc;
2. Precipitating stimuli, which are external and
internal stimuli that arouse discomfort feeling;
3. Precipitating responses, referring to the over-
perception of physical symptoms or inadequate
perception of internal stimuli;
4. Maintaining processes, which are the
conditional learning of pain-related fear and
physiological responses as a result of conditional
learning.
Researchers then suggested: recurring stress and
pain episode leads to increased muscle tension, which
leads to insufficient blood and oxygen in affected
muscles, consequently releasing pain-related
substances, finally resulting in muscular and
sympathetic hyperactivity, thereby forming a vicious
cycle (Flor, 1990).
In this paper, an integrated model for the
development of neurological symptoms in SSD is
established based on literature analysis. This paper
will start by reviewing theories with empirical
supports from both psychological and biological
perspectives, then identify major factors that play a
role in the development of each symptom. Finally, a
general developmental path of neurological
symptoms of SSD will be drawn.
A Psychobiological Model for the Neurological Symptoms in Somatic Symptom Disorder
271

2 METHOD
Literature referenced in this paper is drawn from three
databases (PubMed, UpToDate, and NCBI) by
searching “somatization cause”, “somatoform cause”,
“somatic symptom cause”, “chronic headache”,
“muscle weakness”, and “chronic dizziness”. Papers
are excluded if: (1) irrelated with the cause of SSD;
(2) individual case without other empirical supports;
(3) did not refer to any of the three neurological
symptoms; (4) is specific to a group of patients; (5)
published before 2000. The potential factors causing
the three symptoms are extracted from selected
literature and explained in the following section.
3 RESULTS
3.1 Chronic Headache
3.1.1 Pre-Existing Health Issue
Headache is one symptom of anxiety. As patients
with anxiety demonstrate stress responses and are
more vulnerable to external stimuli. Lindsay Allet
and Rachel Allet stated that anxiety level is widely
recognized in relation to headaches (Allet, 2006).
Shim, Aram Park, and Sung-Pa Park did a statistical
analysis to determine whether alexithymia,
somatization, anxiety and depression are factors
causing chronic headaches (Shim, 2018). They found
that these factors are statistically significant in effect
on headache patients. Anderson, Maes, and Berk
stated that somatic symptoms such as pain and
muscular tension, are major comorbidities of
depression (Anderson, 2012).
3.1.2 Cognitive Processing
Shim, Aram Park, and Sung-Pa Park found that
people with alexithymia are more likely to be
associated with tension-induced chronic headaches
(Shim, 2018). Since alexithymia patients are more
self-affective (Saito, 2016) and hence pay more focus
on their own feeling, a more sensitive perception
toward physical change may be expected, thereby
leading to a more frequent report of headache.
Cappucci and Simons measured anxiety sensitivity by
patients’ self-report and discovered that SSD patients
have high anxiety sensitivity (Cappucci, 2014). They
hypothesized a model that anxiety sensitivity leads to
fear of pain and consequently a stronger experience
of pain-related disability.
3.1.3 External Stimuli
Anderson, Maes, and Berk found that cortisol release
under stress situations may increase mu-opioid
transcription and affect the tryptophan pathway,
tryptophan depletion causes photophobia and
headache (Anderson,, 2012). Espinosa Jovel and
Mejia suggested a causal relationship between
individual hyperexcitability and caffeine intake
(Espinosa, 2017). Moreover, excessive caffeine
intake can result in depression and headaches.
Another group of researchers presented a series of
SSD cases after HPV vaccine injections, which are
speculated to be caused by a sympathetic nervous
system dysfunction stimulated by HPV injection in
the susceptible population (Palmieri, 2016). Although
this phenomenon was observed worldwide, data is
still insufficient to draw a causal relationship between
HPV vaccination and SSD.
3.2 Muscular Weakness (Functional
Weakness)
3.2.1 Pre-Existing Health Issue
Shangguan et al. investigated people who developed
anxiety disorder during the Covid pandemic and
found a statistically significant correlation between
stress and anxiety level, and subjective feeling of
muscular weakness (Shangguan, 2020). Chaturvedi,
Maguire, and Somashekar studied SSD in patients
with cancer. Tiredness, exhaustion, and weakness are
frequently reported. The researchers suggested SSDs
may be the symptom of depression in cancer patients
or side effects of radiation treatment (Chaturvedi,
2006). They also found an association between liver
metastasis (tumor) and weakness. Liver dysfunction
seems to be generally associated with energy levels
(Swain, 2006).
3.2.2 Individual Condition
Shangguan et al. also discovered in their study that
females have a stronger statistical association with
subjective somatic symptoms (Shangguan, 2020).
Stone, Warlow, and Sharpe discovered female gender
dominance in cases of muscular weakness (Stone,
2010).
ICBB 2022 - International Conference on Biotechnology and Biomedicine
272

3.2.3 Cognitive Processing
Stone, Warlow, and Sharpe found patients with
functional weakness tend to think their symptom is “a
mystery” and believe that their symptom is
physiological instead of psychological (Stone, 2010).
Observation of medical management of patients with
functional weakness done by Stone and Carson shows
an improved somatic condition of patients after
changing thinking processes from “the symptom is
devastating” to “the symptom is curable.” (Stone,
2011) The fact that change in cognitive processes can
relieve a patient’s condition shows an important role
played by individuals' cognition in SSD.
3.2.4 External Stimuli
Jotwani and Turnbull introduced some cases
suggesting central neuraxial anesthesia may cause
postoperative weakness because some GABA-
containing sedatives may inhibit certain neural
pathways and lead to the symptoms (Jotwani, 2020).
However, the author mentioned data is insufficient to
draw a conclusion. They also added, in their specific
case, the patient seemed to exhibit an unconscious
stress response, which could result in her somatic
symptom. Lack of vitamin-D intake is also related to
muscle weakness (Dawson-Hughes, 2017) and this
argument was backed up by an experiment done on
mice, which discovers muscle weakness of mice with
vitamin-D receptor removed (Girgis, 2019).
3.3 Chronic Dizziness
3.3.1 Pre-Existing Health Issue
Gupta reviewed past studies on the relationship
between post-traumatic stress disorder (PTSD) and
chronic dizziness (Gupta, 2013). It was concluded by
previous studies that one of the features of PTSD is
sleepiness and partial consciousness, which may be
perceived by individuals as dizziness (Gupta, 2013).
Staab stated a relationship between chronic dizziness
and traumatic brain injury. He introduced that many
patients who had undergone traumatic brain injury
reported “subjective dizziness, imbalance,
hypersensitivity to motion cues.” (Staab, 2006)
Cortese et al. analyzed the DNA of 95 patients with
neurological symptoms of imbalance and dizziness.
They discovered a disordered replication of a DNA
unit named RFC1, leading to ataxia, which causes the
symptoms of dizziness (Cortese, 2020). The patients
usually report neurological symptoms at the sixth
year of the onset of ataxia (Cortese, 2020). Hence,
when investigating SSD, patients' history has to be
taken into account.
3.3.2 External Stimuli
Buzhdygan et al. studied the effect of SARS-CoV-2
spike protein on patients' brain activity and found that
this spike protein can affect the blood-brain barrier
function, causing inflammation in endothelium and
leading to neurological symptoms including chronic
dizziness (Buzhdygan, 2020). Fang et al. analyzed
blood samples of patients with chronic dizziness and
discovered a significantly high level of oxidative
stress parameters and emotional stress-related
neurotransmitters (Fang, 2020). They suggested that
the redox system in SSD patients may be impaired.
4 DISCUSSION
It seems that in all three neurological symptoms of
SSD, the cause, or mechanism, is generally the same
and are interrelated. Four significant factors had been
identified: pre-existing health condition, external
stimuli, cognitive processing, and individual
condition.
4.1 Pre-Existing Condition
Most studies addressed depression and anxiety as the
cause of individuals' strong perception of physical
symptoms. Patients with depression disorder are
featured in decreased interest toward the external
environment and lowered self-esteem (Özen, 2010).
Decreased attention to external stimuli means a
higher level of attention on senses of oneself,
therefore depressive individuals are more likely to
experience and exaggerate somatic symptoms.
Lowered self-esteem means an expectancy of
negative experiences, hence negative physiological
changes are more evident for depressive patients.
Moreover, some depressive patients feel they need
more social attention and caring. When they associate
others' attention with their report of discomfort,
reporting SSD would become a learned behavior.
Individuals with anxiety tend to exhibit unnecessary
thoughts and associate negative consequences with
somatic symptoms (over-interpretation). They were
found to be more often associated with
hypochondriasis (Özen, 2010). Just as Shangguan et
A Psychobiological Model for the Neurological Symptoms in Somatic Symptom Disorder
273

al. discovered, individuals with anxiety tend to
exaggerate and frequently report somatic symptoms
(Shangguan, 2020). Also, panic attacks in anxiety
disorder can directly result in sweating,
lightheadedness, headache, dizziness, weakness,
muscle tension, etc. (Better Health Channel, 2020)
Genetic deficits such as metabolic myopathies (Johns
Hopkins, 2021), which is a decrease in muscle
metabolism, can be also expressed as muscular
weakness. Other pre-existing medical conditions like
PTSD or cancer tumors, as referenced in the last
section, are all potential factors causing the symptoms
of SSD.
4.2 External Stimuli
External stimuli are associated with both
psychological and biological responses. A stress
condition can lead to anxiety response, thus the
release of stress-related chemicals, and the
malfunction of neural pathways in SSD patients. It
could be inferred from Anderson, Maes, and Berk’s
study, the amount of cortisol released by SSD patients
is abnormal because normal cortisol metabolism
would not induce neural pathway dysfunction
(Anderson, 2012). Therefore, it is hard to tell whether
the mental status of SSD patients caused them to
amplify changes brought by external stimuli, or the
biological difference/change in their body reacted to
the external stimuli. Other external stimuli might be
strenuous exercise, cold weather, strong light &
sound stimuli, and sleep deprivation. These factors
can lead to change in blood pressure, muscle
contraction, and vascular contraction, which are all
causes of headache and dizziness.
4.3 Cognitive Processing
When a physiological change is perceived, SSD
patients seem to go through a different cognitive
process, either consciously or unconsciously.
According to the model of Eifert, Lejuez, and
Bouman, past learning would cause the individual to
believe in their “state of being ill” and start to use
their coping skills in response to the external
threatening stimuli (Eifert, 1998). The researchers
suggested that illness belief and coping skills are
safety-seeking behaviors. Intuitively, we have to
focus on the threatening stimulus to ensure we are in
a safe condition, and to respond as quickly as
possible. This probably explains why SSD patients
pay much attention to their somatic feeling. In Stone
and Carson’s case, the SSD patients received
psychological counseling to change their thinking
process (Stone, 2011). Their finding shows that when
SSD patients do not view somatic symptoms as risk
factors, their stress responses are reduced (Stone,
2011). This demonstrates the effect of cognitive
processing on symptoms presented by SSD patients.
4.4 Individual Condition
Every individual is different, both biologically and
psychologically. Gender is a significant factor in
SSD. Female is more susceptible to emotional change
and negative external stimuli, sometimes hold a more
self-focused thinking process (Ingram, 1988). The
premenstrual syndrome was found to be strongly
connected with SSD and alexithymia when appeared
together with depression (Kuczmierczyk, 1995).
Other conditions include social environment, like the
epidemic prevention in the society one’s in during
Covid; education, whether or not one knows SSD or
cognitive process or the physiological change they are
experiencing; immunity; fitness; etc.
4.5 A Psychobiological Model Of SSD
From the analysis of factors, a general development
path of neurological symptoms in SSD can be seen:
I. Individual condition determines the one’s
susceptibility
II. External stimuli incite a physiological change
III. The physiological change combines with
individual’s pre-existing condition (if exists) and
perceived by individual
IV. The cognitive processing of individual
determines the strength of their response (SSD patient
respond strongly due to 1/2/3)
V. Self-pressuring/worrying/prolonged symptom
becomes the new stimuli
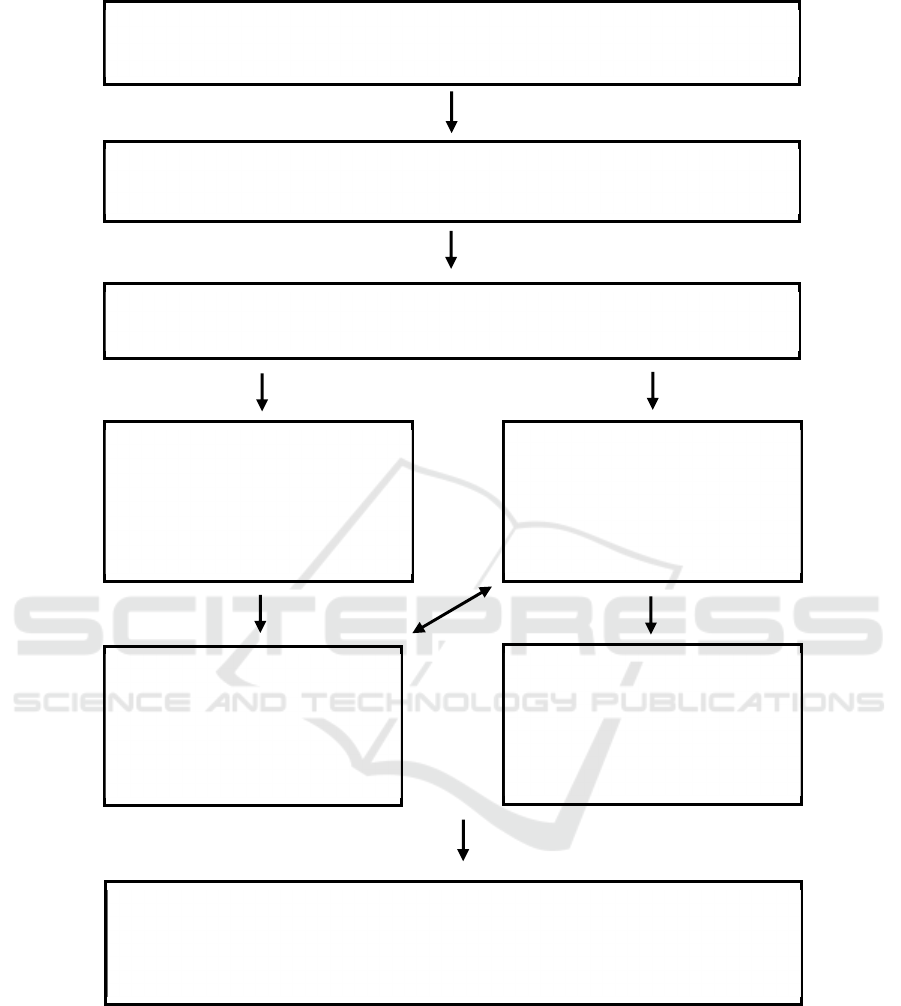
This path is presented visually in Figure 1.
ICBB 2022 - International Conference on Biotechnology and Biomedicine
274
.
Figure 1: Model for Neurological Symptoms Development of SSD.
5 CONCLUSION
In summary, this paper reviewed previous research on
SSD cause and development. This paper found that
external stimuli incite a physical change in SSD
patients, then biological factors, including individual
differences and physical symptoms, are processed by
psychological factors, such as preexisting mental
disorders and cognitive differences, eventually
amplifying patient’s perception of their actual
physical change. This work innovatively considered
three types of factors and combined them into one
model, thereby providing a comprehensive discussion
External stimuli
Exercise, weather change, light, sound, sleep deprivation, medication, etc.
Individual condition
Gender, social environment, education, immunity, fitness, lifestyle, diet, etc.
Physiological change / symptom
Perceive symptom as threat
Pre-existing condition
Depression, anxiety, PTSD, metabolic
myopathies, impaired neural pathway, etc.
Cognitive processing
Past learning, beliefs, social demand,
etc.
(Affected by mental disorders)
Response
Help-seeking behavior, anxiety,
emotional change, sleep change,
hormone imbalance, etc.
Intensified symptom
Or
Increased attention to symptom
Recurring / prolonged symptom
Or
Maintained feeling of the symptom
A Psychobiological Model for the Neurological Symptoms in Somatic Symptom Disorder
275

of SSD development. This work will help researchers
to target a specific point to intervene in disease
development, for example, guide the patient to have
an appropriate cognition of physical discomfort.
Future studies can focus on providing more empirical
support so that a causal relationship between one
factor such as gender, and the response, such as
anxiety, may be derived.
REFERENCES
American Psychiatric Association. (2013). Somatic
symptom and related disorder. In: Robin, L. C. & Scott,
O. L. (Eds.), Diagnostic and statistical manual of mental
disorders: DSM-5 (5th ed., pp. 309–327). essay,
American Psychiatric Association., Washington. pp.
308 – 312.
Anderson, G., Maes, M., & Berk, M. (2012). Inflammation-
related disorders in the tryptophan catabolite pathway
in depression and somatization. Advances in Protein
Chemistry and Structural Biology Volume 88, 27–48.
https://doi.org/10.1016/b978-0-12-398314-5.00002-7
Allet, J. L., & Allet, R. E. (2006). Somatoform disorders in
neurological practice. Current Opinion in Psychiatry,
19(4), 413–420.
https://doi.org/10.1097/01.yco.0000228764.25732.21
Better Health Channel. (2020). Panic Attack. Retrieved
December 1, 2021, from
https://www.betterhealth.vic.gov.au/health/conditionsa
ndtreatments/panic-attack.
Buzhdygan, T. P., DeOre, B. J., Baldwin-Leclair, A.,
Bullock, T. A., McGary, H. M., Khan, J. A., Razmpour,
R., Hale, J. F., Galie, P. A., Potula, R., Andrews, A. M.,
& Ramirez, S. H. (2020). The sars-COV-2 spike
protein alters barrier function in 2D static and 3D
microfluidic in-vitro models of the human blood–brain
barrier. Neurobiology of Disease, 146, 105131.
https://doi.org/10.1016/j.nbd.2020.105131
Cappucci, S., & Simons, L. E. (2014). Anxiety sensitivity
and fear of pain in paediatric headache patients.
European Journal of Pain, 19(2), 246–252.
https://doi.org/10.1002/ejp.542
Chaturvedi, S. K., Peter Maguire, G., & Somashekar, B. S.
(2006). Somatization in cancer. International Review of
Psychiatry, 18(1), 49–54.
https://doi.org/10.1080/09540260500466881
Cleveland Clinic. (2018). Somatic symptom disorder in
adults. Cleveland Clinic. Retrieved December 1, 2021,
from
https://my.clevelandclinic.org/health/diseases/17976-
somatic-symptom-disorder-in-adults.
Cortese, A., Tozza, S., Yau, W. Y., Rossi, S., Beecroft, S.
J., Jaunmuktane, Z., Dyer, Z., Ravenscroft, G., Lamont,
P. J., Mossman, S., Chancellor, A., Maisonobe, T.,
Pereon, Y., Cauquil, C., Colnaghi, S., Mallucci, G.,
Curro, R., Tomaselli, P. J., Thomas-Black, G., … Reilly,
M. M. (2020). Cerebellar ataxia, neuropathy, vestibular
areflexia syndrome due to RFC1 repeat expansion.
Brain, 143(2), 480–490.
https://doi.org/10.1093/brain/awz418
Dawson-Hughes, B. (2017). Vitamin D and muscle
function. The Journal of Steroid Biochemistry and
Molecular Biology, 173, 313–316.
https://doi.org/10.1016/j.jsbmb.2017.03.018
Dimsdale, J. E., & Dantzer, R. (2007). A biological
substrate for somatoform disorders: Importance of
pathophysiology. Psychosomatic Medicine, 69(9),
850–854.
https://doi.org/10.1097/psy.0b013e31815b00e7
Eifert, G. H., Bouman, T. K., & Lejuez, C. W. (1998).
Somatoform disorders. In M. Hersen, & A. S. Bellack
(Eds.), Comprehensive Clinical Psychology (pp. 543 -
565). Pergamon Press.
Espinosa Jovel, C. A., & Sobrino Mejía, F. E. (2017).
Caffeine and headache: Specific remarks. Neurología
(English Edition), 32(6), 394–398.
https://doi.org/10.1016/j.nrleng.2014.12.022
Fang, Z., Huang, K., Gil, C.-H., Jeong, J.-W., Yoo, H.-R.,
& Kim, H.-G. (2020). Biomarkers of oxidative
stress and endogenous antioxidants for patients with
chronic subjective dizziness. Scientific Reports, 10(1).
https://doi.org/10.1038/s41598-020-58218-w
Flor, H., Birbaumer, N., & Turk, D. C. (1990). The
psychobiology of chronic pain. Advances in Behaviour
Research and Therapy, 12(2), 47–84.
https://doi.org/10.1016/0146-6402(90)90007-d
Girgis, C. M., Cha, K. M., So, B., Tsang, M., Chen, J.,
Houweling, P. J., Schindeler, A., Stokes, R., Swarbrick,
M. M., Evesson, F. J., Cooper, S. T., & Gunton, J. E.
(2019). Mice with myocyte deletion of vitamin D
receptor have sarcopenia and impaired muscle function.
Journal of Cachexia, Sarcopenia and Muscle, 10(6),
1228–1240. https://doi.org/10.1002/jcsm.12460
Gupta, M. A. (2013). Review of somatic symptoms in post-
traumatic stress disorder. International Review of
Psychiatry, 25(1), 86–99.
https://doi.org/10.3109/09540261.2012.736367
Ingram, R. E., Cruet, D., Johnson, B. R., & Wisnicki, K. S.
(1988). Self-focused attention, gender, gender role, and
vulnerability to negative affect. Journal of Personality
and Social Psychology, 55(6), 967–978.
https://doi.org/10.1037/0022-3514.55.6.967
Johns Hopkins. (2021). Metabolic myopathy. Johns
Hopkins Medicine. Retrieved December 1, 2021, from
https://www.hopkinsmedicine.org/health/conditions-
and-diseases/metabolic-myopathy.
Jotwani, R., & Turnbull, Z. A. (2020). Postoperative
hemiparesis due to conversion disorder after moderate
sedation: A case report. Anaesthesia Reports, 8(1), 17–
19. https://doi.org/10.1002/anr3.12035
Kuczmierczyk, A. R., Labrum, A. H., & Johnson, C. C.
(1995). The relationship between mood, somatization,
and alexithymia in premenstrual syndrome.
Psychosomatics, 36(1), 26–32.
https://doi.org/10.1016/s0033-3182(95)71704-2
Looper, K. J., & Kirmayer, L. J. (2002). Behavioral
medicine approaches to somatoform disorders. Journal
ICBB 2022 - International Conference on Biotechnology and Biomedicine
276

of Consulting and Clinical Psychology, 70(3), 810–827.
https://doi.org/10.1037/0022-006x.70.3.810
Özen, E. M., Serhadlı, Z. N., Türkcan, A. S., & Ülker,
G. E. (2010). Somatization in depression and anxiety
disorders. Dusunen Adam: The Journal of Psychiatry
and Neurological Sciences, 60–65.
https://doi.org/10.5350/dajpn2010230109t
Palmieri, B., Poddighe, D., Vadalà, M., Laurino, C.,
Carnovale, C., & Clementi, E. (2016). Severe
somatoform and dysautonomic syndromes after HPV
vaccination: Case series and review of literature.
Immunologic Research, 65(1), 106–116.
https://doi.org/10.1007/s12026-016-8820-z
Rief, W., & Barsky, A. J. (2005). Psychobiological
perspectives on Somatoform Disorders.
Psychoneuroendocrinology, 30(10), 996–1002.
https://doi.org/10.1016/j.psyneuen.2005.03.018
Shim, E.-J., Park, A., & Park, S.-P. (2018). The relationship
between alexithymia and headache impact: The role of
somatization and pain catastrophizing. Quality of Life
Research, 27(9), 2283–2294.
https://doi.org/10.1007/s11136-018-1894-4
Saito, N., Yokoyama, T., & Ohira, H. (2016). Self-other
distinction enhanced empathic responses in individuals
with alexithymia. Scientific Reports, 6(1).
https://doi.org/10.1038/srep35059
Shangguan, F., Quan, X., Qian, W., Zhou, C., Zhang, C.,
Zhang, X. Y., & Liu, Z. (2020). Prevalence and
correlates of somatization in anxious individuals in a
Chinese online crisis intervention during covid-19
epidemic. Journal of Affective Disorders, 277, 436–442.
https://doi.org/10.1016/j.jad.2020.08.035
Swain, M. G. (2006). Fatigue in liver disease:
Pathophysiology and clinical management. Canadian
Journal of Gastroenterology, 20(3), 181–188.
https://doi.org/10.1155/2006/624832
Stone, J., Warlow, C., & Sharpe, M. (2010). The symptom
of functional weakness: A controlled study of 107
patients. Brain, 133(5), 1537–1551.
https://doi.org/10.1093/brain/awq068
Stone, J., & Carson, A. (2011). Functional neurologic
symptoms: Assessment and management. Neurologic
Clinics, 29(1), 1–18.
https://doi.org/10.1016/j.ncl.2010.10.011
Staab, J. P. (2006). Chronic dizziness: The interface
between psychiatry and Neuro-Otology. Current
Opinion in Neurology, 19(1), 41–48.
https://doi.org/10.1097/01.wco.0000198102.95294.1f
Witthöft, M., & Hiller, W. (2010). Psychological
approaches to origins and treatments of somatoform
disorders. Annual Review of Clinical Psychology, 6(1),
257–283.
https://doi.org/10.1146/annurev.clinpsy.121208.13150
5
A Psychobiological Model for the Neurological Symptoms in Somatic Symptom Disorder
277
